Abstract
Puberty has been described as a life stage of considerable metabolic risk specially for those with obesity. The low-grade systemic inflammatory status associated with obesity could be one of the connections with metabolic syndrome (MetS). Thus, we aimed to assess the relationship between inflammatory and cardiovascular biomarkers and the development of MetS during puberty. Seventy-five children from the PUBMEP study (33 females), aged 4–18 years, were included. Cardiovascular and inflammatory biomarkers were measured in the prepubertal and pubertal stage, including high-sensitivity C-reactive protein (CRP), leptin, tumor necrosis factor-alpha (TNFα), interleukin 8 (IL8), monocyte chemoattractant protein 1 (MCP-1), total plasminogen activator inhibitor-1 (tPAI), resistin, adiponectin, myeloperoxidase (MPO), and soluble intercellular adhesion molecule-1 (sICAM-1). MetS was diagnosed at each measurement point. Mixed-effects and logistic regressions were performed. Those children with MetS in puberty presented higher prepubertal values of several cardiometabolic biomarkers in comparison to those without MetS (z-score body mass index (zBMI), waist circumference, insulin, HOMA-IR, leptin, and tPAI (p < 0.05)). For prepubertal children with obesity, the odds of developing MetS in puberty were significantly higher in those having high zBMI (OR = 4.27; CI: 1.39–22.59) or high concentrations of tPAI (OR = 1.19; CI: 1.06–1.43).
Conclusion: Those with obesity with higher prepubertal tPAI plasma levels had 19% higher odds of having MetS at puberty highlighting the existence of association between MetS, obesity, and inflammation already in puberty. Thus, assessing cardiometabolic and inflammatory status in children with obesity already at prepuberty is key to avoiding future comorbidities.
What is Known: • Inflammation, metabolic syndrome, and obesity may have their onset in childhood. • Puberty is a life stage characterized for an increased cardiovascular risk. | |
What is New: • Prepuberty state could be an early indicator of future cardiometabolic risk. • Children with obesity and high total plasminogen have higher odds of future metabolic syndrome. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood obesity is considered a worldwide concern as the rate of increase, in many countries, has been greater than the rate of increase in adult obesity [1]. In addition, childhood obesity has been related to cardiovascular diseases and diabetes in adulthood [2]. Among these diseases, metabolic syndrome (MetS) is a cluster of several cardiometabolic risk factors such as hyperglycemia, dyslipidemia, elevated blood pressure, and central or total adiposity [3]. In 2020, about 3% of children and 5% of adolescents had MetS, with some variation across countries and regions and the definitions used [4].
The presence of MetS in childhood has been associated with the risk of cardiometabolic disorders in adulthood [5, 6] and with subclinical atherosclerosis in obese children [7]. Additionally, those with MetS in childhood showed a higher risk in later life of diabetes mellitus type 2 (T2DM) and a higher risk of having high carotid intima-media thickness cIMT [5]. Thus, the presence of MetS in childhood could predict future cardiovascular risk factors; this could be due to the association between MetS and inflammation, which could be triggered by adiposity. In previous studies, obesity has been associated with MetS in all stages of childhood, independently of the definition used [8] and this prevalence of MetS in children and adolescents increases with the severity of obesity [9].
As adiposity is considered the common trigger for MetS and the inflammatory state, it has been suggested that both could co-exist [10], but there is some controversy [11]. The increase of the adipose tissue mass leads to an increased turnover of free fatty acids (FFAs) and changes in the secretion of pro-inflammatory adipokines [12]. This secretion of hormones and adipocytokines, such as leptin, adiponectin, resistin, and monocyte chemoattractant protein 1 (MCP-1), among others, as well as a variety of interleukins together with TNF-α, enhance the development and/or the progression of chronic diseases, including insulin resistance and chronic inflammation [13].
