Abstract
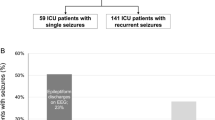
Neurological morbidity is a growing concern in children with severe bronchiolitis. The aim of the study was to evaluate the frequency of occurrence and the factors associated with seizures in very young infants < 3 months of age, admitted to a pediatric intensive care unit (PICU) for severe bronchiolitis. We performed a single center retrospective cohort study evaluating occurrence of seizures in infants admitted to the PICU between 2010 and 2018 for severe bronchiolitis. We described characteristics of the patients, laboratory test, brain imaging, and electroencephalogram results, as well as the treatment used. We conducted a multivariable logistic regression to identify factors associated with the occurrence of seizures. A p value < 0.05 was considered significant. A total of 805 patients were included in the study; 722 (89.6%) were mechanically ventilated. Twenty-six infants (3.2%, 95% confidence interval, 95% CI [2.1%; 4.7%]) had seizures shortly prior to admission or during PICU stay. In the multivariable analysis, hyponatremia (odds ratio, OR: 4.6, 95%CI [1.86; 11.43], p = 0.001) and invasive ventilation (OR: 2.6, 95% CI [1.14; 5.9], p < 0.001) were associated with an increased likelihood of seizures occurrence.
Conclusion: Seizures occur in at least 3% of very young infants with severe bronchiolitis, and the characteristics of these are different to those experienced by older infants, but they shared the same risk factors (hyponatremia and mechanical ventilation). This highlights the extrapulmonary morbidity associated with bronchiolitis in this population.
What is Known: • Bronchiolitis is the leading cause of pediatric intensive care admission and use of mechanical ventilation in infants. • Neurological morbidities have to be investigated in this population at risk of neurological complications. | |
What is New: • Seizure is a complication in at least 3% of very young infants with severe bronchiolitis. • Seizure characteristics are different, but the main risk factors are the same than in older infants (hyponatremia and mechanical ventilation). |

Similar content being viewed by others
Availability of data and material
Individual participant data will not be made available.
Code availability
Not applicable.
Abbreviations
- BIPAP:
-
Bilevel positive airway pressure
- CI:
-
Confidence interval
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomography
- EEG:
-
Electroencephalogram
- HFNC:
-
High flow nasal cannula
- IMV:
-
Invasive mechanical ventilation
- IQR:
-
Interquartile range
- MRI:
-
Magnetic resonance imaging
- nCPAP:
-
Nasal continuous positive airway pressure
- NIV:
-
Non-invasive ventilation
- OR:
-
Odds ratio
- PICU:
-
Pediatric intensive care unit
- RSV:
-
Respiratory syncytial virus
References
Meissner HC (2016) Viral bronchiolitis in children. New Engl J Med 374(62):72. https://doi.org/10.1056/nejmra1413456
Bohmwald K, Gálvez NMS, Ríos M, Kalergis AM (2018) Neurologic alterations due to respiratory virus infections. Front Cell Neurosci 12:386. https://doi.org/10.3389/fncel.2018.00386
Shein SL, Slain KN, Clayton JA, McKee B, Rotta AT, Wilson-Costello D (2017) Neurologic and functional morbidity in critically ill children with bronchiolitis*. Pediatr Crit Care Me 18:1106–1113. https://doi.org/10.1097/pcc.0000000000001337
Sweetman LL, Ng Y, Butler IJ, Bodensteiner JB (2005) Neurologic complications associated with respiratory syncytial virus. Pediatr Neurol 32:307–310. https://doi.org/10.1016/j.pediatrneurol.2005.01.010
Eisenhut M (2006) Extrapulmonary manifestations of severe respiratory syncytial virus infection – a systematic review. Crit Care 10:R107. https://doi.org/10.1186/cc4984
