Abstract
Despite of growing evidence of the beneficial effects of placental transfusion techniques, there is no available sufficient data about their effects on vulnerable hemodynamics and myocardium of premature infants. The purpose of this work is to study ventricular functions and hemodynamics after applying different placental transfusion techniques, delayed cord clamping (DCC), cut cord milking (C-UCM), and intact cord milking (I-UCM). Sixty-four infants delivered whether by C-section or vaginal delivery were randomly assigned to undergo C-UCM (20–30 cm), I-UCM (3–4 strippings), and DCC (30–60 s). Functional echocardiography was done on day 1 and day 3 of life for 57 infants. Primary outcome variable was superior vena cava flow measurement in infants having placental transfusion in the first 24 h of life and between 64 and 72 h. Secondary outcomes were other echocardiographic and clinical hemodynamic parameters, and biventricular functions in those infants. Of a total 196 preterm infants ≤ 32 weeks delivered in the study period, from January 2021 to August 2021, 57 infants were eligible and survived till the second examination. They were randomly assigned to the three groups. Neonates randomly assigned to DCC had significantly higher superior vena cava flow and lower right ventricular systolic function in the first 24 h of life. This finding vanished at day 3. Neonates undergone different methods of placental transfusions had similar hemoglobin, admission temperature, and mean blood pressure in the first 24 h of life.
Conclusion: Despite their potential benefits, placental transfusions have shown to alter the hemodynamics and adversely affect myocardial function of premature neonates.
Trial registration: This trial was registered in the clinical trial gov NCT04811872.
What is Known: • Placental transfusion techniques might have benefits regarding prematurity- related morbidities and mortality. | |
What is New: • Placental transfusion might adversely affect the myocardium and alter hemodynamics in premature infants. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transition from fetal to neonatal life is the most complex life time event of a human being. Prematurity is one of the factors that hamper smooth transition and placental transfusion is one of the techniques being utilized to facilitate adequate transition [1]. In addition to providing adequate blood volume, and improving pulmonary flow, pulmonary vascular resistance, left ventricular preload, and tissue oxygenation, placental transfusion techniques provide various benefits that extend beyond the transition period such as decreasing the incidence of necrotizing enterocolitis (NEC), intraventricular hemorrhage (IVH), late onset sepsis, respiratory support days, inotropes and transfusion needs, and improving hemoglobin levels, iron stores, and neurodevelopmental outcome. Simply, placental transfusion might help in solving the challenging problems of prematurity, thereby improving the morbidities and mortality of preterm infants [2–11]. There are 3 types of placenta transfusions that are variable in timing, duration, and amount of blood transfused including cut-umbilical cord milking (C-UCM), intact umbilical cord milking (I-UCM), and delayed cord clamping (DCC) [12].
There is a paucity of studies that compare those different techniques regarding their effect on cardiovascular parameters. In the current work, we aim at studying the effect of those different techniques on hemodynamics and cardiac function of premature infants.
Aim of the work
Studying the effects of different placental transfusion techniques on the hemodynamics and cardiac functions of premature neonates ≤ 32 weeks.
Method
This three-armed parallel randomized control trial was conducted at the Alexandria University Maternity Hospital (AUMH), from January 2021 to August 2021. Approval from Institute Ethics Committee and parental consents were obtained. This trial was registered in the clinical trial gov NCT04811872.
Randomization and blinding
Randomization into the 3 groups was done using random permuted blocks of 6 and 9 size prepared by a person not involved in the study. Allocation into the three groups was done using serially numbered opaque and sealed envelopes by neonatology residents attending deliveries. The obstetricians were informed about plan of cord management before delivery. Blinding was not applicable at the stage of placental transfusion due to nature of the intervention, while at the stage of scanning, the operator was blinded to the state of placental transfusion.
Sample size calculation
A minimal total sample size of 57 patients (19 per group) is needed to detect a difference in mean superior vena cava flow (SVCF) among three groups of preterm infants with different methods of placental transfusion (intact umbilical cord milking, cut-umbilical cord milking, and delayed cord clamping) to study the effects of these methods on hemodynamics and neonatal outcomes in premature neonates with assumed group means of 93, 70, and 81 ml/kg/min, respectively, using group standard deviations of 24, 22, and 29 ml/kg/min, one-way ANOVA test, a significance level of 0.05, and 80% power (PASS program version 20) [13].
