Abstract
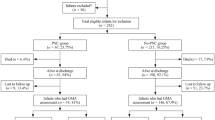
Acute chorioamnionitis and maternal vascular malperfusion are associated with an increased risk of bronchopulmonary dysplasia. To prevent bronchopulmonary dysplasia, postnatal corticosteroids are given to preterm neonates. Clinical observations indicate not all neonates respond to corticosteroids, the so-called non-responders. This study aimed to investigate the association between placental pathology and short-term response to postnatal corticosteroids in neonates < 32 weeks postconceptional age at risk for bronchopulmonary dysplasia. All neonates < 32 weeks born between 2009 and 2016, receiving corticosteroids in the course of BPD, were included. The preterm neonates were divided into three groups depending on placental histology: acute chorioamnionitis, maternal vascular malperfusion, or no placental pathology. Respiratory support was assessed prior to treatment and at days 4 and 7. A responder was defined as extubation within 7 days after starting corticosteroid treatment. In total, 52% of the chorioamnionitis neonates, 67% of the maternal vascular malperfusion neonates, and 58% of neonates in the no pathology group were responders. The odds ratio for extubation was 0.53 (0.18–1.55) at day 4 and 0.66 (0.23–1.97) at day 7, in the chorioamnionitis group compared to the maternal vascular malperfusion.
Conclusion: Short-term response to postnatal corticosteroids did not significantly differ between premature neonates born after acute chorioamnionitis, maternal vascular malperfusion, or no placenta pathology. However, a trend of better corticosteroid response in maternal vascular malperfusion neonates was found, potentially due to differences in prenatal pulmonary development and postnatal cortisol.
What is Known: |
• Bronchopulmonary dysplasia is related to chorioamnionitis and maternal vascular malperfusion. |
• Corticosteroids remain an important treatment in the course of bronchopulmonary dysplasia despite conflicting results and non-responsiveness in some preterm neonates. |
What is New: |
• Non-responsiveness might be related to differences in pulmonary inflammation and systemic cortisol due to predispositions triggered by chorioamnionitis or maternal vascular malperfusion. |
• Neonates born after maternal vascular malperfusion seem to respond better to postnatal corticosteroid treatment. |




Similar content being viewed by others
Abbreviations
- BPD :
-
Bronchopulmonary dysplasia
- BW :
-
Birth weight
- CA :
-
Chorioamnionitis
- CPAP:
-
Continues positive airway pressure
- FGR:
-
Fetal growth restriction
- FIR:
-
Fetal inflammatory response
- FiO2 :
-
Oxygen demand
- GA:
-
Gestational age
- HFO:
-
High frequency oscillation
- MAP:
-
Mean airway pressure
- MVM:
-
Maternal vascular malperfusion
- LF :
-
Low flow
- NIPPV:
-
Non-invasive positive pressure ventilation
- NP:
-
No pathology
- PEEP:
-
Positive end expiratory pressure
- PH:
-
Pulmonary hypertension
- PIP:
-
Peak inspiratory pressure
- PROM:
-
Premature rupture of membranes
References
Thébaud B, Goss KN, Laughon M, Whitsett JA, Abman SH, Steinhorn RH et al (2019) Bronchopulmonary dysplasia Nat Rev Dis Primers 5(1):78
Kramer BW, Lievense S, Been JV, Zimmermann LJ (2010) From classic to new bronchopulmonary dysplasia. Ned Tijdschr Geneeskd 154:A1024
Taglauer E, Abman SH, Keller RL (2018) Recent advances in antenatal factors predisposing to bronchopulmonary dysplasia. Semin Perinatol 42(7):413–424