Ralston S, Hill V (2009) Incidence of apnea in infants hospitalized with respiratory syncytial virus bronchiolitis: a systematic review. J Pediatr 155:728–733. https://doi.org/10.1016/j.jpeds.2009.04.063
Ng Y, Cox C, Atkins J, Butler IJ (2001) Encephalopathy associated with respiratory syncytial virus bronchiolitis. J Child Neurol 16:105–108. https://doi.org/10.1177/088307380101600207
Cha T, Choi YJ, Oh J-W, Kim CR, Park DW, Seol IJ, Moon JH (2019) Respiratory syncytial virus-associated seizures in Korean children, 2011–2016. Korean J Pediatr 62:131–137. https://doi.org/10.3345/kjp.2018.07066
Uda K, Kitazawa K (2017) Febrile status epilepticus due to respiratory syncytial virus infection. Pediatr Int 59:878–884. https://doi.org/10.1111/ped.13300
Millichap JJ, Wainwright MS (2009) Neurological complications of respiratory syncytial virus infection: case series and review of literature. J Child Neurol 24:1499–1503. https://doi.org/10.1177/0883073808331362
Zlateva KT, Ranst MV (2004) Detection of subgroup B respiratory syncitial virus in the cerebrospinal fluid of a patient with respiratory syncitial virus pneumonia. Pediatr Infect Dis J 23:1065–1066. https://doi.org/10.1097/01.inf.0000143654.12493.c9
Kho N, Kerrigan JF, Tong T, Browne R, Knilans J (2004) Respiratory syncytial virus infection and neurologic abnormalities: retrospective cohort study. J Child Neurol 19:859–864. https://doi.org/10.1177/08830738040190110301
Lavagno C, Milani GP, Uestuener P, Simonetti GD, Casaulta C, Bianchetti MG, Fare PB, Lava SAG (2017) Hyponatremia in children with acute respiratory infections: a reappraisal. Pediatr Pulmonol 52:962–967. https://doi.org/10.1002/ppul.23671
Luu R, DeWitt PE, Reiter PD et al (2013) Hyponatremia in children with bronchiolitis admitted to the pediatric intensive care unit is associated with worse outcomes. J Pediatr 163:1652–1656.e1. https://doi.org/10.1016/j.jpeds.2013.06.041
Iwazu Y, Honma S, Fujisawa G, Uki K, Yanaka I, Sato Y, Murata M, Kusano E, Asano Y (2007) Hyponatremic seizure associated with acute respiratory infection. Clin Exp Nephrol 11:230–234. https://doi.org/10.1007/s10157-007-0476-5
Hanna S, Tibby S, Durward A, Murdoch I (2003) Incidence of hyponatraemia and hyponatraemic seizures in severe respiratory syncytial virus bronchiolitis. Acta Paediatr 92:430–434. https://doi.org/10.1111/j.1651-2227.2003.tb00573.x
Friedman JN, Rieder MJ, Walton JM (2014) Bronchiolitis: recommendations for diagnosis, monitoring and management of children one to 24 months of age. Paediatr Child Health 19:485–491. https://doi.org/10.1093/pch/19.9.485
Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, Johnson DW, Light MJ, Maraqa NF, Mendonca EA, Phelan KJ, Zorc JJ, Stanko-Lopp D, Brown MA, Nathanson I, Rosenblum E, Sayles S 3rd, Hernandez-Cancio S, American Academy of Pediatrics (2014) Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics 134:e1474–e1502. https://doi.org/10.1542/peds.2014-2742
Javouhey E, Barats A, Richard N, Stamm D, Floret D (2008) Non-invasive ventilation as primary ventilatory support for infants with severe bronchiolitis. Intensive Care Med 34(1608):1614. https://doi.org/10.1007/s00134-008-1150-4
Shein SL, Slain K, Schlurmann NM et al (2017) Hyponatremia and hypotonic intravenous fluids are associated with unfavorable outcomes of bronchiolitis admissions. Hosp Pediatr 7:263–270. https://doi.org/10.1542/hpeds.2016-0205
Valla FV, Baudin F, Demaret P, Rooze S, Moullet C, Cotting J, Ford-Chessel C, Pouyau R, Peretti N, Tume LN, Milesi C, le Roux BG (2019) Nutritional management of young infants presenting with acute bronchiolitis in Belgium, France and Switzerland: survey of current practices and documentary search of national guidelines worldwide. Eur J Pediatr 178:331–340. https://doi.org/10.1007/s00431-018-3300-1