Study population
At the study period, 196 preterm infants ≤ 32 weeks were born in AUMH. This is a tertiary center that receives critically ill pregnant women from three governments. Only 64 were eligible and randomized to three groups. Patients with congenital anomalies (n = 13), placental or cord problems (n = 100), passed 24 h at time of first examination (n = 6), or lacked parental consents (n = 3) were excluded from the study. Of 64 infants who had one of placental transfusion methods and first imaging, fifty-seven infants lived till time of the second examination (Fig. 1).
Interventions
The study was designed to be carried out in 2 steps. As a first step, 64 pregnant women who are expected to deliver at or before 32 0/7 weeks were randomly assigned to 3 experimental groups: cut-umbilical cord milking (C-UCM), intact umbilical cord milking (I-UCM), and delayed cord clamping (DCC).
A cut-umbilical cord milking entails clamping and cutting a long segment (20–30 cm) of the umbilical cord immediately after birth and handing it over to the attending neonatologist, who will untwist the cord and milk the entire contents into the baby three times.
Intact umbilical cord milking (I-UCM): Umbilical cord milking was performed by holding the newborn between the maternal thighs. The cord was pinched between 2 fingers as close to the placenta as possible and milked to the infants’ side over a 2-s duration, then it was released and allowed to refill with blood for a brief 1- to 2-s pause between each milking motion. This was repeated for 3 times. Group of delayed cord clamping (DCC) in which infants were placed between the maternal thigh below the level of placenta and waiting 30–60 s before clamping the cord. The resident physician attending the delivery recorded the time elapsed from when the infant was delivered until the time the umbilical cord was clamped by the obstetrician to make sure that time exceeded 30 s [12].
Second step, a prospective cohort study, in which the operator was blinded to state of placental transfusions. A model of GE Vivid iq premium was used for functional echocardiography (FE). There was a GE 12S-RS probe with a frequency range of 5–11 MHz. An examination was performed using 2D, M-mode, color Doppler, continuous wave, and pulsed wave (PW) Dopplers. Doppler volumetric measurements of the superior vena cava flow, left ventricular output (LVO), and right ventricular output (RVO) were measured using Evans and Kluckow methodology [14, 15]. The velocity time integral (VTI) was calculated from the Doppler velocity tracings and averaged over 5 consecutive cardiac cycles in case of SVCF and 3 consecutive cycles in case of RVO and LVO estimations. The heart rate was measured from the peak-to-peak intervals of the Doppler velocity time signals. The duct was measured at its narrowest point, before its entry into the main pulmonary artery. Ductus arteriosus (DA) size, when indexed to the patient’s weight, > 1.4 mm/kg, together with left atrium to aortic root ratio (LA/AO) ratio were considered as markers of hemodynamically significant DA.
Left ventricular systolic and diastolic functions were assessed using fraction shortening (FS) and ejection fraction (EF), and mitral E/A ratio, respectively. Systolic right ventricular function was assessed using tricuspid annular plane systolic excursion (TAPSE) [16].
Cranial sonography was done with a GE 8C-RS probe with a frequency range of 3.5–10 MHz of A model GE Vivid iq premium. Patients were scanned regarding intraventricular hemorrhage (IVH) status and ACA (anterior cerebral artery) velocities; PSV (peak systolic velocity) and EDV (end diastolic velocity), and RI (resistive index) in the first 24 h [17]. On day 3, another cranial scan was performed to screen for IVH without measuring cerebral Doppler velocities.
Primary outcome variable was SVCF in the first day and at day 3 after the procedure of placental transfusion. Secondary outcome variables were other hemodynamic measures such as LVO, RVO, DA, LA/Ao ratio and ACA velocities, cardiac function parameters such as FS, TAPSE and E/A ratio, as well as clinical parameters such as IVH, admission temperature, initial hemoglobin, mean blood pressure, and heart rate on the first day of life. A second FE was conducted on the third day of life for all living patients.
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. The Kolmogorov–Smirnov test was used to verify the normality of distribution. Qualitative data were described using number and percent. Quantitative data were described using range (minimum and maximum), mean, and standard deviation, median and interquartile range (IQR). Significance of the obtained results was judged at the 5% level. Chi-square test, Monte Carlo correction, F-test (ANOVA), and Kruskal Wallis test were used for comparison between the three groups regarding different variables.