Puberty is an important physiological stage in childhood, characterized by changes on endocrine function, among others. It has been shown that increases in body mass index (BMI) and the propensity of overweight and obesity follow a quadratic growth curve with the steepest increase before and during puberty [14]. Additionally, some studies have shown significant differences in MetS between the prepubertal and postpubertal stages, pointing to puberty as a metabolically risky life period for children with obesity [8]. However, there is scarce information about the longitudinal association between MetS and inflammation during puberty.
Thus, the present study aimed to evaluate the association between the longitudinal trajectories of cardiometabolic and inflammatory markers during puberty and the development of MetS in a sample of Spanish children with obesity. Additionally, the risk of developing MetS during puberty was evaluated considering the prepubertal levels of assessed cardiometabolic and inflammatory biomarkers.
Materials and methods
Study design
For the overall PUBMEP study (“Puberty and metabolic risk in obese children. Epigenetic alterations and pathophysiological and diagnostic implications”), a total of 374 subjects were contacted, of which 49 were not located, 36 could not participate because they had changed their place of residence or met any of the exclusion criteria, and 98 declined the invitation. Out of them, 191 agreed to participate in the PUBMEP study. All these children were recruited as prepubertal children during the period 2012–2015, T1, and called again for follow-up medical consultation in 2018, T2. Children were recruited at Lozano Blesa University Clinical Hospital (Zaragoza), Santiago de Compostela University Clinical Hospital (Santiago de Compostela), and Reina Sofia University Clinical Hospital (Córdoba).
However, 75 children participated in the present study (42 boys and 33 girls) as they had complete information in both time points, T1 and T2, for all the anthropometric markers and all the cardiometabolic biomarkers.
Ethical considerations
The PUBMEP study has been conducted following the Declaration of Helsinki (Edinburgh 2000 revised). Moreover, the study was approved by the corresponding ethic committees in each of the participating centers. All parents or guardians and children over 12 years provided written informed consent, while younger children gave their assent.
Anthropometric measurements
A set of anthropometric markers were measured by trained researchers using standard procedures: body weight (kg, SECA 701 model class III digital display (Germany)), height (cm, a Harpenden wall-mounted stadiometer), and waist circumference (WC, SECA (Germany) (cm)) were measured twice in underwear or light sportswear and barefoot. Blood pressure was measured three times. The measurement was performed with an OMRON M3 digital blood pressure monitor (Japan) after 5 min of resting.
The BMI status (weight in kg/height in m2) was identified according to Cole et al. [15]. The abdominal waist measurements were related to the Spanish percentile tables of Fernández et al. [16]. Besides the assessment of the pubertal stage following the Tanner classification (1 for prepubertal and 2–5 for pubertal children) [17, 18], it was also confirmed with a hormonal study.
Metabolic syndrome definition
To determine the presence of MS, we used the definition established by Olza et al. in 2011 [19], which includes obesity (body mass index or zBMI > 95p) and one of the following: hypertension (BP z-score > 95p), insulin resistance (HOMA IR ≥ 95p), hypertriglyceridemia (TAG z-score > 95p) [20], and low HDL-c (HDL-c < 5p) [21]. The 95th percentile of HOMA-IR was considered 2.5 in the prepubertal stage, 3.38 in pubertal boys, and 3.905 in pubertal girls established in a cohort of Spanish children [22, 23]. The values of blood pressure adjusted for sex, age, and height were classified according to international references [24].
Biomarkers
Samples were obtained after 12 h of fasting status. Total cholesterol and triacylglycerols (TAG) (Advia 2400 Chemistry system; Siemens healthcare diagnostics, Erlangen, Germany) and HDL-c and low-density lipoprotein cholesterol were determined (LDL-c) (SAS-3 cholesterol profile kit—Helena Biosciences Europe; Tyne and Wear, UK). Plasma fasting glucose (Advia 2400 Chemistry system; Siemens healthcare diagnostics, Erlangen, Germany) and insulin (Advia centaur XP analyzer, Siemens healthcare diagnostics, Erlangen, Germany) determinations were used to calculate the HOMA-IR index.
