Abstract
Recent literature has shown that sleep patterns are shaped during the first years of life, playing a relevant role in children’s functioning. We focused on comparing sleep patterns in infants and toddlers in Spain before and during COVID-19 home confinement to assess the immediate impact on sleep patterns. We compared data from two cross-sectional surveys from parents of 1658 children three to 36 months of age from Spain. One conducted before COVID-19 (2017–2018, n = 1380) and another during COVID-19 pandemic (March–May of 2020, n = 254). We used an internet self-administrated questionnaire using the Brief Infant Sleep Questionnaire (BISQ) criteria in both surveys. During confinement, infants and toddlers went to sleep later (median bedtime 21:30 before confinement vs. 21:36 during confinement (p = 0.004)). More infants and toddlers showed longer sleep latencies (> 30 min) during confinement median 33.9% versus 12.3% (p < 0.001). Based on the recommended BISQ criteria, we observed an increase in poor sleepers meeting at least one criterion of inadequate patterns during confinement (p < 0.001). Parental perception of a child’s sleep as problematics were 39.4% and 44.1% (adjusted p = 0.363) before and under lockdown, respectively.
Conclusion: Home confinement generally affected infant’s and toddler’s sleep patterns negatively; however, parents did not report worse perception of sleep quality of their children. Follow-up studies can help understand the potential long-term effects of the COVID-19 pandemic on sleep patterns.
What is Known: • Adequate sleep patterns in infants and toddlers are relevant as they are linked to proper and long-term social-emotional development as well as adequate daytime functioning. • Regarding sleep patterns in paediatrics during the COVID pandemic, recent literature has described an increase in total daily sleep time as well as more exposure to screens in children and adolescents, providing evidence of immediate collateral consequences of the COVID-19 outbreak. | |
What is New: • Comparing sleep patterns in two samples of infants and toddlers in Spain before and during COVID-confinement, we found later bedtimes as well as a significant increase in infants’ and toddlers’ sleep latency by >30 min during confinement. • Parental self-reported questionnaire during COVID-19 home confinement reported an overall worsening of their children’s sleep based on the BISQ criteria. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep patterns change rapidly across the earliest years of life and play an important role in children’s daytime functioning. There is a growing interest in determining those factors influencing children’s sleep development (both intrinsic (i.e., child characteristics) and extrinsic (i.e., environmental input)) [1, 2]. Children sleep patterns might rapidly take a turn-over in light of external factors such the current public health pandemic due to COVID-19 outbreak. On March 14, 2020, in response to the first wave outbreak, the Spanish Government imposed one of the most stringent lockdowns in Europe (BOE-A-2020–3692 https://www.boe.es/eli/es/rd/2020/03/14/463) especially for children, as an emergency measure to prevent further spreading of the infection. After 6 weeks of strict home confinement, Spanish minors were permitted to leave the house for one hour within allotted time slots and half-mile radius. This sudden unexpected circumstance meant having to adapt to a new reality for both adults and children. Previous literature has found that during non-school period, children tend to be physically less active, have longer screen time, irregular sleep patterns, and less adequate diets, resulting in weight gain and a loss of cardiorespiratory fitness [3, 4].
In these recent past months, there is growing evidence being published about the impact of this pandemic on children’s health, sleep patterns and psychological development. A meta-analysis on the psychological and behavioural impact of home confinement and quarantine measures during COVID-19 pandemic in 22.996 children/adolescents from diverse European countries, Asian countries, and South America showed that 79.4% of children were affected negatively by the pandemic and quarantine; at least 21.3% of them had a sleep disturbance [5]. A cross-sectional study carried out during the quarantine on 1143 Spanish and Italian parents of children aged three to 18 years old found that 85.7% of the parents perceived changes in their children’s emotional state and behaviours. The most frequent symptoms were difficulty concentrating (76.6%), boredom (52%), irritability (39%), restlessness (38.8%), nervousness (38%), feelings of loneliness (31.3%), uneasiness (30.4%), and worries (30.1%). Spanish parents reported more symptoms than Italians ones [6].
