Abstract
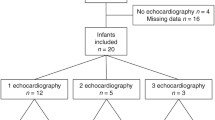
The impact of patent ductus arteriosus (PDA) on vital sign trends represented as histograms, and perfusion index in particular, is unknown. This study aimed to split continuously obtained PI and other vital signs before, during, and after medical treatment of PDA, into histogram bins, and determine the utility of PI and other vital sign histograms in the early prediction of hemodynamically significant PDA (hsPDA). In 34 infants at a mean gestational age of 26 ± 2.1 weeks, we prospectively collected vital signs for three different periods, 24 h before starting treatment of PDA, during PDA treatment, and 24 h after completion of the course of treatment, and confirmed PDA closure by echo. Histograms with three comparable periods were obtained from preterm infants who did not require treatment for PDA and analyzed for comparison. The duration of time spent in each histogram bin was determined for each time epoch. Episodes of low PI < 0.4 and high PI > 2 were significantly longer in duration in infants with PDA before treatment compared to those in infants with PDA during and after treatment. The arterial oxygen saturation (SpO2) < 80% was also longer in duration in infants with PDA before compared to that in infants with PDA during and after treatment. Low PI < 0.4 correlated with most echocardiography indices of hsPDA.
Conclusion: We conclude that a patent ductus arteriosus requiring treatment in preterm infants ≤ 29 weeks GA was associated with significant fluctuations between a low PI < 0.4 alternating with a high PI > 2, reflecting the dynamic nature of hsPDA shunt volume. PI variability may be an early marker of hsPDA.
What is Known: • The perfusion index is a continuous underutilized parameter provided by pulse oximetry to assess the peripheral perfusion. • The perfusion index helps predict conditions with hemodynamic instability. | |
What is New: • The perfusion index assessed as daily histogram trends can predict patent ductus arteriosus requiring treatment. |



Similar content being viewed by others
Data availability
All data and original material are available for transparency.
Abbreviations
- ABP:
-
Arterial blood pressure
- DBP:
-
Diastolic blood pressure
- hsPDA:
-
Hemodynamically significant patent ductus arteriosus
- HR:
-
Heart rate
- MBP:
-
Mean blood pressure
- PDA:
-
Patent ductus arteriosus
- PI:
-
Perfusion index
- SpO2 :
-
Oxygen saturation measured by pulse oximetry
- SBP:
-
Systolic blood pressure
- Echo:
-
Neonatal echocardiography performed by a pediatric cardiologist
References
Noori S, McCoy M, Anderson MP, Ramji F, Seri I (2014) Changes in cardiac function and cerebral blood flow in relation to peri/intraventricular hemorrhage in extremely preterm infants. J Pediatr 164(2):264–70.e1-3 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24183212
Noori S, Wlodaver A, Gottipati V, McCoy M, Schultz D, Escobedo M (2012) Transitional changes in cardiac and cerebral hemodynamics in term neonates at birth. J Pediatr. [cited 2012 Jul 3];160(6):943–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22244465
Noori S, Stavroudis TA, Seri I (2009) Systemic and cerebral hemodynamics during the transitional period after premature birth. Clin Perinatol. [cited 2012 may 14];36(4):723–36, v. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19944832
Rakza T, Magnenant E, Klosowski S, Tourneux P, Bachiri A, Storme L (2007) Early hemodynamic consequences of patent ductus arteriosus in preterm infants with intrauterine growth restriction. J Pediatr. Dec;151(6):624–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18035142
Teixeira LS, Shivananda SP, Stephens D, Arsdell G Van, Mcnamara PJ (2008) Postoperative cardiorespiratory instability following ligation of the preterm ductus arteriosus is related to early need for intervention. 803–10
Fraser D (2017) Patent ductus arteriosus in preterm infants , part 1 : understanding the pathophysiologic link between the patent ductus arteriosus and clinical complications. 36(5):265–72
