Abstract
Purpose
To evaluate the effect of antenatal corticosteroids (AC) therapy on short- and long-term outcomes among very low birth weight preterm infants after histologic chorioamnionitis (HCA).
Methods
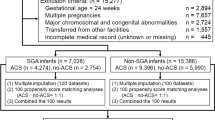
We performed a retrospective analysis of 5240 single very low birth weight (VLBW) infants born at 22 + 0 and 33 + 6 weeks of gestation between 2003 and 2007, who registered to the Neonatal Research Network Japan. The effects of AC therapy on mortality, neurodevelopmental outcomes at 3 years of age and neonatal morbidities were analyzed in the groups with or without HCA using logistic regression analysis.
Results
In the study subjects, 840 were with HCA, 2734 were without HCA, and 1666 were excluded without data for HCA. AC therapy was significantly associated with decreasing mortality before 3 years of age; [0.52 (0.32–0.86)], [odds ratio (95 % confidence intervals]. There were no differences between the two groups regarding neurodevelopmental outcomes, including cerebral palsy [0.90 (0.41–1.99)], development quotient <70 [0.93 (0.48–1.81)], visual impairment [0.46 (0.04–5.18)], and severe hearing impairment [4.00 (0.30–53.4)] in the group with HCA as well as without HCA. Regarding neonatal morbidities, AC therapy was associated with a lower incidence of respiratory distress syndrome [0.67 (0.50–0.91)], sepsis [0.62 (0.41–0.94)], late-onset adrenal insufficiency [0.62 (0.39–0.98)] and an increased incidence of chronic lung disease [1.62 (1.18–2.24)] in the group with HCA. In the group without HCA, AC therapy was associated with decreasing respiratory distress syndrome [0.60 (0.43–0.84)] and increasing chronic lung disease [1.34 (1.11–1.62)].
Conclusion
AC therapy is significantly associated with reduced mortality before 3 years of age in VLBW infants with HCA, but not with neurodevelopmental outcomes, which was same as the results found in infants without HCA. AC therapy is recommended for women with suspected chorioamnionitis, as well as those without chorioamnionitis.

Similar content being viewed by others
References
Brownfoot FC, Gagliardi DI, Bain E, Middleton P, Crowther CA (2013) Different corticosteroids and regimens for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 8:CD006764
Crowly P (2002) Prophylactic corticosteroids for preterm birth. Cochrane Database Syst Rev 4:CD000065
Crowly PA (1995) Antenatal corticosteroid therapy: a meta-analysis of the randomized trial. 1972–1994. Am J Obstet Gynecol 173:322–335
Antenatal corticosteroid therapy for fetal maturation (2011) ACOG Committee Opinion No. 475. American College of Obstetricians and Gynecologists. Obstet Gynecol 117:422–424
(1994) Effect of corticosteroids for fetal maturation on perinatal outcomes. NIH Consens Statement 12:1–24
Stutchfield P, Whitaker R, Russell I (2005) Antenatal steroids for term elective caesarean section research team. Antenatal betamethasone and incidence of neonatal respiratory distress after elective caesarian section: pragmatic randomized trial. BMJ 331:662
Murphy KE, Hannah ME, Willan AR, Hewson SA, Ohlsson A, Kelly EN et al (2008) Multiple course of antenatal corticosteroids for preterm birth (MACS): a randomized controlled trial. Lancet 372:2143–2151
Qublan H, Malkawi H, Hiasat M, Hindawi IM, Al-Taani MI, Abu- Khait SA et al (2001) The effect of antenatal corticosteroid therapy on pregnancies complicated by premature rupture of membranes. Clin Exp Obstet Gtnecol 28:183–186
Garite TJ, Rumney PJ, Briggs GG, Harding JA, Nageotte MP, Towers CV et al (1992) A randomized placebo-controlled trial of betamethasone for the prevention of respiratory distress syndrome at 24–28 weeks gestation. Am J Obstet Gynecol 166:646–651
Kent A, Lomas F, Hurrion E, Dahlstrom JE (2005) Antenatal steroids may reduce adverse neurological outcome following chorioamnionitis: neuro developmental outcome and chorioamnionitis in premature infants. J Paediatr Child Health 41:186–190
