Abstract
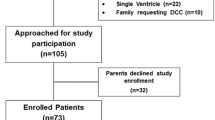
The time of cord clamping in intrauterine growth–restricted (IUGR) neonates remains an area of uncertainty. This assessor-blinded randomized controlled trial compared the effects of delayed cord clamping (DCC) with early cord clamping (ECC) on the systemic blood flow (SBF) and cerebral hemodynamics in IUGR neonates of gestational age ≥28 weeks, not requiring resuscitation. Eligible newborns were randomized to DCC (cord clamping after 60 s; n=55) or ECC (cord clamping within 30 s; n=55) group immediately after delivery. The primary outcome variable was superior vena cava (SVC) blood flow at 24±2 h. The secondary outcome variables were right ventricular output (RVO), anterior cerebral artery (ACA) blood flow velocity (BFV), superior mesenteric artery (SMA)-BFV and venous hematocrit at 24±2 h, peak total serum bilirubin (TSB), incidences of polycythemia, intraventricular hemorrhage, respiratory distress, feeding intolerance, and necrotizing enterocolitis, outcome, duration of hospital stay, screening audiometry, and serum ferritin levels at the postnatal age of 3 months. Compared to ECC, DCC was associated with significantly higher SVC flow (101.22±21.02 and 81.27±19.12 mL/kg/min, in DCC and ECC groups, respectively; p<0.0001), and significantly increased RVO, SMA-BFV, venous hematocrit, and serum ferritin levels. Though peak TSB was significantly higher with DCC, duration of phototherapy was comparable. ACA-BFV, incidence of polycythemia, and other outcomes were comparable between the groups.
Conclusions: DCC was a safe and beneficial intervention in IUGR infants with an improved SBF and SMA-BFV and an increased hematocrit and serum ferritin levels without higher incidences of polycythemia and requirement of phototherapy for significant hyperbilirubinemia.
Trial registration: Clinical Trials Registry of India (CTRI/2019/05/018904)
What is Known: • Delayed cord clamping (DCC) increases superior vena cava (SVC) blood flow in preterm neonates. • DCC increases hematocrit and serum ferritin in intrauterine growth–restricted (IUGR) neonates, but there may be an associated risk of polycythemia and neonatal hyperbilirubinemia. | |
What is New: • DCC increases SVC blood flow, right ventricular output, superior mesenteric artery blood flow velocity, venous hematocrit, and serum ferritin in IUGR neonates. • Incidences of polycythemia and duration of phototherapy for significant neonatal hyperbilirubinemia do not increase with DCC. |

Similar content being viewed by others
Data availability
Deidentified individual participant data (including data dictionaries) will be made available, in addition to study protocols, the statistical analysis plan, and the informed consent form. The data will be made available upon publication to researchers who provide a methodologically sound proposal for use in achieving the goals of the approved proposal. Proposals should be submitted to drkanhu.ped@gmail.com.
Abbreviations
- ACA:
-
Anterior cerebral artery
- ASSR:
-
Auditory Steady-State Response Audiometry
- ANOVA:
-
Analysis of variance
- BFV:
-
Blood flow velocity
- BW:
-
Birth weight
- BERA:
-
Brainstem-evoked response audiometry
- CC:
-
Cord clamping
- CI:
-
Confidence interval
- CPAP:
-
Continuous positive airway pressure
- CTRI:
-
Clinical Trial Registry of India
- EDV:
-
End-diastolic velocity
- GA:
-
Gestational age
- DCC:
-
Delayed cord clamping
- ECC:
-
Early cord clamping
- HHHFNC:
-
Heated humidified high flow nasal cannula
- IVH:
-
Intraventricular hemorrhage
- IUGR:
-
Intrauterine growth restriction
- IQR:
-
Interquartile range
- LED:
-
Light-emitting diode
- MD:
-
Mean difference
- n :
-
Number
- N :
-
Total number in that population
- NEC:
-
Necrotizing enterocolitis
- NNH:
-
Neonatal hyperbilirubinemia
- NNTB:
-
Number needed to treat for benefit
- NNTH:
-
Number needed to treat to harm
- NS:
-
Non-significant
- LAMA:
-
Left against medical advice
- PET:
-
Partial exchange transfusion
- PSV:
-
Peak-systolic velocity
- RCT:
-
Randomized controlled trial
- RI:
-
Resistive index
- RR:
-
Relative risk
- RVO:
-
Right ventricular output
- SD:
-
Standard deviation
- SMA:
-
Superior mesenteric artery
- SVC:
-
Superior vena cava
- TSB:
-
Total serum bilirubin
- TcB:
-
Transcutaneous bilirubinometer
- UA:
-
Umbilical artery
- VTI:
-
Velocity time integral
References