Regarding inflammatory biomarkers, high-sensitivity C-reactive protein (hsCRP) was determined using a particle-enhanced turbidimetric immunoassay (Dade Behring Inc., Deerfield, IL, USA). The rest of the inflammatory biomarkers: adiponectin, leptin, resistin, TNF-α, IL-8, total plasminogen activator inhibitor-1 (tPAI-1), myeloperoxidase (MPO), monocyte chemoattractant protein-1 (MCP-1), soluble intercellular cell adhesion molecule-1 sICAM-1, and soluble vascular cell adhesion molecule-1 (sVCAM) were analyzed using a Luminex 200 system (Luminex Corporation, Austin, TX, USA) with human monoclonal antibodies from Millipore (EMD Millipore Corp, Billerica, MA).
Statistical analysis
Continuous values in descriptive tables are expressed as mean and standard deviation, median and interquartile range, or sample and percentage. All variables, except age, Tanner stage, and glucose, were log-transformed. In the descriptive statistics of the sample, the overall progression of body composition and cardiometabolic and inflammatory biomarkers from prepubertal to pubertal are shown. In addition, results of the progression were analyzed by sex.
Also, a prospective analysis was performed grouping the participants by BMI category and MetS prevalence in prepuberty. Four categories were considered: normal weight (NW), overweight (OW), obesity with no-MetS (OB no-MS), and obesity with MetS (OB MS). Then, a retrospective analysis of the cardiometabolic and inflammatory biomarkers and their increment, where participants were grouped by MetS prevalence in puberty, was performed. For these analyses, mixed-effects linear models were employed. The models included fixed effects for puberty stage, group, and their interaction to allow within and between-group comparisons and Tanner stage and sex to correct for any differences in pubertal stage and sex between groups. For all the analyses, mixed-effect models were fitted for each of the variables. A random effect for participants was included to account for repeated measures.
The models were used to test for changes in outcomes during progression from prepubertal to pubertal stage within each group, pairwise outcomes differences at the prepubertal stage between groups, and pairwise differences in the prepubertal-pubertal progression between groups (Supplementary Table 1). All tests were calculated using the Kenward-Roger method for degrees of freedom and corrected for false discovery rate using the Benjamini–Yekutieli procedure.
Finally, backward stepwise model selection based on AIC was used to select the final model that best predicts MS in puberty according to prepubertal data in children with obesity in prepuberty. Variables included in the initial model were prepubertal levels of BMI-z, leptin, TNF-α, resistin, adiponectin, sICAM1, MPO, MCP1, tPAI, HOMA-IR, and age, as well as sex and Tanner stage in puberty (as confounding factors) (Supplementary Table 2).
All statistical analyses were performed using the R statistical package (4.1.0 version). Differences found were significant when p < 0.005.
Results
Descriptive characteristics for the study population can be found in Table 1. Body composition and inflammatory and cardiometabolic biomarkers values in the prepubertal and pubertal stages are shown in that table for the overall population and by sex.
There were differences by pubertal stage in the overall population, being the concentrations of those biomarkers included in the MetS definition, DBP, SBP, HOMA-IR, and TAG, significantly higher in puberty (p < 0.05). On the other hand, HDL-c and LDL-c had significantly lower concentrations in puberty when compared with prepuberty (p < 0.005). Regarding the inflammatory biomarkers, IL8 and adiponectin showed significant differences by pubertal stage (p < 0.05). For girls, significant differences (p < 0.05) by pubertal status were found for HOMA-IR, among the MetS components, and leptin, while, for boys, those differences (p < 0.05) were found for SBP, HOMA-IR, TAG, and HDL-c and, among the inflammatory biomarkers, for adiponectin (p < 0.001).