Baud O, Zupan V, Lacaze-Masmonteil T, Audibert F, Shojaei T, Thebaud B et al (2000) The relationships between antenatal management, the cause of delivery and neonatal outcome in a large cohort of very preterm singleton infants. BJOG 107:877–884
Goldenberg RL, Andrews WW, Faye-Petersen OM, Cliver SP, Goepfert AR, Hauth JC (2006) The Alabama Preterm Study: Corticosteroids and neonatal outcome in 23- to 32-week newborns with various markers of intrauterine infection. Am J Obstet Gynecol 195:1020–1024
Been JV, Rours IG, Kornelisse RF, Passos VL, Kramer BW, Schneider TAJ et al (2009) Histologic chorioamnionitis, fetal involvement, and antenatal steroids: effects on neonatal outcome in preterm infants. Am J Obstet Gynecol 201:587.e1–587.e8
Been JV, Degraeuwe PL, Kramer BW, Zimmermann LJI (2011) Antenatal steroids and neonatal outcome after chorioamnionitis: a meta-analysis. BJOG 118:113–122
Lahra MM, Jeffery HE (2004) A fetal response to chorioamnionitis is associated with early survival after preterm birth. Am J Obstet Gynecol 190:147–151
Oskoui M, Coutinho F, Dykeman J, Jette N, Pringsheim (2013) An Update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol 55:509–519
Kusuda S, Fujimura M, Sakuma I, Aotani H, Kabe K, Itani Y et al (2006) Morbidity and mortality of infants with very low birth weight in japan: center variation. Pediatrics 118:1130–1138
Papile L, Burstein J, Burstein R, Koffler H (1978) Incidence and evolution of subependymal and intraventricular hemorrhage; a study of infants with birth weights less than 1500. J Pediatr 92:5229–5534
Ng PC, Lee CH, Lam CWK, Ma KC, Fok TF, Chan IH et al (2004) transient adrenocortical insufficiency of prematurity and systemic hypotension in very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 89:119–126
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L et al (1978) Neonatal necrotizing enterocolitis. Therapeutic decision based upon clinical staging. Ann Surg 187:1–7
Kono Y, Mishita J, Yonemoto N, Kusuda S, Fujimura M (2011) Outcomes of very-low-birthweight infants at 3 years of age born in 2003–2004 in Japan. Pediatr Int 53(6):1051–1058
Mishita J (2000) Protocols for follow-up of high-risk infants. Perinat Med 30:1263–1272 (In Japanese)
Mori R, Kusuda S, Fujimura M (2011) Antenatal corticosteroids promote survival of extremely preterm infants born at 22–23 weeks of gestation. J Pediatr 159:110–114
Shimizu M, Sugano K, Kono Y, Yonemoto N (2010) Developmental characteristics of VLBW at 3 years according to antenatal steroids. J Jpn Soc Perinat Neonat Med 50:p614 (in Japanese)
Miyazaki K, Furuhashi M, Ishikawa K, Tamakoshi K, Ikeda T, Kusuda S, Fujimura M (2014) The effects of antenatal corticosteroids therapy on very preterm infants after chorioamnionitis. Arch Gtnecol Obstet 289:1185–1190
Moody DM, Brown WR, Challa VR, Blocks SM (1994) Alkaline phosphatase histochemical staining in the study of germinal matrix hemorrhage and brain vascular morphology in a very-low-birth-weight neonate. Pediatr Res 35:424–430
Volpe JJ (2001) Neurobiology of periventricular leukomalacia in the preterm infants. Pediatr Res 50:553–562
Lyon A (2000) Chronic lung disease of prematurity. The role of intra-uterine infection. Eur J Pediatr 159:798–802
Waffarn F, Davis EP (2012) Effects of antenatal corticosteroids on the hypothalamic-pituitary-adrenocortical axis of the fetus and newborn: Experimental finding and clinical considerations. Am J Obstet Gynecol 207:446–454
Blanc WA (1981) Pathology of the placenta, membranes, and umbilical cord in bacterial, fungal, and viral infections in man. In: Naeye RL, Kissane JM, Kaufman N (eds). Perinatal diseases. Internal Academy of Pathology Monograph. Baltimore: Williams & Wilkins pp. 67–132
Acknowledgments
