Abstract
There are no compatible tools that assess bowel function in young children, older children, and adults. This precludes clinical follow-up and longitudinal scientific research. Our aim was therefore to develop and validate a bowel function questionnaire equivalent to the pediatric (8–17 years) and adult (≥ 18 years) Groningen Defecation and Fecal Continence (DeFeC) questionnaires for children from the age of 1 month to 7 years. We developed, validated, and translated the Early Pediatric Groningen DeFeC (EP-DeFeC) questionnaire according to the Consensus-based Standards for the selection of health Measurement Instruments (COSMIN). The EP-DeFeC incorporates different validated bowel function scoring systems, including the Rome IV criteria that are also included in the pediatric and adult DeFeC. We assessed feasibility and reproducibility by a test–retest survey. The study population (N = 100) consisted of the parents/caregivers of children whose median age was 4.0 (IQR 2.0–5.0) years. The mean interval between testing and retesting was 2.7 ± 1.1 months. None of the respondents commented on ambiguities regarding the questions. The overall median time taken to complete the EP-DeFeC was 8.7 min (IQR 6.8–11.8). The overall observed agreement was 78.9% with an overall kappa coefficient of 0.51, indicating moderate agreement.
Conclusion: The EP-DeFeC is a feasible, reproducible, and validated questionnaire for assessing bowel function in children from the age of 1 month to 7 years. If used in combination with its pediatric (8–17 years) and adult (≥ 18 years) equivalents, this questionnaire enables longitudinal follow-up of bowel function from infancy to adulthood.
What is Known: • Bowel function problems are common among young children. • Unfortunately, there are no compatible tools that assess bowel function in young children, older children, and adults, which precludes clinical follow-up and longitudinal scientific research. | |
What is New: • The Early Pediatric Groningen Defecation and Fecal Continence (EP-DeFeC) questionnaire is validated to assess bowel function in children from the age of 1 month to 7 years. • If used together with its pediatric and adult equivalents, longitudinal follow-up of bowel function from infancy to adulthood becomes possible. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bowel function problems are common among children. In general pediatric populations between 0 and 18 years of age, the prevalence rates for functional constipation vary between 1 and 32% [1]. Estimates of the prevalence of fecal incontinence range between 1 and 4% in toilet-trained children [2]. Recently, extensive community studies showed that no less than 3 to 12% of infants and 10 to 19% of toddlers suffer from functional constipation [3, 4]. In these young children, bowel function problems negatively affect their quality of life and lead to considerable health care costs [4,5,6]. This underscores the need for standardized diagnostic tools in young children. Nevertheless, many of the existing bowel function questionnaires are unvalidated, address only one aspect of bowel function, can only be used in a specific setting, or they are designed for older children or adults and thereby excluding younger children and infants. Moreover, in order to compare bowel function at different ages, uniform terminology and scores are required [7]. Unfortunately, there are no compatible tools that assess bowel function in young children, as well as in older children and adults. This impairs clinical follow-up of young children with bowel disorders and longitudinal scientific research of bowel function.
The aim of this study was to develop and validate a detailed bowel function questionnaire for children from 1 month to 7 years of age. The questionnaire had to be equivalent to the pediatric (8–17 years) and adult (≥ 18 years) Groningen Defecation and Fecal Continence (DeFeC) questionnaires [8], to enable longitudinal follow-up of bowel function from infancy to adulthood.
Materials and methods
The questionnaire we developed is equivalent to the Pediatric DeFeC (P-DeFeC) questionnaire for children from 8 to 17 years and the validated adult DeFeC questionnaire for respondents of 18 years and over [8]. We therefore named the newly developed questionnaire the Early Pediatric Groningen Defecation and Fecal Continence (EP-DeFeC) questionnaire. The development, structural validation, and translation of the EP-DeFeC were performed in accordance with the Consensus-based Standards for the selection of health Measurement Instruments (COSMIN) [9, 10]. The study was conducted in compliance with the ethical standards of the Medical Ethical Review Board of University Medical Center Groningen.