When analyzing preschoolers’ sleep patterns during home confinement, a recent cross-sectional study [7] on 412 infants and toddlers 0–35 months from several mainly European countries described an acute decrease in sleep quality. At follow-up (1 and 2 months later), this effect rebounded to the level reported for the period before the home confinement. Caregiver’s stress level was also identified as a substantial risk factor determining lower sleep quality [7]. Another study based in China [8] evaluated 1619 preschoolers (aged 4–6 years) sleep patterns based on the completed the Children’s Sleep Habit Questionnaire (CSHQ), comparing the findings to a similar sample recruited in 2018. Confined preschoolers showed later bedtimes and wake times, longer nocturnal and shorter nap sleep durations, comparable 24-h sleep duration, and fewer caregiver-reported sleep disturbances [8]. Another study carried out in Japan [9] compared cross-sectional data from online surveys describing the sleep behaviour of infants and caregivers in two time slots (before and during the COVID-19 pandemic) finding no significant differences in wake-up times, bedtimes, or nocturnal sleep times (p = 0.613). However, confined infants showed a decrease in total sleep time and media use increased significantly [9].
The aim of this work is to compare two similar samples of infant and toddlers in Spain three to 36 months of age (before and during COVID-19 confinement) in order to identify possible sleep pattern changes related to the COVID-19 confinement. We hypothesize to find a negative impact on infants and toddlers sleep patterns during the COVID-19 confinement.
Methods
We analyzed a repeated cross-sectional survey of parents who reported having a healthy infant/toddler between 3 and 36 months of age in Spain. One conducted before COVID-19 confinement (2017–2018) [10] and another conducted during the strict home confinement of the first wave of COVID-19 (March–May of 2020). We used an internet self-administrated questionnaire assessing sleep patterns using the Spanish validated Brief Infant Sleep Questionnaire (BISQ) criteria [11, 12] in both surveys. The BISQ comprises 14 items: 4 on the demographic characteristics of the child and 10 on sleep habits. There are 4 multiple-choice single-answer questions and 6 open-ended questions about the timing and duration of sleep. This questionnaire has been described as a robust instrument of proven reliability and validity, easy to use and brief, and thus adequate as a screening tool [13, 14].The sample recruitment, the inclusion, and exclusion criteria as well as the variables measured and analyses carried out mirrored our previous study in order to be able to perform adequate comparisons between both our samples [10].
Participants
We compared 1634 infants and toddlers recruited in two different stages (1380 before confinement (February 2017 to February 2018) and 254 during confinement (March–May 2020). Both samples included healthy Spanish children between ages 3 to 36 months. Data were collected from a digital online questionnaire available within a free-access website. Parents were invited to participate either during their child’s paediatric follow-up visit at Hospital Universitari General de Catalunya or through online free access forums about parenting topics.
Measures
Parents completed a self-reported 47 item online questionnaire, which included the Spanish validated Brief Infant Sleep Questionnaire (BISQ-E) [12] (based on the BISQ [11]. Other items included in the questionnaire were demographic data and general family habits; however, this complementary data was not used in the current study analysis.
In order to understand developmental patterns and resembling the original BISQ methodology [11], children were grouped in five age ranges as initially done in the BISQ validation. Group 1 was ages 3 to 6 months; group 2, ages 7 to 12 months; group 3, ages 13 to 18 months; group 4, ages 19 to 24 months; and group 5, ages 25 to 36 months.
Based on the BISQ criteria established for clinically classifying poor sleepers [11] (more than three awakenings a night, nocturnal awakenings longer than 1 h and, a total sleep time in the 24-h period of less than 9 h), where any of these indications in a child suggests the need for further follow-up, we used this same criterion for defining problematic sleep behaviour. Parental perception of sleep quality was also included in the analysis as a variable present in the original BISQ [11].