Kim SY, Choi CW, Jung E, Lee J, Lee JA, Kim H et al (2015) Neonatal morbidities associated with histologic chorioamnionitis defined based on the site and extent of inflammation in very low birth weight infants. J Korean Med Sci 30(10):1476–1482
Mestan KK, Check J, Minturn L, Yallapragada S, Farrow KN, Liu X et al (2014) Placental pathologic changes of maternal vascular underperfusion in bronchopulmonary dysplasia and pulmonary hypertension. Placenta 35(8):570–574
Mir IN, Chalak LF, Brown LS, Johnson-Welch S, Heyne R, Rosenfeld CR et al (2020) Impact of multiple placental pathologies on neonatal death, bronchopulmonary dysplasia, and neurodevelopmental impairment in preterm infants. Pediatr Res 87(5):885–891
Barrington KJ (2001) The adverse neuro-developmental effects of postnatal steroids in the preterm infant: a systematic review of RCTs. BMC Pediatr 1:1
Watterberg K (2012) Evidence-based neonatal pharmacotherapy: postnatal corticosteroids. Clin Perinatol 39(1):47–59
Doyle LW, Davis PG, Morley CJ, McPhee A, Carlin JB, Investigators DS (2006) Low-dose dexamethasone facilitates extubation among chronically ventilator-dependent infants: a multicenter, international, randomized, controlled trial. Pediatrics 117(1):75–83
Watterberg KL, Gerdes JS, Cole CH, Aucott SW, Thilo EH, Mammel MC et al (2004) Prophylaxis of early adrenal insufficiency to prevent bronchopulmonary dysplasia: a multicenter trial. Pediatrics 114(6):1649–1657
Shaffer ML, Baud O, Lacaze-Masmonteil T, Peltoniemi OM, Bonsante F, Watterberg KL (2019) Effect of prophylaxis for early adrenal insufficiency using low-dose hydrocortisone in very preterm infants: an individual patient data meta-analysis. J Pediatr 207(136–42):e5
Baud O, Maury L, Lebail F, Ramful D, El Moussawi F, Nicaise C et al (2016) Effect of early low-dose hydrocortisone on survival without bronchopulmonary dysplasia in extremely preterm infants (PREMILOC): a double-blind, placebo-controlled, multicentre, randomised trial. The Lancet 387(10030):1827–1836
Onland W, Cools F, Kroon A, Rademaker K, Merkus MP, Dijk PH et al (2019) Effect of hydrocortisone therapy initiated 7 to 14 days after birth on mortality or bronchopulmonary dysplasia among very preterm infants receiving mechanical ventilation: a randomized clinical trial. JAMA 321(4):354–363
Cummings JJ, Pramanik AK (2022) Postnatal corticosteroids to prevent or treat chronic lung disease following preterm birth. Pediatrics e2022057530. https://doi.org/10.1542/peds.2022-057530
Lewis T, Chalise P, Gauldin C, Truog W (2019) Pharmacometabolomics of respiratory phenotypic response to dexamethasone in preterm infants at risk for bronchopulmonary dysplasia. Clin Transl Sci 12(6):591–599
Clauss C, Thomas S, Khodak I, Tack V, Akerman M, Hanna N et al (2020) Hydrocortisone and bronchopulmonary dysplasia: variables associated with response in premature infants. J Perinatol 40(9):1349–1357
Héneau A, Guimiot F, Mohamed D, Novais ARB, Alberti C, Baud O, et al (2018) Placental findings and effect of prophylactic hydrocortisone in extremely preterm infants. Pediatrics 141(2)
Khong TY, Mooney EE, Ariel I, Balmus NC, Boyd TK, Brundler MA et al (2016) Sampling and definitions of placental lesions: Amsterdam placental workshop group consensus statement. Arch Pathol Lab Med 140(7):698–713
Hendrix MLE, Bons JAP, Alers NO, Severens-Rijvers CAH, Spaanderman MEA, Al-Nasiry S (2019) Maternal vascular malformation in the placenta is an indicator for fetal growth restriction irrespective of neonatal birthweight. Placenta 87:8–15