Literature search
We conducted a comprehensive literature search of the PubMed, EMBASE, and Cochrane Library databases to identify the existing bowel function scores and definitions for young children up to 7 years of age. The Medical Subject Heading (MeSH) terms we used were as follows: “Child, Preschool,” “Infant,”, “Surveys and Questionnaires,” “Signs and Symptoms, Digestive,” “Fecal Incontinence,” and “Defecation,” which were supplemented by different keywords.
Item selection
The items regarding bowel function that we included in the EP-DeFeC are derived from the Bristol Stool Scale [11], the Rome IV criteria for functional constipation in neonates/toddlers [12] and children [2], the Rome IV criteria for irritable bowel syndrome in children [2], the age-adapted Constipation Scoring System [13], the Obstructed Defecation Syndrome score by Renzi and colleagues [14], the Rome IV criteria for non-retentive fecal incontinence in children [2], the Continence Grading Scale by Jorge and Wexner [15], the Vaizey incontinence score [16], the Pediatric Incontinence/Constipation scores [17], the Holschneider score [18], the Templeton score [19], and Rintala and colleagues’ bowel function score [20]. The EP-DeFeC also contains questions concerning urological functioning based on the standardized definitions of the International Children’s Continence Society [21]. Most of these scoring systems, or their adult equivalents [22,23,24,25,26], were also included in the P-DeFeC and the adult DeFeC, which enables the comparison of bowel function from infancy to adulthood (Fig. 1).
The scoring systems incorporated in all the Groningen Defecation and Fecal Continence (DeFeC) questionnaires. Abbreviations: IBS, irritable bowel syndrome; ICCS, International Children’s Continence Society; ICS, International Continence Society; LARS, low anterior resection syndrome; PICS, pediatric incontinence/constipation score
On account of the early age of the group targeted for the questionnaire, it was unavoidable that the child’s parents or caregivers completed the EP-DeFeC. Therefore, we adapted all the questions to this setting. We are aware that some of the children can read around the age of 5 or 6 years, but we did not want to introduce a selection bias based on the ability of the child to read. Additionally, we designed the EP-DeFeC in such a way that inapplicable questions could be excluded, for example, the exclusion of questions regarding fecal incontinence if the parents or caregivers had indicated that their child was not yet toilet trained.
In developing the EP-DeFeC, we endeavored to adhere as closely as possible to the format of the existing P-DeFeC and adult DeFeC questionnaires (Table 1) [8]. Thus, the EP-DeFeC consisted of eight categories: personal details, defecation pattern, constipation, constipation-related questions, fecal continence, urge, urinary continence, and medical history. We did not include questions from the P-DeFeC and adult DeFeC that did not apply to children between 1 month and 7 years of age, such as residential information, educational level, work, and obstetric/gynecological medical history. On the contrary, we added additional age-related questions to the EP-DeFeC, such as a preterm birth and type of feeding (Table 1).
Pilot testing
We sent the first draft of the EP-DeFeC to a Delphi panel consisting of pediatricians, pediatric surgeons, pediatric gastroenterologists, pediatric physiotherapists, and specialized pediatric nurses. They were specifically asked to provide feedback on completeness, relevance, redundancy, and/or the wording of the questions and to test the content validity of the questionnaire [9, 10]. All remarks were discussed and incorporated in the second draft of the EP-DeFeC.
Feasibility
The second draft of the EP-DeFeC was distributed randomly among native Dutch-speaking parents with various levels of education who had children aged between 1 month and 7 years. The parents were asked to read the questionnaire thoroughly and to mention any ambiguous questions or answer options. After the pilot testing was completed, the problems raised by the parents were discussed and revised. This resulted in the definitive version of the EP-DeFeC, which consisted of 75 questions (Online Resource 1).