Procedure
The Institutional Ethics Review Board at General University of Catalunya Hospital and Catalonia International University, Barcelona, approved this study. All users provided consent to the inclusion of their data in the present research study and were able to decline participation at all times. The researchers provided users with contact information should they have any questions, concerns, or desire to withdraw consent. Data from second cross-sectional sample were collected from April 2020 to June 2020.
For this study, a self-registered website domain was created called www.epison.es where the questionnaire was uploaded and encrypted. The completion of the questionnaire was voluntary, and parents were not offered any compensation for their participation. Inclusion criteria were parents with infants and toddlers from 3 to 36 months of age residing in Spain. Exclusion criteria were limited to literacy in Spanish language.
Analyses
The variables were described with frequency and percentage for the qualitative variables, the mean and standard deviation for the quantitative normal-distributed variables, and median and interquartile range for the quantitative not normally distributed variables.
To compare two groups (before and during confinement, for example), a prevalence ratio was calculated for qualitative variables, with their confidence interval and p-value. Mann–Whitney test was performed for quantitative not normally distributed variables.
The confidence intervals were calculated with a level of confidence of 95%. The tests were considered significant when the p-value was under 0.05. The normality was tested with the Shapiro–Wilk test (n < 50) and the Kolmogorov–Smirnov test. (n ≥ 50). All the analyses were performed with R Statistical Software version 3.5.1 for MAC.
Results
Both samples of infants and toddlers were distributed regarding age in months as following: infants and toddlers age 3–6 months 13.8%, 7–12 months 20.4%, 13–18 months 17.3%, 19–24 months 14.6%, and 25–36 months 33.9%. Further data on demographics are presented in Table 1.
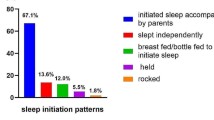
Table 2 compares sleep patterns and ecology before and during confinement. We found that during confinement, infants and toddlers went to sleep later than similar population under no confinement: median bedtime 21:30 (IQR 21–22) before confinement vs. 21:36 bedtime (IQR 21–22:30) during confinement (p = 0.004). This finding was also significant when considering the youngest infant group (3–6 months of age) with median bedtime 21:24 (IQR 20:48.8–22:18) before confinement vs. median bedtime 22:00 (IQR 21:30–23) during confinement (p = 0.017)) and the oldest toddler group (25–36 months of age) (median bedtime 21:36 (IQR 21:18–22:06) before confinement vs. median bedtime 22:00 (IQR 21:30–22:36) during confinement (p < 0.001) (see Supplementary tables: Table A. Bedtime). Regarding total sleep time in a 24-h period, we found a tendency for less total sleep time during confinement (12.0 h (IQR 11.0–13.0) before confinement vs. 12.0 h (IQR 11.0–12.7) during confinement) however non statistically significant (p = 0.078).
In Table 2, prevalence of infants and toddlers presenting with the criteria used in the original BISQ to define poor sleepers are presented [11] (total sleep time < 9 h, > 3 night awakenings, duration of awakenings > 1 h) as well as sleep onset latency longer than 30 min both before and during COVID-19 confinement. Results were adjusted for age distribution of our sample, sex, and parental level of education. We found more infants and toddlers presenting with a sleep latency longer than 30 min during confinement (p < 0.001). However, we found a decrease in infants and toddlers presenting with longer than 1 h nocturnal awakenings: 16.7% (IQR 14.8–18.8) before confinement vs. 9.8% (IQR 6.47–14.18) during confinement (p = 0.011).
Based on the mentioned BISQ criteria for classifying inadequate sleep patterns, we categorised both samples of infants and toddlers in three groups; (i) none, (ii) one of the poor sleeper BISQ criteria, and (iii) two or more poor sleeper BISQ criteria. We observed a statistically significant increase in infants and toddlers showing criteria for classifying poor sleepers during confinement (p < 0.001). Therefore, during COVID-19 home confinement, infants and toddlers showed longer sleep latency, later bedtime, and more criteria for classifying poor sleepers as defined in the original BISQ (more than three awakenings a night, nocturnal awakenings longer than 1 h and, a total sleep time of less than 9 h [11].