Results
Among the 64 infants randomly assigned to the three groups, 19 were assigned to the I-UCM group, 23 to the C-UCM group, and 22 to the DCC group. Seven patients did not survive to the second examination on third day of life (Fig. 1). In all 57 patients, a functional echocardiography was conducted between 6 and 22 h, and a second one was performed between 64 and 72 h of life. In DCC group, cord clamping was delayed for a period of 32–50 s, with a median of 43 s and a mean of 41.32 ± 5.7 s.
In Table 1, no significant differences were found between the studied groups in terms of demographic characteristics, maternal risk factors, or resuscitation data. Vital signs, laboratory parameters, ventilation needs, and inotropic support did not differ significantly between studied groups (Table 2).
No significant differences were found among the three groups regarding PDA size, direction, and being hemodynamically significant. SVCF, the primary outcome, was significantly higher in the DCC group than I-UCM and C-UCM groups with mean values 120.29 ± 43.11, 83.5 ± 34.83, and 97.44 ± 30.27, respectively, p value 0.013 (Table 3). While after day 3, no significant differences were found among the three studied groups (Table 4).
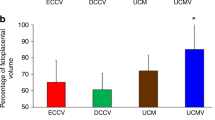
TAPSE was significantly lower in DCC than in the other two groups. The second imaging, however, did not reveal any significant differences. Other echocardiographic parameters did not show significant differences between the groups in either scan. Table 5 shows no significant differences among studied groups regarding IVH occurrence, ACA-RI, and cerebral blood flow velocities (PSV and EDV) in the first 24 h. On the second cranial scan, only two patients had progressed from IVH grade I to IVH grade III in the cut-UCM group, although there were still no significant differences among the three groups.
For DCC and intact UCM, there were 4 patients who died before discharge in each group, and for cut UCM there were three patients who died before discharge. In DCC group, the time to death was significantly shorter, however, the three groups did not differ significantly in term of pre-discharge mortality (S-Tables 2 and 3). Days to discharge were not significantly different between the studied groups (S-Table 1). S-Tables 4, 5, 6, 7, 8 and 9 show comparisons between echocardiographic parameters on day 1 and day 3 in each of the three groups.
Discussion
A comparison of hemodynamics and cardiac functions in preterm infants with different placental transfusion techniques, I-UCM, C-UCM, and DCC, is presented in this study.
While placental transfusions have many benefits, the main disadvantage is the rapid transfusions provided by the 3 techniques and the possible changes in hemodynamics in vulnerable premature infants. This may not allow enough time for smooth transition and adaptation of cardiovascular system, especially in cord milking groups.
Another challenge that could be faced with cut cord milking is that blood would be transfused after taking the first breath and the available length of the cord segment to be milked might not be sufficient. However, this technique might be a good alternative if the two other techniques could not be done or missed.
No significant differences were found among studied groups in terms of demographics. In the DCC group, the type of delivery or anesthesia might affect the contractions of the uterus, and thus the amount of blood transfused. None of the studied groups demonstrated significant differences for those variables.
Katheria et al. found no differences in pulse oxygen saturation and heart rate between the UCM and DCC groups of infants delivered by cesarean section; their blood pressure was higher in UCM group in the first 15 h of life [13]. According to the present study, no significant differences were detected between the three studied groups in mean blood pressure, heart rate, or saturation in the first 24 h, nor were there any significant differences in temperature at admission. This might be attributed to short duration of procedure in intact cord milking, transfusion of warm blood in the DCC, and the use of servo-controlled heater during cut cord milking.
Whether different techniques of placental transfusion have similar effect on hemoglobin (Hb) level is point of debate in various studies. Kilicdag and Shirk showed no significant differences regarding Hb level between C-UCM and I-UCM, and DCC and I-UCM, respectively [18, 19]. Katheria et al. showed significant difference in Hb levels between DCC and I-UCM in preterm infants born by C-section, in which infants in DCC group are expected to have lower Hb levels owing to lack of effective uterine contractions in their mothers [13]. In the current work, the mean values of hemoglobin in the three groups were more than 15 g/dl. Although the results were not statistically significant, the I-UCM group had a tendency toward higher hemoglobin levels and fewer newborns with hemoglobin concentrations below 15 mg/dl, which also suggests that I-UCM may be a better choice in premature neonates.