Reproducibility and reliability
We performed a test–retest survey to determine the reproducibility of all questions and the reliability of the different scoring systems in the EP-DeFeC. We invited a randomly selected sample of Dutch parents of children between 1 month and 7 years of age to complete the EP-DeFeC. All participants were recruited by an external survey company (Dynata, Rotterdam, the Netherlands) from all regions of the Netherlands. Respondents were asked to complete the EP-DeFeC again after approximately 3 months. This time interval was chosen to ensure that the test–retest interval was long enough to prevent recall but short enough that the likelihood of major changes in the respondent’s circumstances was minimal, according to the COSMIN principles [9]. The respondents were not initially informed about the fact that they would be asked to complete the questionnaire again. We also assessed how long it took to complete the questionnaire. We excluded respondents who reported a different date of birth and/or sex of their child on the test and retest forms, which rendered these questionnaires invalid. All questionnaires were completed digitally, with the obligation to complete all applicable questions before submitting the questionnaire.
Translation
The final EP-DeFeC was translated from Dutch into English. In accordance with the COSMIN principles, the translation was performed by two independent professional translators who were naive as to the topic [9]. One translator translated the questionnaire into English and the other translated the questionnaire back into Dutch. Discrepancies between the translations were discussed and resolved in the final English version of the EP-DeFeC.
Statistical analysis
Descriptive statistics on personal characteristics and the time required to complete the questionnaire are shown as mean ± SD or median (IQR), depending on their distribution. Categorical variables are shown as number (percentage). We calculated the percentage of observed agreement for all categorical and dichotomous questions. We evaluated the reproducibility of all questions by calculating the unweighted kappa coefficient for the questions with dichotomous answer options and the weighted Cohen kappa coefficient for the questions with multiple, ordinal answer options. To examine the reproducibility of the scoring systems, the unweighted kappa coefficient was determined for the scoring systems with a dichotomous outcome. The reliability of the continuous scoring systems was expressed as intraclass correlation coefficient (ICC). All kappa coefficients and ICC values were interpreted according to Landis and Koch—values between 0.01 and 0.20 were considered slight agreement, values between 0.21 and 0.40 as fair agreement, values between 0.41 and 0.60 as moderate agreement, values between 0.61 and 0.80 as substantial agreement, and values between 0.81 and 1.00 as almost perfect agreement [27]. All analyses were performed with SPSS software, Version 23.0 (Armonk, NY, USA: IBM Corp), and the image was created with Biorender.com.
Results
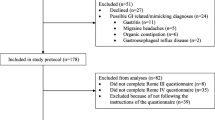
A total of 124 parents of children between 1 month and 7 years of age completed the test and retest of the EP-DeFeC without any missing values. We excluded 24 of these respondents because the date of birth and/or sex of the child between the test and retest did not match. The children of the 100 included respondents had a median age of 4.0 (IQR 2.0–5.0) years, and 57% of them were boys. The mean time interval between the test and retest was 2.7 ± 1.1 months. The mean time interval between the test and retest was not significantly different between infants/toddlers and older children (2.5 versus 2.9 months, p = 0.092).
Feasibility
None of the respondents commented on ambiguities regarding any of the 75 questions of the final EP-DeFeC. The overall median time to complete the EP-DeFeC was 8.7 min (IQR 6.8–11.8, Table 2). Parents of a child who always wore a diaper took a median of 7.9 (IQR 5.9–9.9) minutes to complete the EP-DeFeC. Parents of a child who had just started toilet training or who was fully toilet trained spent a median of 9.5 (IQR 8.8–13.5) and 9.0 (IQR 7.3–12.2) minutes, respectively, to complete the EP-DeFeC (Table 2).
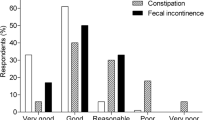
Reproducibility of all questions of the EP-DeFeC
The percentage of observed agreement of the questions in every category of the EP-DeFeC ranged between 67.7 and 91.8%, with mean kappa coefficients between 0.38 and 0.60 (Table 3). All categories except defecation pattern showed moderate or substantial agreement. The overall observed agreement of the EP-DeFeC was 78.9%, with an overall kappa coefficient of 0.51, indicating moderate agreement (Table 3). The overall observed agreement and overall kappa coefficient were not different between infants/toddlers and older children (Online Resource 2).