In Table 2, we also compare parental perception of the child’s sleep problem before confinement and during confinement. A trend of increasing parental perception of a child’s sleep as problematic was observed (39.4% of parents referring their child had a sleep problem before confinement vs. 44.1% of parents during confinement) however not statistically significant (adjusted p = 0.363).
In the supplementary tables, the main variables regarding sleep patterns (sleep time, bedtime, number and duration of nocturnal wakefulness, short sleep time, sleep latency, and parental perception) were presented adjusted for sex and age of child, level of education, age of the respondent, and parental perception of sleep difficulty.
Regarding sleep onset latency > 30 min, we found statistically significant differences in both samples globally (12.3% of infants and toddlers presenting a sleep onset latency > 30 min before confinement vs. 33.8% during confinement (p < 0.001). This difference was also found when comparing both sexes, all age groups and among parents with a university degree (10.6% before confinement vs. 38.7% during confinement (p < 0.001) (see supplementary tables: Table E: Sleep onset latency > 30 min).
We found no statistically significant differences in daytime napping (p-value = 0.090). In both samples before confinement and during confinement, daytime napping lasted a median of 2 h, the same first quartile (1 h 30 min) and just 15 min of difference in the third quartile (3 h before home confinement and 2 h 45 min during confinement).
Discussion
This comparative study on infant and toddler sleep patterns analyses two different but comparable samples recruited before and during the COVID-19 pandemic in Spain.
The relevance of studying sleep patterns in early childhood relies on the fact that adequate sleep patterns are linked to proper and long-term social-emotional development. A previous study found that later bedtimes and less total sleep across the 24-h period predicted higher internalizing problem scores (including indices of depression/withdrawal, general anxiety, separation distress, and inhibition) [15]. Regarding sleep patterns in paediatrics specifically during the COVID-19 pandemic, interestingly various and relevant literature has found that changes in sleep patterns are diverse and no unified change for the worse can actually be expected. Zreik [16] analyzed in Israel the possible negative implications for sleep during COVID-19 pandemic for both mothers and infants and toddlers 6–72 months of age, finding that about 30% of mothers reported a negative change in child's sleep quality and a decrease in sleep duration. However, there were also mothers who reported a positive change in sleep quality during COVID-19 pandemic [16]. In our study, we globally found a statistically significantly increase of infants and toddlers presenting inadequate sleep patterns as defined in the BISQ [11] during COVID confinement (37% of infants and toddlers vs. 25% before COVID-19 confinement) (p < 0.001).
Regarding adequacy of sleep duration in our sample, and based on the WHO guidelines for children younger than 5 years as reference [17] (infants younger than 1 year of age should sleep a minimum of 12 h of total sleep time and from 1 to 2 years of age a minimum of 11 h), remarkably, in our research, a quarter of them did not reach this total sleep time of 12 h (IQR 11–12.7). In a recent study analysing sleep patterns in Spanish children of relatively comparable age (0–2 years of age) during home confinement, total sleep time reported was mean of 10.98 h; (SD = 1.8) [18], Another research based in Spain on sleep patterns during COVID-19 pandemic analyzing 280 children from 0 to 4 years of age described a mean sleep time in infants younger than 1 year of 11.69 h (SD = 1.87) and among 1–2 years 11.35 h (SD = 1.74) [19]. Lecuelle [20] found in French preeschoolers that during home confinement, the length of nocturnal sleep increased from 10.3 to 10.9 h, however with no impact on the total duration of sleep over 24 h.
Difficulties initiating and maintaining sleep increased in our study, finding that infants and toddlers during confinement went to bed slightly later. This fact was especially substantial in both the youngest infants and the oldest toddlers. Although we do not have evidence for this finding, a possible explanation for these differences might be that younger and older infants are more aligned with their parents sleeping routines. For example, a study carried in the USA comparing the sleep of infants whose mothers were in home confinement to those whose mothers were working as usual throughout the COVID-19 pandemic found that those Infants with confined mothers had later sleep offset times and longer nighttime sleep durations, compared to infants of mothers who were working as usual [21].