Balasubramanian H, Ananthan A, Jain V, Rao SC, Kabra N (2020) Umbilical cord milking in preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 105:572–580
Rabe H, Gyte GML, Díaz-Rossello JL, Duley L (2019) Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev 9:CD003248
Yao AC, Moinian M, Lind J (1969) Distribution of blood between infant and placenta after birth. Lancet 2:871–873
Smit M, Dawson JA, Ganzeboom A, Hooper SB, Van Roosmalen J, Te Pas AB (2014) Pulse oximetry in newborns with delayed cord clamping and immediate skin-to-skin contact. Arch Dis Child Fetal Neonatal Ed 99:F309–F314
Sommers R, Stonestreet BS, Oh W, Laptook A, Yanowitz TD, Raker C, Mercer J (2012) Hemodynamic effects of delayed cord clamping in premature infants. Pediatrics 129(3):e667–e672
Mercer JS, Vohr BR, McGrath MM, Padbury JF, Wallach M, Oh W (2006) Delayed cord clamping in very preterm infants reduces the incidence of intraventricular hemorrhage and late onset sepsis: a randomized, controlled trial. Pediatrics 117:1235–1242
Rabe H, Reynolds G, Diaz-Rossello J (2008) A systematic review and meta-analysis of a brief delay in clamping the umbilical cord of preterm infants. Neonatology 93:138–144
Fogarty M, Osborn DA, Askie L, Seidler AL, Hunter K, Lui K, Simes J, Tarnow-Mordi W (2018) Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. Am J Obstet Gynecol 218:1–18
Backes CH, Rivera BK, Haque U, Bridge JA, Smith CV, Hutchon DJ et al (2014) Placental transfusion strategies in very preterm neonates: a systematic review and meta-analysis. Obstet Gynecol 124:47–56
McDonald SJ, Middleton P, Dowswell T, Morris PS (2013) Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. Cochrane Database Syst Rev 7:CD004074
Andersson O, Lindquist B, Lindgren M, Stjernqvist K, Domellof M, Hellstrom-Westas L (2015) Effect of delayed cord clamping on neurodevelopment at 4 years of age: a randomized clinical trial. JAMA Pediatr 169:631–638
WHO (2014) Guideline: delayed umbilical cord clamping for improved maternal and infant health and nutrition outcomes. World Health Organization, Geneva www.who.int/elena/titles/cord_clamping/en/
Aziz K, Lee HC, Escobedo MB, Hoover AV, Kamath-Rayne BD, Kapadia VS, Magid DJ, Niermeyer S, Schmölzer GM, Szyld E, Weiner GM, Wyckoff MH, Yamada NK, Zaichkin J (2020) Part 5: Neonatal Resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 142:S524–S550
de Onis M, Blossner M, Villar J (1998) Levels and patterns of intrauterine growth retardation in developing countries. Eur J Clin Nutr 52:S83–S93
Saleem T, Sajjad N, Fatima S, Habib N, Ali SR, Qadir M (2011) Intrauterine growth retardation--small events, big consequences. Ital J Pediatr 37:41
Olsen RN, Shepherd J, Katheria A (2014) Postnatal systemic blood flow in neonates with abnormal fetal umbilical artery Doppler. ISRN Obstet Gynecol 2014:957180
Kluckow M, Evans N (2000) Superior vena cava flow in newborn infants: a novel marker of systemic blood flow. Arch Dis Child Fetal Neonatal Ed 82:F182–F187
Fenton C, McNinch NL, Bieda A, Dowling D, Damato E (2018) Clinical outcomes in preterm infants following institution of a delayed umbilical cord clamping practice change. Adv Neonatal Care 18:223–231
Wirth FH, Goldberg KE, Lubchenco LO (1979) Neonatal hyperviscosity: I. Incidence. Pediatrics 63:833–836
Papageorghiou AT, Ohuma EO, Altman DG, Todros T, Cheikh Ismail L, Lambert A, International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st) et al (2014) International standards for fetal growth based on serial ultrasound measurements: the Fetal Growth Longitudinal Study of the INTERGROWTH-21st Project. Lancet 384:869–879 Erratum in: Lancet 384:1264
Papile LA, Burstein J, Burstein R, Koffler H (1978) Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birthweights less than 1500 g. J Pediatr 92:529–534
Fanaro S (2013) Feeding intolerance in the preterm infant. Early Hum Dev 89:13–20
Kliegman RM, Walsh MC (1987) Neonatal necrotizing enterocolitis: pathogenesis, classification, and spectrum of illness. Curr Probl Pediatr 17:213–288
Yanowitz TD, Yao AC, Pettigrew KD, Werner JC, Oh W, Stonestreet BS (1999) Postnatal hemodynamic changes in very-low-birthweight infants. J Appl Physiol 87:370–380
Evans N, Kluckow M, Simmons M, Osborn D (2002) Which to measure, systemic or organ blood flow? Middle cerebral artery and superior vena cava flow in very preterm infants. Arch Dis Child Fetal Neonatal Ed 87:F181–F184