Reliability of the incorporated scoring systems of the EP-DeFeC
The kappa coefficients of the dichotomous scores and the intraclass correlation coefficients of the continuous scores ranged between 0.34 and 0.91 (Table 4). The majority of the incorporated scoring systems showed almost perfect agreement. The percentage of observed agreement of the continuous scores ranged between 89.1 and 96.4% (Table 4A). The unweighted kappa coefficient for the Rome IV criteria of functional constipation for neonates/toddlers was 0.65 (95% CI, 0.20–1.10), for the Rome IV criteria of functional constipation for children 0.47 (95% CI, 0.05–0.89), for the Rome IV criteria for irritable bowel syndrome for children 0.85 (95% CI, 0.65–1.05), and for the Rome IV criteria for non-retentive fecal incontinence for children 0.34 (95% CI, − 0.07–0.75, Table 4A). The mean intraclass correlation coefficient for all continuous scores for fecal incontinence was 0.87, including the Continence Grading Scale, the Vaizey Continence score, the Holschneider score, the Templeton score, and the PICS incontinence score (Table 4B). This indicates an almost perfect overall agreement for the continuous scores for fecal incontinence. For the continuous scores for constipation, the mean intraclass correlation coefficient was 0.71, including the Constipation Scoring System, the Renzi score, and the PICS constipation score (Table 4B). This indicates a substantial overall agreement for the continuous scores for constipation.
Discussion
We developed the EP-DeFeC questionnaire to assess the bowel function of children between 1 month and 7 years of age (Online Resource 1). Overall, the EP-DeFeC was found to be reproducible and structurally valid in Dutch children of this age.
The EP-DeFeC incorporates various existing, well-known bowel function scores and definitions, such as the Rome IV criteria for functional constipation, the PICS incontinence and constipation scores, the Jorge-Wexner score, and many others (Fig. 1) [2, 11,12,13,14,15,16,17,18,19,20]. Both constipation and fecal incontinence are addressed by the EP-DeFeC as these conditions often go together in children [17, 28]. The bowel function scores facilitate the clinical interpretation of the questionnaire, because only counting fecal incontinence episodes or knowing stool frequency does not necessarily differentiate between children with acceptable bowel function and those in need of medical attention. Moreover, the incorporated validated bowel function scores and definitions for constipation and fecal incontinence also benefit the application of the EP-DeFeC for scientific research purposes. The scientific use of the EP-DeFeC is also supported by the fact that the questionnaire incorporates almost all aspects of the core outcome set for childhood constipation [29].
Most of the incorporated bowel function scores [2, 11,12,13,14,15,16,17,18,19,20,21], or their adult equivalents [22,23,24], are also present in the P-DeFeC and adult DeFeC. Therefore, subsequent use of the EP-DeFeC (1 month to 7 years), P-DeFeC (8 to 17 years), and adult DeFeC (18 years and over) enables follow-up of bowel function from infancy to adulthood. To the best of our knowledge, the series of DeFeC questionnaires is the first tool developed specifically to determine the course of bowel function problems from infancy to adulthood effectively, using validated scoring systems and definitions. The follow-up of bowel function over time will add to our knowledge of the physiological development of bowel function from early childhood to adulthood. Furthermore, the tool can be used to illustrate the course of distinct aspects of the bowel function during the clinical follow-up of young children with bowel disorders, such as Hirschsprung disease and congenital anorectal malformations.