An observation was made in the DCC group that 29 weeker male patient had the lowest initial hemoglobin level (10 mg/dl) and the highest WBCs (80 × 103 µl), the umbilical cord was noted as being pale and whitish in color and had a very little amount of blood to be transfused at birth. However, the patient was not excluded because he had none of the exclusion criteria. Right IVH grade I was noted on day 1 with SVC was 171.7 ml/kg/min, LVO was 397 ml/kg/min, RVO 409 ml/kg/min ductal shunt was unrestricted on the first day of life, and the day 3-SVC flow decreased to 90.3 ml/kg/min on the third day after receiving packed cell transfusion on day 2.
The lowest SVCF is usually recorded around 3–12 h after birth, with a gradual increase thereafter until 24–48 h after birth. After the transitional phase, the SVC flow remains relatively stable at 85–90 ml/kg/min in preterm infants [20]. In the first 24 h, placental transfusion might be one of principal factors affecting hemodynamics and myocardial function in the study population. Metrics of the 2nd scan, on day 3 might represent partial recovery from effect of placental transfusion and might be a reflection of other postnatal factors such as sepsis-related illness, mechanical ventilation, and the use of inotropes [21].
SVCF was significantly higher in the DCC group in the first 24 h after birth than I-UCM and C-UCM groups. This difference disappeared on day 3. The relative increase in SVCF in the 1st 24 h might played a role in lack of occurrence of catastrophic IVH in the 3 studied group in first day of life. Moreover, only 2 patients developed IVH grade I in the DCC group with significantly higher mean values of SVCF. SVCF is a measure of systemic blood flow (SBF) as well as RVO and LVO. Therefore, patients in the DCC group tended to have higher RVO and LVO.
In the current study, we used TAPSE, and EF and FS to evaluate systolic function of right and left ventricles, respectively. Left ventricular diastolic function was evaluated using E/A ratio.
There is scarcity of data about normative and reference values of echocardiographic parameters in preterm infants [22]. Noori et al. in their observational study on 29 preterm infants with gestational age = 26.2 ± 1.5 weeks reported that average FS was 34% ± 5% (range 23–48%) in the first 3 postnatal days in hemodynamically stable preterm infants [23]. Left ventricular dysfunction can be classified into the following: mild (FS 20–25%), moderate (FS 15–19%), and severe (FS ≤ 14%) [22]. In the current work, 8/19, 8/19, and 10/19 patients had FS less than 23% in C-UCM, I-UCM, and DCC, respectively. However, 2 out of those 26 patients only needed inotropic support and only three of them have LVO < 120 ml/kg /min; the normal LVO range in neonates is 150–400 ml/kg/min [24]. This might indicate that normative values might need be adjusted to a lower level in premature infants. It is also probably that rapid autotransfusion by the three placental transfusion techniques might have affected left ventricle (LV) systolic function. Taking into consideration that FS and EF measured by linear left ventricular minor-axis dimensions reflect movement of region of LV along the cursor line of M-mode, so it underestimates the entire LV contractile function.
The LV E/A ratio values were normal in the three study groups since the lower accepted value is 0.7:1 in premature infants [25] and no significant differences were found between the three groups. TAPSE was significantly lower in DCC group despite still being within physiological range of premature infants and this difference disappeared on day 3. The lowest accepted value for TAPSE in premature neonates is 4 mm [26]. This finding is similar to what happens in recipient fetus in twin to twin (TTT) syndrome with more affection of right ventricle by volume overload. After fetoscopic laser coagulation of the connecting vessel, rapid normalization of cardiac function occurs [27].
Early and rapid volume expansion might have detrimental effect on ventricular functions in preterm infants [28]. The immature myocardium has limited ability to tolerate over transfusion or rapid transfusions with decreased contractile reserve, as only 30% of the fetal myocardium contains contractile mass, in contrast to 60% in the adult [29]. The right ventricle (RV) is more vulnerable to transfusion intolerance. RV has a higher resting tension than the adult RV, leading to lower ventricular compliance in utero and early neonatal life [29]. The coronary flow is related to pressure difference between aortic root to the right atrium (RA). When RA pressure escalates, thus, the flow in right coronary artery might be insufficient leading to transient wall ischemia [30]. In the current work, DCC patients’ right ventricles were affected more than the other 2 groups. This could have 2 possible explanations: first, the amount of transfused blood might be higher in DCC patients. DCC for 30–45 s in preterm infants resulted in up to 28 ml/kg increase in blood volume, while C-UCM with 30-cm cord segment and I-UCM for 4 times may increase blood volume by 8 ml/kg and 14 ml/kg, respectively [31]. Second, patients of DCC group have lower birthweight and gestational age (Table 1) and TAPSE values increase linearly with gestational age and birth weight [32]. Yao et al. suggested that late cord clamping, by allowing a sizable placental transfusion, appeared to affect adversely the LV performance of the neonates [33].