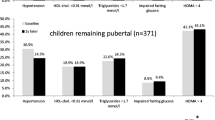
In Table 2, participants are divided by BMI category and prevalence of MetS in prepuberty (NW, OW, OB no-MS, and OB MS) and their body composition markers, cardiometabolic and inflammatory variables were assessed in the prepubertal, the pubertal stage and the increase or change, i.e., T2 values − T1 values. Regarding the within-group changes, age and WC were the variables that showed significant differences from pre to pubertal stage within all assessed groups: NW, OW, OB no-MS, and OB MS. Prepubertal differences between groups showed that NW subjects had significantly lower values than the rest of the groups for BMI-z, WC, insulin, HOMA-IR, and leptin. Those in the prepubertal NW groups had also lower values of tPAI in comparison with those in the OB groups: OB no-MS and OB MS.
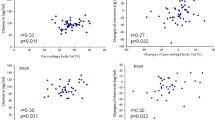
To analyze how prepubertal values of cardiometabolic and inflammatory biomarkers, and their increment, are associated with the prevalence of MetS in puberty, we post-categorized the subjects based on if they presented MS in puberty or not. Descriptive statistics of participants at the prepubertal and pubertal stage, as well as the prepubertal-pubertal increment, are presented in Table 3, grouped by MetS prevalence in puberty. Significant changes (p < 0.05) from pre- to pubertal stages were found for BMI, WC, insulin, HOMA-IR, cholesterol, HDL-c, TAG, IL-8, and adiponectin within the group of those no-MS in puberty. The prepubertal values of BMI-z, WC, HOMA-IR, leptin, and tPAI were higher between groups for those that developed MS in puberty. For those with MetS in puberty, significant increments from pre- to pubertal stages were found for BMI, WC, and DBP. There were no significant between-group differences in the evolution of the anthropometry and cardiometabolic and inflammatory biomarkers between participants with and without MS in puberty (data not shown).
As all participants who presented MetS in puberty were obese, in Table 4 results of a stepwise logistic regression to test which prepubertal inflammatory biomarker helps the most to predict MetS are shown. For this, we restricted analyses to the group of 34 children with obesity in the prepubertal stage. Within these participants, among the inflammatory biomarkers included in the model, tPAI significantly (p < 0.017) helped to predict MetS in puberty (OR = 1.19; CI: 1.06–1.43).
Discussion
In this study, significant differences in obesity degree and MetS were observed longitudinally for the mean concentrations of a set of anthropometric and cardiovascular/inflammatory biomarkers in childhood. Those with MetS in puberty had already higher values of several cardiometabolic biomarkers in prepuberty. Finally, it was observed that the odds of having MetS in puberty were significantly higher when having high zBMI or high concentrations of tPAI, for those obese in prepuberty.
Puberty is a transition period, characterized by physiologic change, including secretion of sex steroids, acceleration in growth, and accumulation of both lean and fat mass. Puberty is also a period of change for the cardiometabolic risk factors, insulin resistance, plasma lipids, blood pressure, and adipokines [25,26,27]. Also, puberty is one of the greatest risk factors for impairment of body composition [28] and the transition from metabolically healthy to unhealthy obesity [29].
Overall, in our sample, we observed a derangement associated with pubertal development for most of the cardiometabolic markers in both sexes. However, for cholesterol and LDL-c we found a better profile in those pubertal when compared with the prepubertal participants. Previous evidence suggests that there are changes in total cholesterol and lipid profiles during puberty. Out of these changes, the most well-described are the decrease in total and low-density lipoprotein cholesterol during puberty which are in line with our results [26, 30,31,32]. It has been suggested that the changes in lipid levels occurring during adolescence and sexual maturation are closely related to the alterations in hormones during this period of life. However, most of the studies assessing changes in lipids over time do not consider pubertal maturation so results are mostly based on cross-sectional studies.