We also found longer sleep onset latencies (> 30 min) during COVID-19 confinement, with infants and toddlers showing more difficulty to fall asleep. Interestingly, however, prolonged nocturnal awakening of more than 1 h decreased. We have analysed the possible impact of the passage to the daylight saving time (March 29, 2020 in Spain) in the sleep latency duration in our sample, not finding significant statistical differences among both samples (PR 0.99 (IC 95% 0.73–1.33, p-value = 0.932). Previous literature has already described similar findings regarding infants and toddlers with delayed bedtime being significantly associated with bedtime resistance even when adjusting for total sleep time [18, 22].
A study examining 3157 preschoolers in Chile found that during early stages of the pandemic, sleep duration increased, and sleep quality declined. Toddlers and preschoolers with space to play at home and living in rural areas experienced an attenuated impact of the pandemic restrictions on their physical activity levels, screen time, and sleep quality [23]. Therefore, home confinement might play a role in regulating sleep patterns intertwined with other variables previously described such as sleep light, activity level, social contact, and psychological well-being [6, 19, 24] as well as the potential influence of longer screen time exposure in explaining later bedtimes [8, 19, 24].
Previous literature has also pointed out that low optimism and parental stress correlates negatively with sleep duration and parental perception of sleep quality [25]. In our study, we found that 44% of parents indicated their child had a sleep problem during COVID-19 confinement, whereas 39% of parents stated sleep difficulties before COVID-19 confinement.
There were some limitations to the present study. Home confinement in Spain took place between March–May 2020; however, we recruited our sample from April to June 2020 after receiving approval from our Ethics Committee; therefore, a memory bias in this short time span might be taken into account. Both samples (before confinement and during confinement) showed slight differences in some characteristics such as a slightly uneven proportion of toddlers among 19–24 months of age in both samples (21% before confinement vs. 14% during confinement (p = 0.026)), a higher proportion of parents with a university degree (64% before confinement vs. 77% during confinement (p < 0.001)), and a higher percentage of parents younger than 25 years of age (1.5% before confinement vs. 10% during confinement (p < 0.001)). This might be probably due to the relatively smaller sample recruited during confinement. However, methodologically in both groups, we followed same procedural guidance.
Our sample may have a limited generalizability as participants were recruited by convenience sampling and were mostly living in the region of Catalonia in Spain. Regarding demographical characteristics, sample size limitations have to be noted. Despite this limitation, the results in this current research showed statistical significance. Our sample included an unbalanced proportion of families with higher education, as can be expected from a primarily internet-based study. Nevertheless, our findings were consistent with previous cross-cultural web-based studies [11, 26, 27], showing similar epidemiological characteristics so we believe we have obtained similar segments of the population within our country for purposes of cross-cultural comparison [11, 27]. For the present research, we based the definition of sleep difficulties solely on the criteria presented in the BISQ [11], thus not taking into account other aspects of this complex construct. We used a limited number of sleep variables to define sleep ecology without taking into account further variables that have shown to have a predictor value for sleep quality such as the use of routines, parental stress during COVID-19 pandemic, and sociodemographic relevant data such as size of living unit, income, housing location and space, and remote-working of one or both parents.
The reliance on parental reports in assessing infant sleep has inherent limitations; however, previous research [13, 28] has shown a high correlation between parent-reported sleep duration and actigraphy-recorded sleep duration in young healthy children. Further, parents with concern about their child’s sleep may have been more likely to participate, skewing this aspect of our results. Information bias may be an inherent limitation to web-based surveys. However, the fact that there was not an interviewer carrying out the questionnaire may have decreased an unacceptability bias (29).
Conclusions
These results suggest that confinement due to COVID-19 pandemic had a significant impact on infants’ and toddler’s sleep during the initial wave in Spain. In light of these findings, sleep habits need constant consideration along a child’s development as a changing environment and context such as the COVID-10 pandemic has shown to have a considerate impact among a short time span. Follow-up studies focusing on infant’s and toddler’s sleep patterns might help assess the potential long-term effects of the COVID-19 pandemic.