Although bowel function is the main topic of the EP-DeFeC, additional questions about sex, preterm birth, diet, therapies, medical history, and familial medical history are included. Previously, these factors were associated with bowel function [1, 3, 5, 30, 31]. Furthermore, the EP-DeFeC also includes urological questions, because it is known that children often suffer from concomitant bladder and bowel dysfunction [32]. These additional questions make the EP-DeFeC a feasible tool to screen for coexisting and/or causative factors of the detected bowel function problems. Therefore, the answers provided in the EP-DeFeC questionnaire may indicate the need for drug therapy, dietary advice, and/or bowel training programs.
The development and testing of the EP-DeFeC among a diverse sample of respondents adds to its applicability. We distributed the questionnaire among Dutch parents with young children from all regions within the Netherlands and with various educational levels. Furthermore, the feasibility analysis shows that the EP-DeFeC is usually quick and easy to complete. The fact that inapplicable parts of the EP-DeFeC can be excluded may have added to its feasibility in this young age group with a large physiological variation in bowel function. Hopefully, the short time to complete the EP-DeFeC may stimulate its use prior to appointments with a health care provider, at home, or even in the waiting room. Additionally, the EP-DeFeC has been officially translated from Dutch into English and German, making it readily available for international use.
The results show a moderate overall agreement between the test and retest of the EP-DeFeC, which corroborates with the overall reproducibility of the adult DeFeC [8]. The reliability of the Rome IV criteria within the EP-DeFeC was comparable to previous reports [33]. Nevertheless, there was a remarkable difference between the high percentages of observed agreement of some questions and low kappa coefficients. This is mainly caused by extremely low kappa coefficients for questions with small numbers of positive answers, a statistical phenomenon which is termed the Cicchetti paradox [34]. In this case, the low kappa values reflect a low prevalence of the symptom in the cohort instead of a lack of reproducibility. Therefore, we provided both the observed agreement and the kappa coefficients.
An important strength of the present study is that the EP-DeFeC was developed and validated according to the structured COSMIN methods [9, 10]. The main limitation of the current study is that we could not determine the diagnostic validity of the EP-DeFeC, because currently no gold standard exists to objectively assess constipation and/or fecal incontinence in young children because both conditions are symptom-based diagnoses. Furthermore, the EP-DeFeC is created as a quick and easy tool to screen for bowel problems, without requiring physical examination. The Rome IV criterion of presence of a large fecal mass in the rectum, which points to functional constipation, was therefore not taken into account [2, 12]. In this way, the EP-DeFeC may slightly underestimate the prevalence of constipation, although it has been reported that digital rectal examination only has a marginal added value in satisfying the Rome criteria for functional constipation [35]. Another limitation is that the incorporated bowel function scores are not all validated for use in young children. Lastly, the assessment of fecal incontinence in young children is particularly challenging because it depends not only on disease severity, but also on the physiological ability to be toilet trained at a certain age. Therefore, it is important to keep the age of the child and the toilet training status in mind while interpreting the scores for fecal incontinence.
In conclusion, the EP-DeFeC is a feasible and validated questionnaire for assessing bowel function, coexisting disorders, and/or causative factors in children from 1 month to 7 years of age. The development of this questionnaire enables longitudinal follow-up of bowel function from infancy to adulthood, when combined with its pediatric (8 to 17 years) and adult (18 years and over) equivalents. We therefore encourage using the EP-DeFeC for longitudinal clinical purposes and for scientific research.