Research on the effects of hormones on immune functioning also suggests a link between pubertal development and inflammatory physiology [33]. Prior works suggest that sex hormones, which increase during puberty, can have an immunomodulatory effect on inflammatory biomarkers [27]. In our sample, we found an increase of sICAM in pubertal boys. Also, changes in adiponectin and leptin could occur during puberty. Leptin plays a role in the initiation of puberty and increases in puberty [34]. However, sex differences could be found. In girls, leptin increases throughout puberty to adulthood, whereas in boys, leptin tends to decrease [35, 36]. In the present study, leptin was significantly increased in pubertal girls while for pubertal boys the value was lower than in prepuberty even if the decrease was not significant. In adults, sex is the major determinant of leptin concentrations, being higher in women than men [37]. In our study, adiponectin changes differentially in boys’ and girls’ puberty: in girls, there could be a small change, whereas in boys decreases at pubertal onset and continues to go down as puberty progresses [38, 39]. This is in line with our results, where a significant decrease in adiponectin was found in pubertal boys.
In our sample, 12% of the participants exhibited features of MetS. However, there is no consensus regarding the definition of the MetS for children, which makes more difficult the diagnosis [40]. Depending on the definition used, prevalence ranged from 7.6 to 30.8% in a sample of Spanish children [41]. Despite this, it seems clear that MetS is linked to several cardiometabolic diseases and that could increase the risk of future comorbidities. However, only a few studies have examined the link between early life MetS and future cardiovascular disease [6, 42]. Results from a longitudinal study showed that MetS in childhood, combined with changes in age-specific BMI percentile, predicted cardiovascular events later in adulthood [6]. In addition, a study from Magnussen et al. [42] found that MetS in youth could predict MetS in adulthood and high cIMT and T2DM in early to middle adulthood.
In the retrospective analysis conducted comparing the cardiometabolic and inflammatory biomarkers during puberty by prepubertal obesity degree and the prepubertal presence or not of MetS, we observed that children with obesity but no MetS at prepuberty had significantly lower values of zBMI, TNF, resistin, and adiponectin between the pubertal stages. In literature, resistin has been shown to be a potential activator of inflammatory markers and expression of cellular adhesion molecules (CAMs) on the endothelial surface [43]. It has been observed that adolescents with obesity have higher values of resistin independently of their adipose tissue [44]. However, it seems to be an association between resistin, gender, and Tanner stage, which has also been found for adiponectin, that could affect the concentrations [39, 45].
In the longitudinal analysis, we found differences by pubertal status on the cardiometabolic and inflammatory concentrations by MetS status in puberty. Those with MetS in puberty had significantly higher prepubertal values of BMI, zBMI, WC, insulin, HOMA-IR, leptin, and t-PAI than those without MetS. These results suggest that there are already cardiometabolic and inflammatory biomarkers increased during prepuberty for those that will present MetS in the future. Leptin and tPAI are adipokines that have been involved with MetS and the inflammatory process [46]. Also, in previous studies, tPAI has been increased in children with obesity and MetS [22, 47] and also in metabolically unhealthy children [23]. In this last study, PAI-1 was increased in metabolically unhealthy children with overweight/obesity in the prepubertal stage.
In line with these results, we also investigated if having higher prepubertal values of specific biomarkers when obese could predict the prevalence of MetS in puberty. Out of all the cardiometabolic biomarkers investigated, prepubertal tPAI showed associations with future MetS. Possible mechanisms linking increased circulating PAI-1 levels to the MetS suggest that tPAI could have a significant role in metabolic health [48]. Out of the mechanisms, tPAI contributes to the development of adipose tissue and insulin resistance [48]. However, the mechanisms seem complex and probably are interrelated so more longitudinal studies are needed to investigate in deep these associations. In a previous cross-sectional study in adults, PAI-1 and adiponectin showed the most robust associations with MetS components in a general population, indicating that unfavorable adipose tissue performance is a key contributor to these metabolic anomalies [49].
The present work has several limitations. The sample size was low which could affect to the statistical power and to enroll more population would be needed to validate the higher tPAI odds with biomarkers. Also, the analysis was not stratified by sex, due to the sample size. As strengths, we managed to get complete data on the prepubertal and pubertal states of children from three Spanish regions. Also, this is one of the first studies to analyze the association between MetS and cardiometabolic inflammatory biomarkers, assessing the association in both directions, in a sample of prepubertal and pubertal children. Finally, children were individually examined by clinicians to determine their Tanner stage and the diagnosis was confirmed with hormonal variables.