Among neonatologists, there is still no consensus regarding when the umbilical cord should be clamped in preterm infants. Two systematic reviews of 11,736 preterm infants, encompassing more than 100 studies, found that delayed cord clamping was associated with lower mortality than immediate cord clamping [34, 35]. On the other hand, a large multicenter RCT for 1566 preterm infants found that delayed cord clamping did not result in a lower incidence of death or major morbidity at 36 weeks of gestation when compared to immediate cord clamping [36]. While in their long-term follow-up analysis of this mega multicenter RCT revealed that clamping the umbilical cord ≥ 60 s after birth resulted in a 30% reduction in relative mortality without affecting the major disability [37]. In the current study, there were no differences regarding predischarge mortality among the study groups, but the DCC group had lower days to death than the other 2 groups. The small sample size was a major limitation that hampers taking this result into consideration, especially that the DCC group had lower GA and birth weight than the other two groups.
Limitations
In our trial, we were limited by the lack of an immediate cord clamping group. This might justify absence of significant differences in most of echocardiographic parameters between the three evaluated groups, because these three approaches resulted in increased SBFs and altered hemodynamics. It was also important to note that the sample size of the three groups was relatively small in the present study.
The study was also limited by the inability to measure the SVC flow and cardiac output more than two times, since the SVC flow tends to vary widely during the first days of life. A further limitation of the study was the fact that no actions were taken when the SVC flow decreased, as the study was designed as a prospective cohort study, regarding the imaging step. We did not evaluate diastolic function of RV that might be affected by placental transfusions more than diastolic function left ventricle.
Conclusion
Although there are benefits of different placental transfusion techniques, they appear to alter hemodynamics and myocardial function in premature neonates ≤ 32 weeks. Use of delayed cord clamping technique results in significantly increased SVCF and decreased right ventricular systolic function in premature neonates in their 1st 24 h of life. This effect disappeared on day 3. Therefore, although DCC is preferred method because its preferable effect on SVCF in the 1st 24 h, patient’s myocardial function should be monitored. It is possible that the myocardium, especially in patients with delayed cord clamp, may be more susceptible to potential adverse cardiovascular effect than premature neonates without placental transfusion.
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Wu TW, Azhibekov T, Seri I (2016) Transitional hemodynamics in preterm neonates: clinical relevance. Pediatr Neonatol 57(1):7–18. https://doi.org/10.1016/j.pedneo.2015.07.002 (Epub 2015 Aug 29 PMID: 26482579)
Hooper S, Kluckow M (2019) Cardiorespiratory effects of delayed cord clamping. In: Seri I, Kluckow M, Polin RA (eds) Hemodynamics and Cardiology: Neonatology Questions and Controversies, 3rd edn. Elsevier, Mosby, pp 67–82. https://doi.org/10.1016/B978-0-323-53366-9.00004-1
Mercer JS, Vohr BR, McGrath MM, Padbury JF, Wallach M, Oh W (2006) Delayed cord clamping in very preterm infants reduces the incidence of intraventricular hemorrhage and late-onset sepsis: a randomized, controlled trial. Pediatrics 117(4):1235–1242. https://doi.org/10.1542/peds.2005-1706 (PMID: 16585320; PMCID: PMC1564438)
