Abstract
The objective of the study was to report our institutional experience in the management of children and newborns with refractory septic shock who required venoarterial extracorporeal membrane oxygenation (VA ECMO) treatment, and to identify patient-and infection-related factors associated with mortality. This is a retrospective case series in an intensive care unit of a tertiary pediatric center. Inclusion criteria were patients ≤ 18 years old who underwent a VA ECMO due to a refractory septic shock due to circulatory collapse. Patient conditions and support immediately before ECMO, analytical and hemodynamic parameter evolution during ECMO, and post-canulation outcome data were collected. Twenty-one patients were included, 13 of them (65%) male. Nine were pediatric and 12 were newborns. Median septic shock duration prior to ECMO was 29.5 h (IQR, 20–46). Eleven patients (52.4%) suffered cardiac arrest (CA). Neonatal patients had worse Sepsis Organ Failure Assessment (SOFA) score, Oxygenation Index and PaO2/FiO2 ratio, blood gas analysis, lactate levels, and left ventricular ejection fraction compared to pediatric patients. Survival was 33.3% among pediatric patients (60% if we exclude pneumococcal cases) and 50% among newborns. Hours of sepsis evolution and mean airway pressure (MAP) prior to ECMO were significantly higher in the non-survivor group. CA was not a predictor of mortality. Streptococcus pneumoniae infection was a mortality risk factor. There was an improvement in survival during the second period, from 14.3 to 57.2%, related to shorter sepsis evolution before ECMO placement, better candidate selection, and greater ECMO support once the patient was placed.
Conclusion: Patients with refractory septic shock should be transferred precociously to a referral ECMO center. However, therapy should be used with caution in patients with vasoplegic pattern shock or S. pneumoniae sepsis.
What is Known: • Children with refractory septic shock have significant mortality rates, and although ECMO is recommended, overall survival is low. • There are no studies regarding characteristics of infections as predictors of pediatric survival in ECMO. | |
What is New: • Septic children should be transferred precociously to referral ECMO centers during the first hours if patients do not respond to conventional therapy. • Treatment should be used with caution in patients with vasoplegic pattern shock or S. pneumoniae sepsis. |
Similar content being viewed by others
Introduction
Despite treatment advances in critical patient management, septic shock is one of the leading causes of death among children worldwide. In developed countries, mortality in septic children ranges from 2 to 13%, and it is higher among those with underlying diseases [17]. Shock development and multiorgan dysfunction syndrome are the most determinant factors of mortality [13, 21]. The American College of Critical Care Medicine published guidelines in which veno-arterial extracorporeal membrane oxygenation (VA ECMO) is suggested in pediatric and newborn patients with unresponsive refractory septic shock to fluids and inotropic support [5, 6, 15]. In addition, a recent (2017) review by Extracoporeal Life Support Organization (ELSO) pointed out that survival of pediatric refractory septic shock in ECMO has improved [7], although it still has a wide range (between 27 and 70% depending on the series) [2, 10,12,12, 19], perhaps due to different ECMO strategies and causative microorganisms.
The aims of the present study were to describe our VA ECMO experience in the management of refractory septic shock in our pediatric and neonatal intensive care units, to compare newborns and pediatric patients, and to identify patient- and infection-related factors associated with mortality.
Patients and methods
This is a single-center retrospective observational study carried out at Hospital Sant Joan de Déu, Barcelona (Spain), a tertiary referral pediatric hospital. We reviewed our ECMO database to identify those newborns and children who received VA ECMO from January 1, 2001, to January 31, 2017.
Patients were included in the study if they met the following criteria:
-
Refractory septic shock according to the 2005 Pediatric Sepsis Consensus Conference criteria [8] requiring VA ECMO for circulatory collapse despite mechanical ventilation (MV), fluid resuscitation, and inotrope therapy.
-
Positive bacterial culture or real-time polymerase chain reaction (PCR), before ECMO support.
Patients were excluded if:
-
infection was diagnosed once the patient was placed in ECMO, and
-
patients required ECMO for other non-septic causes or were placed on ECMO mainly due to respiratory failure secondary to infection.
General management of septic shock
Our septic shock guidelines follow those published by Dellinger et al. [6]. These are clinical assessment, central venous oxygen saturation, lactate measurements, and echocardiography used to guide therapy. Once the patient is admitted to the unit, antibiotic infusion and volume loading with crystalloids are started. Cultures are taken before antibiotic infusion when possible. If there is no response to fluid therapy, vasoactive agents are indicated. Generally, dopamine, in neonates, and epinephrine (cold shock) or norepinephrine (warm shock), in children, are the first inotropic choices (Davis 2017) [5]. In cases of myocardial depression and low cardiac output with adequate blood pressure, dobutamine is used. If there is suspicion of suprarenal suppression, corticoid therapy at stress doses (50–100 mg/m2) is given. In newborns with signs of pulmonary hypertension, nitric oxide is started.