In conclusion, those with MetS in puberty had already higher values of several cardiometabolic biomarkers in prepuberty suggesting that prepuberty is a critical period for the onset of future MetS. In line with this, those with higher prepubertal tPAI had 19% odds of having MetS at puberty which highlights the bi-directional association between MetS and specific biomarkers. Thus, assessing cardiometabolic status already at prepuberty is key to avoiding future comorbidities. Further studies with large population are needed to confirm these results.
References
Collaborators GBDO, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K et al (2017) Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 377(1):13–27
Bjerregaard LG, Jensen BW, Angquist L, Osler M, Sorensen TIA, Baker JL (2018) Change in overweight from childhood to early adulthood and risk of type 2 diabetes. N Engl J Med 378(14):1302–1312
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA et al (2005) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation 112(17):2735–2752
Noubiap JJ, Nansseu JR, Lontchi-Yimagou E, Nkeck JR, Nyaga UF, Ngouo AT et al (2022) Global, regional, and country estimates of metabolic syndrome burden in children and adolescents in 2020: a systematic review and modelling analysis. Lancet Child Adolesc Health 6(3):158–170
Magnussen CG, Koskinen J, Chen W, Thomson R, Schmidt MD, Srinivasan SR et al (2010) Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation 122(16):1604–1611
Morrison JA, Friedman LA, Gray-McGuire C (2007) Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: the Princeton Lipid Research Clinics Follow-up Study. Pediatrics 120(2):340–345
Huang K, Zou CC, Yang XZ, Chen XQ, Liang L (2010) Carotid intima-media thickness and serum endothelial marker levels in obese children with metabolic syndrome. Arch Pediatr Adolesc Med 164(9):846–851
Ekelund U, Anderssen S, Andersen LB, Riddoch CJ, Sardinha LB, Luan J et al (2009) Prevalence and correlates of the metabolic syndrome in a population-based sample of European youth. Am J Clin Nutr 89(1):90–96
Calcaterra V, Klersy C, Muratori T, Telli S, Caramagna C, Scaglia F et al (2008) Prevalence of metabolic syndrome (MS) in children and adolescents with varying degrees of obesity. Clin Endocrinol 68(6):868–872
Berg AH, Scherer PE (2005) Adipose tissue, inflammation, and cardiovascular disease. Circ Res 96(9):939–949
Wärnberg J, Marcos A (2008) Low-grade inflammation and the metabolic syndrome in children and adolescents. Curr Opin Lipidol 19(1):11–15
Stefan N, Haring HU (2013) The role of hepatokines in metabolism. Nat Rev Endocrinol 9(3):144–152
Boutari C, Mantzoros CS (2018) Inflammation: a key player linking obesity with malignancies. Metabolism 81:A3–A6
Rzehak P, Heinrich J (2006) Development of relative weight, overweight and obesity from childhood to young adulthood. A longitudinal analysis of individual change of height and weight. Eur J Epidemiol. 21(9):661–672
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ (Clinical research ed) 320(7244):1240–1243
Fernández JR, Redden DT, Pietrobelli A, Allison DB (2004) Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr 145(4):439–444
Marshall WA, Tanner JM (1969) Variations in pattern of pubertal changes in girls. Arch Dis Child 44(235):291–303
Marshall WA, Tanner JM (1970) Variations in the pattern of pubertal changes in boys. Arch Dis Child 45(239):13–23
Olza J, Gil-Campos M, Leis R, Bueno G, Aguilera CM, Valle M et al (2011) Presence of the metabolic syndrome in obese children at prepubertal age. Ann Nutr Metab 58(4):343–350