Mercer JS, Erickson-Owens DA, Vohr BR, Tucker RJ, Parker AB, Oh W et al (2016) Effects of placental transfusion on neonatal and 18 month outcomes in preterm infants: a randomized controlled trial. J Pediatr 168:50–5.e1. https://doi.org/10.1016/j/jpeds.2015.09.068
Oh W, Fanaroff AA, Carlo WA, Donovan EF, McDonald SA, Poole WK, Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network (2011) Effects of delayed cord clamping in very-low-birth-weight infants. J Perinatol 31(Suppl 1):S68–S71. https://doi.org/10.1038/jp.2010.186 (PMID: 21448208; PMCID: PMC3327157)
Rabe H, Wacker A, Hülskamp G, Hörnig-Franz I, Schulze-Everding A, Harms E, Cirkel U, Louwen F, Witteler R, Schneider HP (2000) A randomised controlled trial of delayed cord clamping in very low birth weight preterm infants. Eur J Pediatr 159(10):775–777. https://doi.org/10.1007/pl00008345 (PMID: 11039135)
Das B, Sundaram V, Kumar P, Mordi WT, Dhaliwal LK, Das R (2018) Effect of placental transfusion on iron stores in moderately preterm neonates of 30–33 weeks gestation. Indian J Pediatr 85(3):172–178. https://doi.org/10.1007/s12098-017-2490-2 (Epub 2017 Nov 4 PMID: 29101631)
Garg B, Bansal A (2017) Role of delayed cord clamping in prevention of necrotizing enterocolitis in preterm neonates: a systematic review. J Matern Fetal Neonatal Med 32:1–23. https://doi.org/10.1080/14767058.2017.1370704
Kinmond S, Aitchison TC, Holland BM, Jones JG, Turner TL, Wardrop CA (1993) Umbilical cord clamping and preterm infants: a randomised trial. BMJ 306(6871):172–175. https://doi.org/10.1136/bmj.306.6871.172 (PMID: 8443480; PMCID: PMC1676623)
Straňák Z, Feyereislová S, Korček P, Dempsey E (2018) Placental transfusion and cardiovascular instability in the preterm infant. Front Pediatr 27(6):39. https://doi.org/10.3389/fped.2018.00039 (PMID: 29535993; PMCID: PMC5835097)
Lodha A, Shah PS, Soraisham AS et al (2019) Association of deferred vs immediate cord clamping with severe neurological injury and survival in extremely low-gestational-age neonates. JAMA Netw Open 2(3):e191286. https://doi.org/10.1001/jamanetworkopen.2019.1286
Katheria AC, Lakshminrusimha S, Rabe H, McAdams R, Mercer JS (2017) Placental transfusion: a review. J Perinatol 37(2):105–111. https://doi.org/10.1038/jp.2016.151 (Epub 2016 Sep 22. PMID: 27654493; PMCID: PMC5290307)
Katheria AC, Truong G, Cousins L, Oshiro B, Finer NN (2015) Umbilical cord milking versus delayed cord clamping in preterm infants. Pediatrics 136(1):61–69. https://doi.org/10.1542/peds.2015-0368 (PMID: 26122803; PMCID: PMC4485011)
Kluckow M, Evans N (2000) Superior vena cava flow in newborn infants: a novel marker of systemic blood flow. Arch Dis Child Fetal Neonatal Ed 82(3):F182–F187
Evans N, Kluckow M (1996) Early determinants of right and left ventricular output in ventilated preterm infants. Arch Dis Child Fetal Neonatal Ed 74(2):F88–F94
Noori S (2018) Assessment of systolic, diastolic, and global cardiac function. In: Siassi B, Noori S, Acherman RJ, Wong PC (eds) Practical neonatal echocardiography. McGraw Hill. https://accesspediatrics.mhmedical.com/content.aspx?bookid=2497§ionid=203646736. Accessed 17 Sept 2022
Noori S (2018) Application of pulsed wave and continuous-wave Doppler in the assessment and measurement of cardiac and systemic blood flow. In: Siassi B, Noori S, Acherman RJ, Wong PC (eds) Practical neonatal echocardiography. McGraw Hill. https://accesspediatrics.mhmedical.com/content.aspx?bookid=2497§ionid=203646543. Accessed 17 Sept 2022
Kilicdag H, Karagun BS, Antmen AB, Candan E, Erbas H (2021) Umbilical cord management in late preterm and term infants: a randomized controlled trial. Am J Perinatol 39:1308–1313
Shirk SK, Manolis SA, Lambers DS, Smith KL (2019) Delayed clamping vs milking of umbilical cord in preterm infants: a randomized controlled trial. Am J Obstet Gynecol 220(5):482