We thank the institutions and representative physicians enrolled in the Neonatal Research Network Database in Japan, which include: Sapporo City General Hospital: S. Hattori; Kushiro Red Cross Hospital: A. Noro; Aomori Prefectural Central Hospital: T. Amizuka; Iwate Medical University: S. Chida; Sendai Red Cross Hospital: R. Takahashi; Akita Red Cross Hospital: H. Arai; Fukushima Medical University: T. Imamura; National Fukushima Hospital: N. Ujiie; University of Tsukuba: Y. Miyazono; Tsuchiura Kyodo General Hospital: J. Shimizu; Dokkyo Medical University: H. Suzumura; Jichi Medical University: Y. Kono; Saitama Children’s Medical Center: M. Shimizu; Saitama Medical University Saitama Medical Center: T. Kunikata; Gunma Children’s Medical Center: T. Fujiu; Kameda Medical Center: H. Sato; Tokyo Women’s Medical University Yachiyo Medical Center: T. Kondo; Tokyo Metropolitan Bokuto Hospital: T. Watanabe; Showa University: M. Aizawa; Tokyo Women’s Medical University: A. Uchiyama; Nihon University Itabashi Hospital: M. Makimoto; Teikyo University: J. Hoshi; Toho University: H. Yoda; Japan Red Cross Medical Center: Y. Kawakami; Aiiku Hospital: N. Ishii; National Center for Child Health and Development: Y. Ito; Kanagawa Children’s Medical Center: H. Itani; Yokohama City University Medical Center: K. Seki; Tokai University: M. Nomura; Kitazato University: M. Nowatari; Yamanashi Prefectural Central Hospital: A. Nemoto; Nagaoka Red Cross Hospital: O. Nagata; Niigata City Hospital: Y. Nagayama; Nagano Children’s Hospital: T. Nakamura; Shinshu University: M. Okada; Iida City Hospital: S. Nakata; National Nagano Hospital: E. Shimazaki; Saku General Hospital: T. Yoda; Toyama Prefectural Central Hospital: T. Hutatani; Ishikawa Prefectural Central Hospital: Y. Ueno; Fukui Prefectural Hospital: K. Iwai; Shizuoka Children’s Hospital: Y. Nakazawa; Seirei Hamamatsu General Hospital: S. Oki; Nagoya Red Cross First Hospital: C. Suzuki; National Mie Hospital: M. Bonno; Gifu Prefectural Central Hospital: Y. Kawano; Otsu Red Cross Hospital: K. Nakamura; Kyoto Red Cross First Hospital: N. Mitsufuji; Osaka Medical Center and Research Institute for Maternal and Child Health: J. Shiraishi; Osaka City General Hospital: H. Ichiba; Takatsuki Hospital: H. Minami; Yodogawa Christian Hospital: H. Wada; Kansai Medical University: A. Ohashi; Aizenbashi Hospital: K. Sumi; Nara Medical University: Y. Takahashi; Wakayama Prefectural Medical University: T. Okutani; Hyogo Prefectural Kobe Children’s Hospital: S. Yoshimoto; Tottori University: I. Nagata; Shimane Prefectural Central Hospital: E. Kato; Kurashiki Central Hospital: S. Watabe S; National Okayama Hospital: M. Kageyama; Hiroshima Prefectural Hospital: R. Fukuhara; Hiroshima City Hospital: M. Hayashitani; Yamaguchi Prefectural Medical Center: K. Hasegawa; National Kagawa Children’s Hospital: A. Ohta; Kagawa University: T. Kuboi; Ehime Prefectural Central Hospital: S. Akiyoshi; Kochi Health Sciences Center: K. Kikkawa; Tokushima University: T. Saijo; St. Mary’s Hospital: S. Shimokawa; Kitakyushu City Municipal Medical Center: N. Matsumoto; Kurume University: H. Kanda; Fukuoka University: E. Oota; National Kyushu Medical Center: G. Kanda; Kyushu University: M. Ochiai; National Nagasaki Medical Center: M. Aoki; Kumamoto City Hospital: Y. Kondo; Kumamoto University: M. Iwai; Oita Prefectural Hospital: K. Iida; Miyazaki University: T. Ikenoue; Kagoshima City Hospital: S. Ibara; Okinawa Chubu Hospital: M. Kohama.
Conflict of interest
This study was partly supported by a Grant from the Ministry of Health, Labor and Welfare, Japan (H16-kodomo-ippan-032, H19-kodomo-ippan-005, H22-jisedai-ippan-006).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miyazaki, K., Furuhashi, M., Ishikawa, K. et al. Long-term outcomes of antenatal corticosteroids treatment in very preterm infants after chorioamnionitis. Arch Gynecol Obstet 292, 1239–1246 (2015). https://doi.org/10.1007/s00404-015-3762-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3762-6