Abbreviations
- COSMIN:
-
Consensus-based Standards for the selection of health Measurement Instruments
- DeFeC:
-
Defecation and Fecal Continence
- EP-DeFeC:
-
Early Pediatric DeFeC
- IBS:
-
Irritable bowel syndrome
- ICC:
-
Intraclass correlation coefficient
- ICCS:
-
International Children’s Continence Society
- ICS:
-
International Continence Society
- LARS:
-
Low anterior resection syndrome
- MeSH:
-
Medical Subject Heading
- P-DeFeC:
-
Pediatric DeFeC
- PICS:
-
Pediatric incontinence/constipation score
References
Koppen IJN, Vriesman MH, Saps M, Rajindrajith S, Shi X, van Etten-Jamaludin FS, Di Lorenzo C, Benninga MA, Tabbers MM (2018) Prevalence of functional defecation disorders in children: a systematic review and meta-analysis. J Pediatr. https://doi.org/S0022-3476(18)30217-8
Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M (2016) Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. https://doi.org/10.1053/j.gastro.2016.02.015
Steutel NF, Zeevenhooven J, Scarpato E, Vandenplas Y, Tabbers MM, Staiano A, Benninga MA (2020) Prevalence of functional gastrointestinal disorders in european infants and toddlers. J Pediatr. https://doi.org/S0022-3476(20)30291-2
Robin SG, Keller C, Zwiener R, Hyman PE, Nurko S, Saps M, Di Lorenzo C, Shulman RJ, Hyams JS, Palsson O, van Tilburg, MAL (2018) Prevalence of pediatric functional gastrointestinal disorders utilizing the Rome IV Criteria. J Pediatr. https://doi.org/S0022-3476(17)31634-7
van Tilburg MA, Hyman PE, Walker L, Rouster A, Palsson OS, Kim SM, Whitehead WE (2015) Prevalence of functional gastrointestinal disorders in infants and toddlers. J Pediatr. https://doi.org/S0022-3476(14)01114-7
Liem O, Harman J, Benninga M, Kelleher K, Mousa H, Di Lorenzo C (2009) Health utilization and cost impact of childhood constipation in the United States. J Pediatr. https://doi.org/10.1016/j.jpeds.2008.07.060
Boronat AC, Ferreira-Maia AP, Matijasevich A, Wang YP (2017) Epidemiology of functional gastrointestinal disorders in children and adolescents: a systematic review. World J Gastroenterol. https://doi.org/10.3748/wjg.v23.i21.3915
Meinds RJ, Timmerman MEW, van Meegdenburg MM, Trzpis M, Broens PMA (2018) Reproducibility, feasibility and validity of the Groningen Defecation and Fecal Continence questionnaires. Scand J Gastroenterol 53:790–796
Mokkink LB, Prinsen C, Patrick DL, Alonso J, Bouter LM, De Vet H, Terwee CB (2019) COSMIN study design checklist for patient-reported outcome measurement instruments
Gagnier JJ, Lai J, Mokkink LB, Terwee LB (2021) COSMIN reporting guideline for studies on measurement properties of patient reported outcome measures
Lewis SJ, Heaton KW (1997) Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. https://doi.org/10.3109/00365529709011203
Benninga MA, Nurko S, Faure C, Hyman PE, St. James Roberts I, Schechter NL, (2016) Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology. https://doi.org/10.1053/j.gastro.2016.02.016
de Abreu GE, Dias Souto Schmitz, A. P., Dourado ER, Barroso U Jr (2019) Association between a constipation scoring system adapted for use in children and the dysfunctional voiding symptom score in children and adolescents with lower urinary tract symptoms. J Pediatr Urol. https://doi.org/S1477-5131(19)30232-3
Renzi A, Brillantino A, Di Sarno G, d’Aniello F (2013) Five-item score for obstructed defecation syndrome: study of validation. Surg Innov 20:119–125
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77–97
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA (1999) Prospective comparison of faecal incontinence grading systems. Gut 44:77–80
Fichtner-Feigl S, Sailer M, Höcht B, Thiede A (2003) Development of a new scoring system for the evaluation of incontinence and constipation in children. Coloproctology
Holschneider AM (1983) Elektromanometrie des Enddarms. Urban & Schwarzenberg, Munich-Wien-Baltimore
Templeton JM,Jr, Ditesheim JA (1985) High imperforate anus--quantitative results of long-term fecal continence. J Pediatr Surg. https://doi.org/S002234688500152X