de Waal K, Kluckow M (2020) Superior vena cava flow: role, assessment and controversies in the management of perinatal perfusion. Semin Fetal Neonatal Med 25(5):101122. https://doi.org/10.1016/j.siny.2020.101122 (Epub 2020 May 21. PMID: 32467039)
Evans N (2006) Assessment and support of the preterm circulation. Early Hum Dev 82(12):803–810. https://doi.org/10.1016/j.earlhumdev.2006.09.020 (Epub 2006 Oct 31 PMID: 17079097)
Tissot C, Singh Y, Sekarski N (2018) Echocardiographic evaluation of ventricular function-for the neonatologist and pediatric intensivist. Front Pediatr 4(6):79. https://doi.org/10.3389/fped.2018.00079 (PMID: 29670871; PMCID: PMC5893826)
Noori S, Wu TW, Seri I (2013) pH effects on cardiac function and systemic vascular resistance in preterm infants. J Pediatr 162(5):958–63.e1. https://doi.org/10.1016/j.jpeds.2012.10.021 (Epub 2012 Nov 16 PMID: 23164307)
Singh Y, Tissot C, Fraga MV, Yousef N, Cortes RG, Lopez J, Sanchez-de-Toledo J, Brierley J, Colunga JM, Raffaj D, Da Cruz E, Durand P, Kenderessy P, Lang HJ, Nishisaki A, Kneyber MC, Tissieres P, Conlon TW, De Luca D (2020) International evidence-based guidelines on Point of Care Ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care 24(1):65. https://doi.org/10.1186/s13054-020-2787-9 (PMID: 32093763; PMCID: PMC7041196)
Skinner J, Alverson D, Hunter S (2000) Echocardiography for the neonatologist. Churchill Livingstone, London (Internet resource)
Leone TA (2018) Persistent pulmonary hypertension in newborn infants: assessment of pulmonary artery pressure. In: Siassi B, Noori S, Acherman RJ, Wong PC (eds) Practical neonatal echocardiography. McGraw Hill. https://accesspediatrics.mhmedical.com/content.aspx?bookid=2497§ionid=203647155
Van Mieghem T, Lewi L, Gucciardo L, Dekoninck P, Van Schoubroeck D, Devlieger R, Deprest J (2010) The fetal heart in twin-to-twin transfusion syndrome. Int J Pediatr 2010:379792. https://doi.org/10.1155/2010/379792 (Epub 2010 Aug 8. PMID: 20811613; PMCID: PMC2929591)
Osborn DA, Evans N (2004) Early volume expansion for prevention of morbidity and mortality in very preterm infants. Cochrane Database Syst Rev 2004(2):CD002055. https://doi.org/10.1002/14651858.CD002055.pub2. PMID: 15106166; PMCID: PMC7025803
Di Maria MV, Abman SH (2015) The neonatal transition of the right ventricle. In: Voelkel NF, Schranz D (eds) The right ventricle in health and disease, 1st edn. Springer Nature, Humana, New York, NY. https://doi.org/10.1007/978-1-4939-1065-6
Rios DR, Lapointe A, Schmolzer GM, Mohammad K, VanMeurs KP, Keller RL, Sehgal A, Lakshminrusimha S, Giesinger RE, Newborn Brain Society Guidelines and Publications Committee (2021) Hemodynamic optimization for neonates with neonatal encephalopathy caused by a hypoxic ischemic event: physiological and therapeutic considerations. Semin Fetal Neonatal Med 26(4):101277. https://doi.org/10.1016/j.siny.2021.101277 (Epub 2021 Aug 12; PMID: 34481738)
McAdams RM, Fay E, Delaney S (2018) Whole blood volumes associated with milking intact and cut umbilical cords in term newborns. J Perinatol 38(3):245–250. https://doi.org/10.1038/s41372-017-0002-x (Epub 2017 Dec 12 PMID: 29234147)
Koestenberger M, Nagel B, Ravekes W, Urlesberger B, Raith W, Avian A, Halb V, Cvirn G, Fritsch P, Gamillscheg A (2011) Systolic right ventricular function in preterm and term neonates: reference values of the tricuspid annular plane systolic excursion (TAPSE) in 258 patients and calculation of Z-score values. Neonatology 100(1):85–92. https://doi.org/10.1159/000322006 (Epub 2011 Jan 26 PMID: 21273793)
Yao AC, Lind J (1977) Effect of early and late cord clamping on the systolic time intervals of the newborn infant. Acta Paediatr Scand 66(4):489–493. https://doi.org/10.1111/j.1651-2227.1977.tb07932.x (PMID: 899765)