VA ECMO is set up when persistent shock with hypotension and progressive organ dysfunction occur despite previous support. Before ECMO entry, all patients undergo a functional echocardiography.
The evidence of severe and irreversible neurological findings is an exclusion criterion for VA ECMO. Cardiac arrest is not an exclusion criterion.
ECMO management
Patient cannulation is performed by trained surgeons, with general anesthesia in the intensive care unit. Cannulas are usually placed in the right jugular vein and the right carotid artery. In larger children, if there is need for greater flow, the femoral vein or artery may be also cannulated. The pumps used during the study period were Maquet® centrifugal pumps, and the membrane oxygenator was the Maquet Quadrox-iDpediatric®.
Currently, initial targeted flows are generally 150–200 ml/kg/min for newborns and 2.4 l/m2/min for children. Once the patient is placed in ECMO, individually directed target goals are normal lactate, venous oxygen saturation > 75%, mean arterial pressure (p50), and reversal of organ dysfunction. Input pressure is tolerated to 20 mmHg. Anticoagulation is administered with intravenous unfractionated heparin to maintain activated clotting time between 200 and 220 s. In cases of severe bleeding, clotting time target is reduced to 160 s. Platelet count is maintained above 100,000/mm3. When diuresis is < 0.5 ml/kg despite diuretic therapy, or when high volume of blood products is required, continuous renal replacement therapy (Prismaflex®) is started. Once ECMO is established, inotropes are weaned and ventilator settings, minimized.
Data collection
The following information was recorded for each patient:
Patient conditions and support immediately before ECMO: sex, age, weight, body surface, identified microorganism, infection site, antibiotic treatment, sepsis shock evolution time (defined as the time from sepsis diagnosis until ECMO start), cardiac arrest (CA) prior to ECMO, Sepsis Organ Failure Assessment (SOFA) score, Pediatric Risk Score of Mortality III (PRISM III) for pediatric patients, Score for Neonatal Acute Physiology Perinatal Extension II (SNAPPE II) for neonatal patients, mean airway pressure (MAP), positive end-expiratory pressure (PEEP), PaO2/FiO2 ratio, Oxygenation Index (OI), Vasoactive-Inotropic Score (VIS) (dopamine in mcg/kg/min + dobutamine in mcg/kg/min + milrinone 10× mcg/kg/min + noradrenaline 100× mcg/kg/min + adrenaline 100× mcg/kg/min), blood gas analyses, and blood lactate. Organic dysfunction was defined according to Goldstein B [8], and multiorganic dysfunction was defined when more than two organs were involved. Functional echocardiography was performed to evaluate left ventricular function and pulmonary hypertension, and left ventricle ejection fraction (LVEF) was recorded.
Analytical parameter evolution and hemodynamic support during ECMO: need for continuous veno-venous hemodiafiltration (CVVHDF), blood analyses with lactate, procalcitonin (PCT) and C-reactive protein (CRP), and VIS were evaluated at 24, 48, and 72 h, and percentage of Cardiac Index (CI) support at 24 and 48 h. ECMO complications such as thrombosis, bleeding, and circuit change were also recorded. Outcomes: mortality at hospital discharge, neurologic complications, total days on ECMO, days on MV, and ICU and hospital length of stay (LOS) were collected.
Patients were classified in two groups: pediatric patients and neonatal patients (those less than 7 days of life).
Statistics
In order to explore the sample, a descriptive statistical analysis of data was performed. Afterwards, a comparative analysis was made between pediatric and neonatal (those with less than 30 days of life) patients, between survivors and non-survivors, and between two equal periods of time (2001 to 2008 and 2009 to 2017). Quantitative variables were expressed as mean and standard deviation or median and interquartile range (IQR) (percentile 25–75), depending on the normal or non-normal distribution of the variables. Frequencies and percentages were used for qualitative variables. Data were compared using Student or Wilcoxon, or Fisher signed rank test, when variables had a normal or non-normal distribution, respectively. Descriptive analysis was performed overall for patients and also for separated groups, pediatric and neonatal. For the multivariate analysis, a logistic regression model was used, introducing variables with a p value < 0.1 in the univariate analysis. This was done with the total cohort of patients and then separately for the pediatric and neonatal groups.
The SPSS® 20.0 statistical software package (SPSS, Inc., Chicago II) was used. A p value under 0.05 was considered statistically significant, and the confidence interval (CI) was estimated using a confidence level of 95%.