Park HW, Choi YS, Kim KS, Kim SN (2015) Chorioamnionitis and patent ductus arteriosus: a systematic review and meta-analysis. PLoS ONE 10(9):e0138114
Galinsky R, Polglase GR, Hooper SB, Black MJ, Moss TJ (2013) The consequences of chorioamnionitis: preterm birth and effects on development. J Pregnancy 2013:412831
Bhatt AJ, Pryhuber GS, Huyck H, Watkins RH, Metlay LA, Maniscalco WM (2001) Disrupted pulmonary vasculature and decreased vascular endothelial growth factor, Flt-1, and TIE-2 in human infants dying with bronchopulmonary dysplasia. Am J Respir Crit Care Med 164(10 Pt 1):1971–1980
Coalson JJ (2006) Pathology of bronchopulmonary dysplasia. Semin Perinatol 30(4):179–184
Rabinovitch M, Gamble W, Nadas AS, Miettinen OS, Reid L (1979) Rat pulmonary circulation after chronic hypoxia: hemodynamic and structural features. Am J Physiol 236(6):H818–H827
Kuypers E, Collins JJ, Kramer BW, Ofman G, Nitsos I, Pillow JJ et al (2012) Intra-amniotic LPS and antenatal betamethasone: inflammation and maturation in preterm lamb lungs. Am J Physiol Lung Cell Mol Physiol 302(4):L380–L389
Villamor-Martinez E, Álvarez-Fuente M, Ghazi AM, Degraeuwe P, Zimmermann LJ, Kramer BW et al (2019) Association of chorioamnionitis with bronchopulmonary dysplasia among preterm infants: a systematic review, meta-analysis, and metaregression. JAMA Netw Open 2(11):e1914611-e
Wang SH, Tsao PN (2020) Phenotypes of bronchopulmonary dysplasia. Int J Mol Sci 21(17)
Fernandez EF, Watterberg KL (2009) Relative adrenal insufficiency in the preterm and term infant. J Perinatol 29(Suppl 2):S44–S49
Goland RS, Wardlaw SL, Blum M, Tropper PJ, Stark RI (1988) Biologically active corticotropin-releasing hormone in maternal and fetal plasma during pregnancy. Am J Obstet Gynecol 159(4):884–890
Johnston RC, Faulkner M, Carpenter PM, Nael A, Haydel D, Sandman CA et al (2020) Associations between placental corticotropin-releasing hormone, maternal cortisol, and birth outcomes, based on placental histopathology. Reprod Sci 27(9):1803–1811
Watterberg KL, Scott SM, Naeye RL (1997) Chorioamnionitis, cortisol, and acute lung disease in very low birth weight infants. Pediatrics 99(2):E6
Chung HR (2014) Adrenal and thyroid function in the fetus and preterm infant. Korean J Pediatr 57(10):425–433
Watterberg KL, Scott SM (1995) Evidence of early adrenal insufficiency in babies who develop bronchopulmonary dysplasia. Pediatrics 95(1):120–125
Ng PC, Lam CW, Lee CH, Ma KC, Fok TF, Chan IH et al (2002) Reference ranges and factors affecting the human corticotropin-releasing hormone test in preterm, very low birth weight infants. J Clin Endocrinol Metab 87(10):4621–4628
Acknowledgements
We are grateful for the reviewers to assess our article.
Author information
Authors and Affiliations
Contributions
V. M. Koenders retrieved and assessed the data and wrote the main manuscript. A. Appels debated the results and made editorial comments. H. L. M. van Straaten and M. A. C. Hemels debated the results and reviewed the article. A. C. Dutman assessed all placentas and made editorial comments. All authors advised and reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The hospitals’ medical ethical committee approved the study.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koenders, V.M., Appels, A., van Straaten, H.L.M. et al. Postnatal corticosteroid response in neonates < 32 weeks and relation with placental pathology. Eur J Pediatr 182, 265–274 (2023). https://doi.org/10.1007/s00431-022-04672-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04672-9