Jasani B, Torgalkar R, Ye XY, Syed S, Shah PS (2021) Association of umbilical cord management strategies with outcomes of preterm infants: a systematic review and network meta-analysis. JAMA Pediatr 175(4):e210102. https://doi.org/10.1001/jamapediatrics.2021.0102 (Epub 2021 Apr 5. PMID: 33683307; PMCID: PMC7941254)
Rabe H, Gyte GM, Díaz-Rossello JL, Duley L (2019) Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev 9(9):CD003248. https://doi.org/10.1002/14651858.CD003248.pub4 (PMID: 31529790; PMCID: PMC6748404)
Tarnow-Mordi W, Morris J, Kirby A, Robledo K, Askie L, Brown R, Evans N, Finlayson S, Fogarty M, Gebski V, Ghadge A, Hague W, Isaacs D, Jeffery M, Keech A, Kluckow M, Popat H, Sebastian L, Aagaard K, Belfort M, Pammi M, Abdel-Latif M, Reynolds G, Ariff S, Sheikh L, Chen Y, Colditz P, Liley H, Pritchard M, de Luca D, de Waal K, Forder P, Duley L, El-Naggar W, Gill A, Newnham J, Simmer K, Groom K, Weston P, Gullam J, Patel H, Koh G, Lui K, Marlow N, Morris S, Sehgal A, Wallace E, Soll R, Young L, Sweet D, Walker S, Watkins A, Wright I, Osborn D, Simes J, Australian Placental Transfusion Study Collaborative Group (2017) Delayed versus immediate cord clamping in preterm infants. N Engl J Med 377(25):2445–2455. https://doi.org/10.1056/NEJMoa1711281 (Epub 2017 Oct 29. PMID: 29081267)
Robledo KP, Tarnow-Mordi WO, Rieger I, Suresh P, Martin A, Yeung C, Ghadge A, Liley HG, Osborn D, Morris J, Hague W, Kluckow M, Lui K, Soll R, Cruz M, Keech A, Kirby A, Simes J, APTS Childhood Follow-up Study collaborators (2022) Effects of delayed versus immediate umbilical cord clamping in reducing death or major disability at 2 years corrected age among very preterm infants (APTS): a multicentre, randomised clinical trial. Lancet Child Adolesc Health 6(3):150–157. https://doi.org/10.1016/S2352-4642(21)00373-4 (Epub 2021 Dec 8. Erratum in: Lancet Child Adolesc Health. 2022 Jan 21;: PMID: 34895510)
Acknowledgements
We are grateful and thankful all the patients, parents, and staff of the NICU of Alexandria University that participated in the study.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
Marwa Mohamed Farag conceived of the presented idea. Ali Mohamed Abd-Almohsen, Heba Ibrahim, and Marwa M. Farag worked out all of the technical and medical details. Heba Idris Abudeif Mohammed Ibrahim collected the data. Marwa M. Farag and Heba Idris Abudeif Mohammed Ibrahim verified the analytical methods. Heba Idris Abudeif Mohammed Ibrahim, Marwa Farag, and Mohamed Alaa Eldin Hassan Thabet contributed in interpretation of results. Marwa Farag wrote the first draft of the manuscript. Mohamed Alaa Eldin Hassan Thabet supervised the findings of this work. All authors provided critical feedback and helped shape the research, analysis, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol has been approved by the Research Ethics Committee of Alexandria faculty of medicine. Approval no. is 0106459 in. IRB no. is 00012098 and FWA no. is 00018699. Two written informed consents were obtained from parents or authorized legal representatives of all newborns who participated in the study for having placental transfusion and publication of anonymous patients’ data.
Consent for publication
Informed consent was obtained from parents or authorized legal representatives of all newborns who participated in the study for publication of anonymous patients’ data.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Farag, M.M., Thabet, M.A.E.H., Abd-Almohsen, A.M. et al. The effect of placental transfusion on hemodynamics in premature newborns: a randomized controlled trial. Eur J Pediatr 181, 4121–4133 (2022). https://doi.org/10.1007/s00431-022-04619-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04619-0