Availability of data and material
The database created for the study is available upon request.
Code availability
N/A.
Abbreviations
- BISQ:
-
Brief Infants Sleep Questionnaire
- COVID-19:
-
Coronavirus-SARS 2019 pandemic
- IQR:
-
Interquartile range
- WHO:
-
World Health Organisation
References
Camerota M, Propper C, Teti D (2019) Intrinsic and extrinsic factors predicting infant sleep: moving beyond main effects. Develop Rev 53
Sette S, Baumgartner E, Ferri R, Bruni O (2017) Predictors of sleep disturbances in the first year of life: a longitudinal study. Sleep Med 36:78–85
Brazendale K, Beets MW, Weaver RG et al (2017) Understanding differences between summer vs. school obesogenic behaviors of children: the structured days hypothesis. Int J Behav Nutr Phys Act 14:100
Cartanyà-Hueso À, Lidón-Moyano C, Cassanello P, Díez-Izquierdo A, Martín-Sánchez JC, Balaguer A, Martínez-Sánchez JM (2021) Smartphone and tablet usage during COVID-19 pandemic confinement in children under 48 months in Barcelona (Spain). Healthcare (Basel) 9(1):96
Panda PK, Gupta J, Chowdhury SR, Kumar R, Meena AK, Madaan P, Sharawat IK, Gulati S (2021) Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: a systematic review and meta-analysis. J Trop Pediatr 67(1):6
Markovic A, Mühlematter C, Beaugrand M, Camos V, Kurth S (2021) Severe effects of the COVID-19 confinement on young children's sleep: a longitudinal study identifying risk and protective factors. J Sleep Res 18
Liu Z, Tang H, Jin Q, Wang G, Yang Z, Chen H, Owens J (2020) Sleep of preschoolers during the coronavirus disease 2019 (COVID-19) outbreak. J Sleep Res e13142
Shinomiya Y, Yoshizaki A, Murata E, Fujisawa TX, Taniike M, Mohri I (2021) Sleep and the general behavior of infants and parents during the closure of schools as a result of the COVID-19 pandemic: comparison with 2019 data. Children 8:168
Cassanello P, Ruiz-Botia I, Díez-Izquierdo A et al (2020) How do infants and toddlers sleep in Spain? A cross-sectional study Eur J Pediatr 180(3):775–782
Sadeh A (2004) A brief screening questionnaire for infant sleep problems: validation and findings for an internet sample. Pediatrics 113
Cassanello P, Díez-Izquierdo A, Gorina N, Matilla-Santander N, Martínez-Sanchez JM, Balaguer A (2018) Adaptación y estudio de propiedades métricas de un cuestionario de valoración del sueño para lactantes y preescolares. An Pediatría 89(4):230–237
Lewandowski AS, Toliver-Sokol M (2011) Palermo TM (2011) Evidence-based review of subjective pediatric sleep measures. J Pediatr Psychol 36(7):780–793
Spruyt K, Gozal D (2021) Pediatric sleep questionnaires as diagnostic or epidemiological tools: a review of currently available instruments Sleep Med Rev 15:19–32
Mindell JA, Leichman ES, DuMond C, Sadeh A (2017) Sleep and social-emotional development in infants and toddlers. J Clin Child Adolesc Psychol 46(2):236–246
Zreik G, Asraf K, Haimov I, Tikotzky L (2021) Maternal perceptions of sleep problems among children and mothers during the coronavirus disease 2019 (COVID-19) pandemic in Israel. J Sleep Res 30(1):e13201
World Health Organization (2019) Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. World Health Organization. https://apps.who.int/iris/handle/10665/311664. Licencia: CC BY-NC-SA 3.0 IGO
Cachón-Zagalaz J, Zagalaz-Sánchez M, Arufe-Giráldez V, Sanmiguel-Rodríguez A, González-Valero G (2021) Physical activity and daily routine among children aged 0–2 during the COVID-19 pandemic in Spain. Int J Environ Res Public Health 18:703
