Abstract
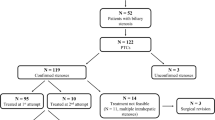
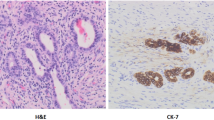
We studied the etiological spectrum, clinicolaboratory and histological profile, and outcome of infants and children under 18 years of age presenting between December 2010 and May 2016 with histological evidence of paucity of intralobular bile ducts (PILBD, bile ducts to portal tract ratio < 0.6) Post-transplant PILBD was excluded. Of 632 pediatric liver biopsies screened, 70 had PILBD—44 were infants. PILBD was classified histologically into destructive (n = 50) and non-destructive PILBD (n = 20). Presentations were jaundice (98%), organomegaly (94%), pale stools (50%), and pruritus (43%). Infants had more cholestasis but less fibrosis on histology. Overall, 29 required liver transplantation (LT) for portal hypertension (n = 26), decompensation (n = 25), growth failure (n = 20), intractable pruritus (n = 5), and recurrent cholangitis (n = 2). Destructive PILBD has an odds for poor outcome (decompensation or need for LT within 1 year) of 1.53 (95% CI = 1.15–2.04). On binary logistic regression analysis, poor outcome was related to advanced fibrosis on liver biopsy [Exp (B) = 5.46, 95% CI = 1.56–19.04].
Conclusion: PILBD was present in 11% of pediatric liver biopsies and has a varied etiological spectrum. Destructive PILBD has poor outcome. Need for LT is guided by the presence of advanced fibrosis.
What is Known: • Natural history of syndromic ductal paucity (Alagille syndrome) is complex. • Duct loss is commonly seen with late presentation of biliary atresia. | |
What is New: • The study classifies the etiological spectrum of ductal paucity histologically into destructive and non-destructive. • Destructive duct loss carries poor prognosis regardless of the etiology of liver disease with subsequent need for liver transplantation. |



Similar content being viewed by others
Abbreviations
- ARC syndrome:
-
Arthrogryposis renal dysfunction cholestasis syndrome
- AST:
-
Aspartate transaminase
- CI:
-
Confidence interval
- CPSS:
-
Congenital portosystemic shunt
- GGT:
-
Gamma-glutamyl transpeptidase
- INR:
-
International normalized ratio
- IQR:
-
Interquartile range
- PFIC:
-
Progressive familial intrahepatic cholestasis
- PILBD:
-
Paucity of intralobular bile ducts
- LB:
-
Liver biopsy
- LT:
-
Liver transplantation
References
Alonso EM, Snover DC, Montag A, Freese DK, Whitington PF (1994) Histologic pathology of the liver in progressive familial intrahepatic cholestasis. J Paediatric Gastroenterol Nutr 18(2):128–133
Bruguera M, Llach J, Rodes J (1992) Nonsyndromic paucity of intrahepatic bile ducts in infancy and idiopathic ductopenia in adulthood: the same syndrome? Hepatology 15(5):830–834
Davit-Spraul A, Fabre M, Branchereau S, Baussan C, Gonzales E, Stieger B, Bernard O, Jacquemin E (2010) ATP8B1 and ABCB11 analysis in 62 children with normal gamma-glutamyl transferase progressive familial intrahepatic cholestasis (PFIC): phenotypic differences between PFIC1 and PFIC2 and natural history. Hepatology 51(5):1645–1655
Deprettere A, Portmann B, Mowat AP (1987) Syndromic paucity of the intrahepatic bile ducts: diagnostic difficulty; severe morbidity throughout early childhood. J Paediatric Gastroenterol Nutr 6(6):865–871
Emerick KM, Rand EB, Goldmuntz E, Krantz ID, Spinner NB, Piccoli DA (1999) Features of Alagille syndrome in 92 patients: frequency and relation to prognosis. Hepatology 29(3):822–829