Rintala RJ, Lindahl H (1995) Is normal bowel function possible after repair of intermediate and high anorectal malformations?. J Pediatr Surg. https://doi.org/S0022-3468(95)90064-0
Austin PF, Bauer SB, Bower W, Chase J, Franco I, Hoebeke P, Rittig S, Vande Walle J, von Gontard A, Wright A, Yang SS, Nevéus T (2014) The standardization of terminology of lower urinary tract function in children and adolescents: update report from the Standardization Committee of the International Children's Continence Society. J Urol
Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD (1996) A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 39:681–685
Lacy BE, Mearin F, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R (2016) Bowel disorders. Gastroenterology. https://doi.org/10.1053/j.gastro.2016.02.031
Rao SSC, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, Wald A (2016) Anorectal disorders. Gastroenterology. https://doi.org/10.1053/j.gastro.2016.02.009
Emmertsen KJ, Laurberg S (2012) Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg. https://doi.org/10.1097/SLA.0b013e31824f1c21
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A, Standardisation Sub-Committee of the International Continence Society (2003) The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. https://doi.org/S0090429502022434
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics
Rajindrajith S, Devanarayana NM, Thapar N, Benninga MA (2021) Functional fecal incontinence in children: epidemiology, pathophysiology, evaluation, and management. J Pediatr Gastroenterol Nutr. https://doi.org/10.1097/MPG.0000000000003056
Kuizenga-Wessel S, Steutel NF, Benninga MA, Devreker T, Scarpato E, Staiano A, Szajewska H, Vandenplas Y, Tabbers MM (2017) Development of a core outcome set for clinical trials in childhood constipation: a study using a Delphi technique. BMJ Paediatr Open. https://doi.org/10.1136/bmjpo-2017-000017
den Hertog J, van Leengoed E, Kolk F, van den Broek L, Kramer E, Bakker EJ, Bakker-van Gijssel E, Bulk A, Kneepkens F, Benninga MA (2012) The defecation pattern of healthy term infants up to the age of 3 months. Arch Dis Child Fetal Neonatal Ed. https://doi.org/10.1136/archdischild-2011-300539
Turco R, Miele E, Russo M, Mastroianni R, Lavorgna A, Paludetto R, Pensabene L, Greco L, Campanozzi A, Borrelli O, Romano C, Chiaro A, Guariso G, Staiano A (2014) Early-life factors associated with pediatric functional constipation. J Pediatr Gastroenterol Nutr. https://doi.org/10.1097/MPG.0000000000000209
van Summeren JJGT, Holtman GA, van Ommeren SC, Kollen BJ, Dekker JH, Berger MY (2018) Bladder symptoms in children with functional constipation: a systematic review. J Pediatr Gastroenterol Nutr. https://doi.org/10.1097/MPG.0000000000002138
Baaleman DF, Velasco-Benítez CA, Méndez-Guzmán LM, Benninga MA, Saps M (2021) Can we rely on the Rome IV questionnaire to diagnose children with functional gastrointestinal disorders? J Neurogastroenterol Motil. https://doi.org/10.5056/jnm20179
Cicchetti DV, Feinstein AR (1990) High agreement but low kappa: II. Resolving the paradoxes. J Clin Epidemiol. https://doi.org/S0895-4356(90)90159-M
Pradhan S, Jagadisan B (2018) Yield and examiner dependence of digital rectal examination in detecting impaction in pediatric functional constipation. J Pediatr Gastroenterol Nutr. https://doi.org/10.1097/MPG.0000000000001969
Acknowledgements
The authors thank the participants of the Delphi panel for their time and feedback. We also acknowledge T. van Wulfften Palthe, PhD, for correcting the English manuscript. Finally, we thank all respondents for participating.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by all authors. The first draft of the manuscript was written by Sanne Verkuijl and Monika Trzpis and Paul Broens commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Verkuijl, S.J., Trzpis, M. & Broens, P.M.A. Development and validation of the Early Pediatric Groningen Defecation and Fecal Continence questionnaire. Eur J Pediatr 182, 615–623 (2023). https://doi.org/10.1007/s00431-022-04714-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04714-2