Giliberti P, De Leonibus C, Giordano L, et al (2016) The physiopathology of the patent ductus arteriosus. 7058(July)
Louis D, Elsayed YN, Ojah C, Alvaro R, Shah PS, Dunn M (2017) Predictors of PDA treatment in preterm neonates who had received prophylactic indomethacin. Am J Perinatol
Skinner JR, Hunter S, Poets CF, Milligan DWA, Southall D, Hey EN (1999) Haemodynamic effects of altering arterial oxygen saturation in preterm infants with respiratory failure. Arch Dis Child 80(2):F81–F87
Bonestroo HJC, Lemmers PMA, Baerts W, van Bel F (2011) Effect of antihypotensive treatment on cerebral oxygenation of preterm infants without PDA. Pediatrics. 128(6):e1502–e1510
El-Khuffash A, James AT, Corcoran JD, Dicker P, Franklin O, Elsayed YN et al (2015) A patent ductus arteriosus severity score predicts chronic lung disease or death before discharge. J Pediatr 167(6)
Schena F, Francescato G, Cappelleri A, Picciolli I, Mayer A, Mosca F et al (2015) Association between hemodynamically significant patent ductus arteriosus and bronchopulmonary dysplasia. J Pediatr 166(6)
Singh Y, Tissot C (2018) Echocardiographic evaluation of transitional circulation for the neonatologists. Front Pediatr 6(May):140 Available from: http://journal.frontiersin.org/article/10.3389/fped.2018.00140/full
Singh Y, Tissot C, Fraga MV, Yousef N, Cortes RG, Lopez J et al (2020) International evidence-based guidelines on Point of Care Ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care 24(1):1–16
Bizzarro M, Li F, Katz K, Shabanova V, Ehrenkranz R, Bhandari V (2013) Temporal quantification of oxygen saturation ranges: an effort to reduce hyperoxia in the neonatal intensive care unit. J Perinatol 34(10):33–38
Elsayed YN, Fraser D (2016) Integrated evaluation of neonatal hemodynamics program optimizing organ perfusion and performance in critically ill neonates, part 1: understanding physiology of neonatal hemodynamics. Neonatal Netw 35(3)
Elsayed YFD (2016) Integrated evaluation of neonatal hemodynamics, part 2: systematic bedside assessment. 192–203
Elsayed YN, Louis D, Ali YH, Amer R, Seshia MM et al (2018) Integrated evaluation of hemodynamics: a novel approach for the assessment and management of preterm infants with compromised systemic circulation. J Perinatol 38(10):1337–1343
Hintz SR, Barnes PD, Bulas D, Slovis TL, Finer NN, Wrage LA et al (2015) Neuroimaging and neurodevelopmental outcome in extremely preterm infants. Pediatrics 135(1):e32–e42 Available from: http://www.ncbi.nlm.nih.gov/pubmed/25554820
Takami T, Sunohara D, Kondo A, Mizukaki N, Suganami Y, Takei Y, Miyajima T, Hoshika A (2010) Changes in cerebral perfusion in extremely LBW infants during the first 72 h after birth. Pediatr Res 68(5):435–439
Vidal M, Ferragu F, Durand S, Baleine J, Batista-Novais AR, Cambonie G (2012) Perfusion index and its dynamic changes in preterm neonates with patent ductus arteriosus. Acta Paediatr. [cited 2013 mar 23];373–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23330870
Nitzan I, Hammerman C, Fink D, Nitzan M, Koppel R, Bromiker R (2018) The effect of patent ductus arteriosus on pre-ductal and post-ductal perfusion index in preterm neonates. Physiol Meas 39(7)
Corsini I, Cecchi A, Coviello C, Dani C (2017) Perfusion index and left ventricular output correlation in healthy term infants. Eur J Pediatr 176(8):1013–1018
Granelli ADW, Östman-Smith I (2007) Noninvasive peripheral perfusion index as a possible tool for screening for critical left heart obstruction. Acta Paediatr Int J Paediatr 96(10):1455–1459
Gomez-Pomar E, Makhoul M, Westgate PM, Ibonia KT, Patwardhan A, Giannone PJ, Bada HS, Abu Jawdeh EG (2017) Relationship between perfusion index and patent ductus arteriosus in preterm infants. Pediatr Res 81(5):775–779
Sur A (2020) Histogram analysis for bedside respiratory monitoring in not critically ill preterm neonates: a proposal for a new way to look at the monitoring data