Hickman TB, Briefel RR, Carroll MD, Rifkind BM, Cleeman JI, Maurer KR et al (1998) Distributions and trends of serum lipid levels among United States children and adolescents ages 4–19 years: data from the Third National Health and Nutrition Examination Survey. Prev Med 27(6):879–890
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report 106(25):3143–421
Olza J, Aguilera CM, Gil-Campos M, Leis R, Bueno G, Valle M et al (2015) A continuous metabolic syndrome score is associated with specific biomarkers of inflammation and CVD risk in prepubertal children. Ann Nutr Metab 66(2–3):72–79
Rupérez AI, Olza J, Gil-Campos M, Leis R, Bueno G, Aguilera CM et al (2018) Cardiovascular risk biomarkers and metabolically unhealthy status in prepubertal children: comparison of definitions. Nutr Metab Cardiovasc Dis 28(5):524–530
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114(2 Suppl 4th Report):555–576
Kelsey MM, Zeitler PS (2016) Insulin resistance of puberty. Curr DiabRep 16(7):64
Morrison JA, Laskarzewski PM, Rauh JL, Brookman R, Mellies M, Frazer M et al (1979) Lipids, lipoproteins, and sexual maturation during adolescence: the Princeton maturation study. Metabolism 28(6):641–649
Stumper A, Moriarity DP, Coe CL, Ellman LM, Abramson LY, Alloy LB (2020) Pubertal status and age are differentially associated with inflammatory biomarkers in female and male adolescents. J Youth Adolesc 49(7):1379–1392
Dai S, Labarthe DR, Grunbaum JA, Harrist RB, Mueller WH (2002) Longitudinal analysis of changes in indices of obesity from age 8 years to age 18 years. Project HeartBeat! Am J Epidemiol. 156(8):720–729
Reinehr T, Wolters B, Knop C, Lass N, Holl RW (2015) Strong effect of pubertal status on metabolic health in obese children: a longitudinal study. J Clin Endocrinol Metab 100(1):301–308
Altwaijri YA, Day RS, Harrist RB, Dwyer JT, Ausman LM, Labarthe DR (2009) Sexual maturation affects diet-blood total cholesterol association in children: Project HeartBeat! Am J Prev Med 37(1 Suppl):S65-70
Porkka KV, Viikari JS, Rönnemaa T, Marniemi J, Akerblom HK (1994) Age and gender specific serum lipid and apolipoprotein fractiles of Finnish children and young adults. The Cardiovascular Risk in Young Finns Study. Acta Paediatr. 83(8):838–848
Tell GS, Mittelmark MB, Vellar OD (1985) Cholesterol, high density lipoprotein cholesterol and triglycerides during puberty: the Oslo Youth Study. Am J Epidemiol 122(5):750–761
Klein SL, Flanagan KL (2016) Sex differences in immune responses. Nat Rev Immunol 16(10):626–638
Garcia-Mayor RV, Andrade MA, Rios M, Lage M, Dieguez C, Casanueva FF (1997) Serum leptin levels in normal children: relationship to age, gender, body mass index, pituitary-gonadal hormones, and pubertal stage. J Clin Endocrinol Metab 82(9):2849–2855
Ahmed ML, Ong KK, Morrell DJ, Cox L, Drayer N, Perry L et al (1999) Longitudinal study of leptin concentrations during puberty: sex differences and relationship to changes in body composition. J Clin Endocrinol Metab 84(3):899–905
Arslanian S, Suprasongsin C, Kalhan SC, Drash AL, Brna R, Janosky JE (1998) Plasma leptin in children: relationship to puberty, gender, body composition, insulin sensitivity, and energy expenditure. Metabolism 47(3):309–312
Saad MF, Damani S, Gingerich RL, Riad-Gabriel MG, Khan A, Boyadjian R et al (1997) Sexual dimorphism in plasma leptin concentration. J Clin Endocrinol Metab 82(2):579–584
Andersen KK, Frystyk J, Wolthers OD, Heuck C, Flyvbjerg A (2007) Gender differences of oligomers and total adiponectin during puberty: a cross-sectional study of 859 Danish school children. J Clin Endocrinol Metab 92(5):1857–1862
Böttner A, Kratzsch J, Müller G, Kapellen TM, Blüher S, Keller E et al (2004) Gender differences of adiponectin levels develop during the progression of puberty and are related to serum androgen levels. J Clin Endocrinol Metab 89(8):4053–4061