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia (2004) Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 114:297–316 Erratum in: Pediatrics114:1138
National Collaborating Centre for Women’s and Children’s Health. Neonatal jaundice: Clinical guideline. 2010. https://www.nice.org.uk/guidance/cg98/evidence/full-guideline-245411821 [Last accessed on 6 November, 2020]
Groves AM, Kuschel CA, Knight DB, Skinner JR (2008) Echocardiographic assessment of blood flow volume in the superior vena cava and descending aorta in the newborn infant. Arch Dis Child Fetal Neonatal Ed 93:F24–F28
Lee A, Liestol K, Nestaas E, Brunvand L, Lindemann R, Fugelseth D (2010) Superior vena cava flow: feasibility and reliability of the off-line analyses. Arch Dis Child Fetal Neonatal Ed 95:F121–F125
Ha KS, Choi BM, Lee EH, Shin J, Cho HJ, Jang GY, Son CS (2018) Chronological echocardiographic changes in healthy term neonates within postnatal 72 hours using Doppler studies. J Kor Med Sci 33:e155
Sloot SC, de Waal KA, van der Lee JH, van Kaam AH (2010) Central blood flow measurements in stable preterm infants after the transitional period. Arch Dis Child Fetal Neonatal Ed 95:F369–F372
Groves AM, Kuschel CA, Knight DB, Skinner JR (2008) Relationship between blood pressure and blood flow in newborn preterm infants. Arch Dis Child Fetal Neonatal Ed 93:F29–F32
Meyer MP, Mildenhall L (2012) Delayed cord clamping and blood flow in the superior vena cava in preterm infants: an observational study. Arch Dis Child Fetal Neonatal Ed 97:F484–F486
Popat H, Robledo KP, Sebastian L, Evans N, Gill A, Kluckow M et al (2016) Effect of delayed cord clamping on systemic blood flow: a randomized controlled trial. J Pediatr 78:81–86.e2
Sahoo T, Thukral A, Sankar MJ, Gupta SK, Agarwal R, Deorari AK, Paul VK (2020) Delayed cord clamping in Rh-alloimmunised infants: a randomised controlled trial. Eur J Pediatr 179:881–889
Chopra A, Thakur A, Garg P, Kler N, Gujral K (2018) Early versus delayed cord clamping in small for gestational age infants and iron stores at 3 months of age - a randomized controlled trial. BMC Pediatrics 18:234
Wang M, Mercer JS, Padbury JF (2018) Delayed cord clamping in infants with suspected intrauterine growth restriction. J Pediatr 201:264–268
Tarnow-Mordi W, Morris J, Kirby A, Robledo K, Askie L, Brown R, Australian Placental Transfusion Study Collaborative Group et al (2017) Delayed versus immediate cord clamping in preterm infants. N Engl J Med 377:2445–2455
Fu X, Dang D, Li S, Xu Z, Wu H (2020) Effect of delayed versus early cord clamping on improving anemia in term infants aged two months or older - a meta-analysis. Indian Pediatr 57:815–819
Singh Y, Tissot C, Fraga MV, Yousef N, Cortes RG, Lopez J, Sanchez-de-Toledo J, Brierley J, Colunga JM, Raffaj D, da Cruz E, Durand P, Kenderessy P, Lang HJ, Nishisaki A, Kneyber MC, Tissieres P, Conlon TW, de Luca D (2020) International evidence-based guidelines on Point of Care Ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care 24:65
Acknowledgments
We would like to thank all the study infants and their families who accepted joining this study.
Author information
Authors and Affiliations
Contributions
Prof Sriparna Basu, Dr. Kanhu Charan Digal, Dr. Poonam Singh, and Dr. Yash Srivastava conceptualized and designed the study, coordinated and supervised data collection, drafted the initial manuscript, and reviewed and revised the manuscript. Dr. Yash Srivastava performed the echocardiography and color Doppler procedures. Prof Jaya Charurvedi helped in data collection and reviewed the manuscript. Dr. Amit Kumar Tyagi performed the hearing assessment and reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The trial was ethically approved by the institute ethics committee of All India Institute of Medical Sciences, Rishikesh, India. Written informed consent was obtained from all the parents of the study participants.
Consent for publication
Written informed consent was obtained from all the parents of the study participants for publication of their data.
Competing interests
The authors declare no competing interests.
Code availability
N/A.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Digal, K.C., Singh, P., Srivastava, Y. et al. Effects of delayed cord clamping in intrauterine growth–restricted neonates: a randomized controlled trial. Eur J Pediatr 180, 1701–1710 (2021). https://doi.org/10.1007/s00431-021-03959-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-03959-7