Fawaz R, Baumann U, Ekong U, Fischler B, Hadzic N, Mack CL, McLin V, Molleston JP, Neimark E, Ng VL, Karpen SJ (2017) Guideline for the evaluation of cholestatic jaundice in infants: Joint Recommendations of the North American Society for Paediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr 64(1):154–168
Hoffenberg EJ, Narkewicz MR, Sondheimer JM, Smith DJ, Silverman A, Sokol RJ (1995) Outcome of syndromic paucity of interlobular bile ducts (Alagille syndrome) with onset of cholestasis in infancy. J Pediatr 127(2):220–224
Kahn E, Daum F, Markowitz J, Teichberg S, Duffy L, Harper R, Aiges H (1986) Nonsyndromatic paucity of interlobular bile ducts: light and electron microscopic evaluation of sequential liver biopsies in early childhood. Hepatology 6(5):890–901
Koçak N, Gürakan F, Yüce A, Çağlar M, Kale G, Göğüş S (1997) Nonsyndromic paucity of interlobular bile ducts: clinical and laboratory findings of 10 cases. J Pediatr Gastroenterol Nutr 24(1):44–48
Nakanuma Y, Sasaki M, Harada K (2015) Autophagy and senescence in fibrosing cholangiopathies. J Hepatol 62(4):934–945
Naveh Y, Bassan L, Rosenthal E, Berkowitz D, Jaffe M, Mandel H, Berant M (1997) Progressive familial intrahepatic cholestasis among the Arab population in Israel. J Pediatr Gastroenterol Nutr 24(5):548–554
Nietgen GW, Vacanti JP, Perez-Atayde AR (1992) Intrahepatic bile duct loss in biliary atresia despite portoenterostomy: a consequence of ongoing obstruction? Gastroenterology 102(6):2126–2133
Pawlikowska L, Strautnieks S, Jankowska I, Czubkowski P, Emerick K, Antoniou A, Wanty C, Fischler B, Jacquemin E, Wali S, Blanchard S, Nielsen IM, Bourke B, McQuaid S, Lacaille F, Byrne JA, van Eerde AM, Kolho KL, Klomp L, Houwen R, Bacchetti P, Lobritto S, Hupertz V, McClean P, Mieli-Vergani G, Shneider B, Nemeth A, Sokal E, Freimer NB, Knisely AS, Rosenthal P, Whitington PF, Pawlowska J, Thompson RJ, Bull LN (2010) Differences in presentation and progression between severe FIC1 and BSEP deficiencies. J Hepatol 53(1):170–178
Raweily EA, Gibson AA, Burt AD (1990) Abnormalities of intrahepatic bile ducts in extrahepatic biliary atresia. Histopathology 17(6):521–527
Reau NS, Jensen DM (2008) Vanishing bile duct syndrome. Clin Liver Dis 12(1):203–217 x
Sibal A, Mishra U (2001) Bile duct paucity—making a case for liver biopsy in the investigation of neonatal cholestasis. Indian Pediatr 38(12):1430–1431
Srivastava A, Goel D, Bolia R, Poddar U, Yachha SK (2014) Alagille syndrome: experience of a tertiary care center in North India. Indian J Gastroenterol 33(1):59–62
Yamaguti DC, Patricio FR (2011) Morphometrical and immunohistochemical study of intrahepatic bile ducts in biliary atresia. Eur J Gastroenterol Hepatol 23(9):759–765
Yehezkely-Schildkraut V, Munichor M, Mandel H, Berkowitz D, Hartman C, Eshach-Adiv O, Shamir R (2003) Nonsyndromic paucity of interlobular bile ducts: report of 10 patients. J Pediatr Gastroenterol Nutr 37(5):546–549
Author information
Authors and Affiliations
Contributions
BLM collected data, BLM and RK analyzed data, CB and AR provided histopathological details, and BLM and RK prepared the first draft which was edited by RK and approved by all other authors. RK will be the guarantor of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical adherence
Maintained.
Additional information
Communicated by Peter de Winter
Rights and permissions
About this article
Cite this article
Meena, B.L., Khanna, R., Bihari, C. et al. Bile duct paucity in childhood—spectrum, profile, and outcome. Eur J Pediatr 177, 1261–1269 (2018). https://doi.org/10.1007/s00431-018-3181-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3181-3