Arufe-Giráldez V, Sanmiguel-Rodríguez A, Zagalaz-Sánchez ML, Cachón-Zagalaz J, Gonzalez-Valero G (2020) Sleep, physical activity and screens in 0–4 years Spanish children during the COVID-19 pandemic. Were the WHO recommendations met? J Hum Sport Exercise
Lecuelle F, Leslie W, Huguelet S, Franco P, Putois B (2020) Did the COVID-19 lockdown really have no impact on young children’s sleep? J Clin Sleep Med 16(12):2121
Kahn M, Barnett N, Glazer A, Gradisar M (2021) Infant sleep during COVID-19: Longitudinal analysis of infants of US mothers in home confinement versus working as usual. Sleep Health 7:19–23
Kitamura S, Enomoto M, Kamei Y et al (2015) Association between delayed bedtime and sleep-related problems among community-dwelling 2-year-old children in Japan. J Physiol Anthropol 34(1):12
Aguilar-Farias N, Toledo-Vargas M, Miranda-Marquez S, Cortinez-O’Ryan A, Cristi-Montero C, Rodriguez-Rodriguez F, Martino-Fuentealba P, Okely AD, Del Pozo CB (2020) Sociodemographic predictors of changes in physical activity, screen time, and sleep among toddlers and preschoolers in Chile during the COVID-19 pandemic. Int J Environ Res Public Health 18(1):176
Moore SA, Faulkner G, Rhodes RE, Brussoni M, Chulak-Bozzer T, Ferguson LJ, Mitra R, O’Reilly N, Spence JC, Vanderloo LM, Tremblay MS (2020) Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act 17(1):85
Miadich SA, Doane LD, Davis MC, Lemery-Chalfant K (2019) Early parental positive personality and stress: Longitudinal associations with children’s sleep. Br J Health Psychol 24(3):629–650
Sadeh A, Mindell JA, Luedke K, Wiegand B (2009) Sleep and sleep ecology in the first 3 years: a web-based study. J Sleep Res 18(1):60–73
Mindell JA, Sadeh A, Wiegand B, How TH, Goh DYT (2010) Cross-cultural differences in infant and toddler sleep. Sleep Med 11(3):274–280
Lomeli HA, Pérez-Olmos I, Talero-Gutiérrez C, Moreno CB, González-Reyes R, Palacios L, de la Peña F (2008) Muñoz-Delgado J (2008) Sleep evaluation scales and questionaries: a review. Actas Esp Psiquiatr 36(1):50–59
Díaz de Rada V (2018) Problemas de representatividad en las encuestas con muestreos probabilísticos. Pap Rev School 74:45
Author information
Authors and Affiliations
Contributions
Cassanello Pia and Balaguer Albert had primary responsibility for protocol development, sample enrolment, outcome assessment, preliminary data analysis, and writing the manuscript. Drs. Ruiz-Botia Irene and Sala-Castellvi Pere participated in the enrolment as well as analytical framework for the study and contributed to the writing of the manuscript. Martin Juan Carlos and Martínez-Sanchez Jose María supervised the design and execution of the study, performed the data analyses, and contributed to the writing of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The Institutional Ethics Review Board at Hospital Universitari General de Catalunya and Universitat Internacional de Catalunya, Barcelona, approved this study.
Consent to participate
All users provided consent to the inclusion of their data in the present research study and were able to decline participation at all times. The researchers provided users with contact information should they have any questions, concerns, or desire to withdraw consent.
Consent for publication
N/A.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cassanello, P., Ruiz-Botia, I., Sala-Castellvi, P. et al. Comparing infant and toddler sleep patterns prior to and during the first wave of home confinement due to COVID-19 in Spain. Eur J Pediatr 181, 1719–1725 (2022). https://doi.org/10.1007/s00431-022-04376-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04376-0