Tume LN, Eveleens RD, Mayordomo-Colunga J et al (2020) Enteral feeding of children on noninvasive respiratory support: a four-center European study. Pediatr Crit Care Me Publish Ahead of Print. https://doi.org/10.1097/pcc.0000000000002602
Tume LN, Valla FV (2017) Enteral feeding in children on noninvasive ventilation is feasible, but clinicians remain fearful&ast. Pediatr Crit Care Me 18:1175–1176. https://doi.org/10.1097/pcc.0000000000001321
Watson RS, Asaro LA, Hertzog JH, Sorce LR, Kachmar AG, Dervan LA, Angus DC, Wypij D, Curley MAQ, RESTORE Study Investigators and the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network (2018) Long-term outcomes after protocolized sedation versus usual care in ventilated pediatric patients. Am J Resp Crit Care 197:1457–1467. https://doi.org/10.1164/rccm.201708-1768oc
Baudin F (2017) Viral bronchiolitis in PICUs: looking further than the acute phase! Pediatr Crit Care Me 18(1178):1179. https://doi.org/10.1097/pcc.0000000000001353
Essouri S, Baudin F, Chevret L et al (2017) Variability of care in infants with severe bronchiolitis: less-invasive respiratory management leads to similar outcomes. J Pediatr 188:156–162.e1. https://doi.org/10.1016/j.jpeds.2017.05.033
Essouri S, Laurent M, Chevret L, Durand P, Ecochard E, Gajdos V, Devictor D, Tissières P (2014) Improved clinical and economic outcomes in severe bronchiolitis with pre-emptive nCPAP ventilatory strategy. Intensive Care Med 40(84):91. https://doi.org/10.1007/s00134-013-3129-z
Libbey JE, Kirkman NJ, Smith MCP, Tanaka T, Wilcox KS, White HS, Fujinami RS (2008) Seizures following picornavirus infection. Epilepsia 49:1066–1074. https://doi.org/10.1111/j.1528-1167.2008.01535.x
Akturk H, Sık G, Salman N, Sutcu M, Tatli B, Akcay Ciblak M, Bulent Erol O, Hancerli Torun S, Citak A, Somer A (2015) Atypical presentation of human bocavirus: severe respiratory tract infection complicated with encephalopathy. J Med Virol 87:1831–1838. https://doi.org/10.1002/jmv.24263
Eisenhut M (2007) Cerebral involvement in respiratory syncytial virus disease. Brain and Development 29:454. https://doi.org/10.1016/j.braindev.2006.11.007
World Health Organization. Guidelines on neonatal seizures. (WHO, ed.) 2011. https://apps.who.int/iris/handle/10665/77756.
Singh A, Stredny CM, Loddenkemper T (2020) Pharmacotherapy for pediatric convulsive status epilepticus. Cns Drugs 34:47–63. https://doi.org/10.1007/s40263-019-00690-8
Milani GP, Rocchi A, Teatini T, Bianchetti MG, Amelio G, Mirra N, Grava A, Agostoni C, Fossali EF (2017) Hyponatremia in infants with new onset moderate-severe bronchiolitis: a cross-sectional study. Respir Med 133:48–50. https://doi.org/10.1016/j.rmed.2017.10.028
Acknowledgement
We thank Philip Robinson (DRCI, Hospices Civils de Lyon) for the help in the manuscript preparation.
Author information
Authors and Affiliations
Contributions
AH and FB conceptualized and designed the study, collected the data, drafted the initial manuscript, and reviewed and revised the manuscript. EJ and FV conceptualized the study, interpreted the data, and critically reviewed the manuscript for important intellectual content. JT interpreted the data and critically reviewed the manuscript for important intellectual content.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the ethics committee of the French intensive care society (CE SRLF 18-29).
Consent to participate
Retrospective study (non-opposition for data collection in the PICU was checked).
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Piet Leroy
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huguet, A., Valla, F., Toulouse, J. et al. Occurrence and risk factors associated with seizures in infants with severe bronchiolitis. Eur J Pediatr 180, 2959–2967 (2021). https://doi.org/10.1007/s00431-021-04070-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04070-7