Evans N, Iyer P (1993) Change in blood pressure after treatment of patent ductus arteriosus with indomethacin. Arch Dis Child 68(5 Spec No):584–7. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1029308&tool=pmcentrez&rendertype=abstract
Clyman RI, Couto J, Murphy GM (2012) Patent ductus arteriosus: are current neonatal treatment options better or worse than no treatment at all? Semin Perinatol. [cited 2014 Jan 30];36(2):123–9. Available from: https://doi.org/10.1053/j.semperi.2011.09.022
Elsayed YN, Amer R, Seshia MM (2017) The impact of integrated evaluation of hemodynamics using targeted neonatal echocardiography with indices of tissue oxygenation: a new approach. J Perinatol 37:527–535
El-Khuffash A, Herbozo C, Jain A, Lapointe A, McNamara PJ (2013) Targeted neonatal echocardiography (TnECHO) service in a Canadian neonatal intensive care unit: a 4-year experience. J Perinatol 33(February):1–4 Available from: http://www.ncbi.nlm.nih.gov/pubmed/23619373
Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P, et al (2011) Targeted neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for training. Eur J Echocardiogr. [cited 2012 Jun 25];12(10):715–36. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21998460
Bendapudi P, Barr S (2014) Diagnosis and management of pulmonary hypertension of the newborn. Paediatr child heal (United Kingdom) 24(1):12–16. Available from. https://doi.org/10.1016/j.paed.2013.05.021
Hakan N, Dilli D, Zenciroglu A, Aydin M, Okumus N (2014) Reference values of perfusion indices in hemodynamically stable newborns during the early neonatal period. Eur J Pediatr 173(5):597–602
Afshar N, Baier RJ, Tagin M, Minski J, Elsayed RRTYN, De Cabo C (2018) The impact of hypoxemia on the development of retinopathy of prematurity in infants less than 29 weeks of gestation. 1(212)
Goff DA, Buckley EM, Durduran T, Wang J, Licht DJ (2010) Noninvasive cerebral perfusion imaging in high-risk neonates. Semin Perinatol 34(1):46–56. Available from. https://doi.org/10.1053/j.semperi.2009.10.005
Groves AM, Kuschel CA, Knight DB, Skinner JR (2008) Does retrograde diastolic flow in the descending aorta signify impaired systemic perfusion in preterm infants? Pediatr Res 63(1):89–94 Available from: http://www.ncbi.nlm.nih.gov/pubmed/18043512
Navarro-Guzman EA, Ledezma-Bautista I, Rubio-Hernandez ME, Escalante-Padron FJ, Lima-Roguel V, Pierdant-Perez M (2019) Correlation of perfusion index with patent ductus arteriosus repercussion in premature newborns. Arch Cardiol Mex 89(2):111–117
Cresi F, Pelle E, Calabrese R, Costa L, Farinasso D, Silvestro L (2010) Perfusion index variations in clinically and hemodynamically stable preterm newborns in the first week of life. Ital J Pediatr 36(6):1–5
Author information
Authors and Affiliations
Contributions
All authors made a substantial contribution to the manuscript and the design of the work: Asmaa Osman was the principal investigator and collected the data, Fatema Elhawary helped in data analysis, Muflih Albalawi performed the required echocardiography studies, and Shyamala Dakshinamurti and Martha Hinton performed the revised statistical analysis and the language. Yasser Elsayed was the principal supervisor, Asmaa Osman and Wegdan Mawlana helped in writing the manuscript, and Yasser Elsayed is the external expert in hemodynamics who designed the protocol included in the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the ethical committee of King Salman Armed Forces Hospital for data collection and publication.
Statement of informed consent
The consent was obtained from parents of all recruited infants for data collection and publication.
Additional information
Communicated by Daniele De Luca
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Communicated by Daniele De Luca
Rights and permissions
About this article
Cite this article
Osman, A.A., Albalawi, M., Dakshinamurti, S. et al. The perfusion index histograms predict patent ductus arteriosus requiring treatment in preterm infants. Eur J Pediatr 180, 1747–1754 (2021). https://doi.org/10.1007/s00431-021-03937-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-03937-z