Tailor AM, Peeters PH, Norat T, Vineis P, Romaguera D (2010) An update on the prevalence of the metabolic syndrome in children and adolescents. Int J Pediatr Obes 5(3):202–213
Olza J, Gil-Campos M, Leis R, Bueno G, Aguilera CM, Valle M et al (2011) Presence of the metabolic syndrome in obese children at prepubertal age. Ann Nutr Metab 58(4):343–350
Magnussen CG, Koskinen J, Chen W, Thomson R, Schmidt MD, Srinivasan SR et al (2010) Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation 122(16):1604–1611
Reilly MP, Lehrke M, Wolfe ML, Rohatgi A, Lazar MA, Rader DJ (2005) Resistin is an inflammatory marker of atherosclerosis in humans. Circulation 111(7):932–939
Maggio AB, Wacker J, Montecucco F, Galan K, Pelli G, Mach F et al (2012) Serum resistin and inflammatory and endothelial activation markers in obese adolescents. J Pediatr 161(6):1022–1027
Gerber M, Boettner A, Seidel B, Lammert A, Bär J, Schuster E et al (2005) Serum resistin levels of obese and lean children and adolescents: biochemical analysis and clinical relevance. J Clin Endocrinol Metab 90(8):4503–4509
Kim JE, Kim JS, Jo MJ, Cho E, Ahn SY, Kwon YJ et al (2022) The roles and associated mechanisms of adipokines in development of metabolic syndrome. Molecules 27(2):334
Olza J, Aguilera CM, Gil-Campos M, Leis R, Bueno G, Valle M et al (2014) Waist-to-height ratio, inflammation and CVD risk in obese children. Public Health Nutr 17(10):2378–2385
Alessi MC, Juhan-Vague I (2006) PAI-1 and the metabolic syndrome: links, causes, and consequences. Arterioscler Thromb Vasc Biol 26(10):2200–2207
Vecchiola A, García K, González-Gómez LM, Tapia-Castillo A, Artigas R, Baudrand R et al (2021) Plasminogen activator inhibitor-1 and adiponectin are associated with metabolic syndrome components. Am J Hypertens 35(4):311–318
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This work was supported by the Plan Nacional de Investigación Científica, Desarrollo e Innovación Tecnológica (I + D + I), Instituto de Salud Carlos III-Health Research Funding (FONDOS FEDER) (PI11/01425, PI11/02042, PI11/02059, PI16/01301, PI16/01205, PI16/00871 and PI20/00563); CIBEROBN Network (CB15/00131, CB15/00043); and Redes temáticas de investigación cooperativa RETIC (Red SAMID RD12/0026/0015).
Author information
Authors and Affiliations
Contributions
C.M.A., G.B., and R.L. contributed to the study conception and design. Material preparation, data collection, and analysis were performed by E.M.G.G., A.I.R., R.V.C., and K.F. The first draft of the manuscript was written by E.M.G.G., A.A.R., and C.M.A. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The PUBMEP study has been conducted following the Declaration of Helsinki (Edinburgh 2000 revised), and the recommendations of the Good Clinical Practice of the CEE (Document 111/3976/88 July 1990) and the legally enforced Spanish regulation, which regulates the clinical investigation of human beings (RD 223/04 about clinical trials). Moreover, the study was approved by the corresponding ethic committees in each of the participating centers.
Consent to participate
All parents or guardians and children over 12 years provided written informed consent, while younger children gave their assent.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Tobias Tenenbaum
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
González-Gil, E.M., Anguita-Ruiz, A., Kalén, A. et al. Longitudinal associations between cardiovascular biomarkers and metabolic syndrome during puberty: the PUBMEP study. Eur J Pediatr 182, 419–429 (2023). https://doi.org/10.1007/s00431-022-04702-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04702-6