The ECMO database was historically approved by the Institutional Review Board. The study was carried out in accordance with the Declaration of Helsinki, and it was approved by the Sant Joan de Déu Institutional Review Board. Written informed consent was not required due to the retrospective nature of the study and the previous approval of the database.
Results
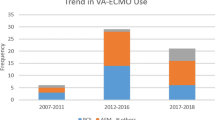
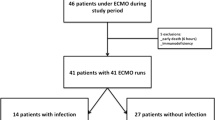
During the last 16 years, 156 ECMO procedures took place in our intensive care units. Of these patients, 21 (13.4%)—14 boys and 7 girls—underwent ECMO due to a refractory septic shock and were included in our study. Nine (42.8%) were pediatric patients and 12 (57.2%), newborns. Median age and weight in the pediatric group was 3.3 years (IQR, 0.7–4.7) and 15 kg (IQR, 8.3–17.5), respectively; in the neonatal group, the median age and weight were 1 day (IQR, 1–5) and 4.1 kg (IQR, 3.5–14.2). They were diagnosed with septic shock for a median duration of 29.5 hours (hrs) before ECMO was started (IQR, 20–46), with significant differences between the pediatric and neonatal groups (p = 0.02) (Table 2), and between the two periods of time (61.5 hrs IQR, 13.25–108.00 in the first period vs 11 hrs IQR, 5–22.5 p = 0.039 in the second) (Table 4). Only one pediatric patient had an underlying disease (non-cyanotic congenital heart disease: ventricle septal defect).
All patients had microbiological evidence of infection, and all of them were receiving the appropriate antibiotic before being placed in ECMO (Table 1). Among neonates, the most frequent microorganisms were S. agalactiae (33.3% of neonates) and E. coli (25%). In the pediatric population, 44.4% of the infections were due to S. pneumoniae.
Patient conditions and support immediately before ECMO
Before ECMO, all patients were intubated, connected to MV, and receiving inotropic support. Table 2 summarizes patient conditions and support before ECMO. The median PRISM III for pediatric patients at admission was 30.5 (IQR, 22.75–39.75), and for neonate patients, SNAPPE II was 95 (IQR, 48–103). We found statistical differences in SOFA score with worse scores in the in neonatal population (p = 0.01). There were no differences between the two time periods (Table 4). All patients had failure of at least three organ systems, with a median number of 4 (IQR, 3–5). Functional echocardiography was performed on all patients; a median LVEF of 27.3% (IQR, 12–56.3) was obtained, which was worse in the neonatal population with 21.3% (IQR, 10–28.5), p = 0.002. Moreover, the neonatal group also had pulmonary hypertension diagnosis and required inhaled nitric oxide (iNO) in 100% of cases.
All patients received infusions of at least two inotropes with a median of VIS 77.5 (IQR, 61.25–214.65) with no difference between the neonatal and pediatric groups. Moreover, 20 patients (95.2%) received hydrocortisone, and 13 patients (62%) received adrenaline boluses. Eleven patients (52.4%) suffered cardiac arrest (CA) and required external cardiac compressions immediately before or during ECMO cannulation, without differences between the two periods (Table 4).
In addition to the differences between groups mentioned above, there were also statistical differences in Oxygenation Index and PaO2/FiO2 ratio, blood gas analysis, and lactate levels, all of which were worse in the neonatal intensive care unit (NICU) patients.
Analytical parameter evolution and hemodynamic support during ECMO
During ECMO, 71.4% of the patients underwent continuous veno-venous hemodiafiltration, including all PICU patients (100%) and 41.6% of NICU patients (p = 0.014) (Table 3). Also, analytical parameters were monitored (lactate, CRP, and PCT) at 24, 48, and 72 h of ECMO. Lactate levels remained significantly higher in neonates, and analytical acute phase reactants were higher in in the pediatric intensive care unit (PICU) population although with no significant differences (Table 2). VIS score was significantly lower compared to the score before ECMO as expected. Median assistance at 24 and 48 h was 65% of the total CI. Assistance was higher in the second time period (Table 4).
Ten patients (47.6%) had mechanical problems with the ECMO circuit, without differences between NICU and PICU groups. All of them were episodes of clotting in the circuit requiring circuit changes, which is a reasonable occurrence after 7 days in ECMO but not earlier.
Outcome data
Nine patients (42.8%) survived to be decannulated from ECMO. Of the 12 deaths (57.1%), 6 patients (66.6%) were in PICU and 6 (50%) in NICU, 4 developed irreversible organ failure, 7 were certified brain dead, and 1 had a massive brain hemorrhage with treatment withdrawn. All patients with distributive septic shock (8) died, including the four cases of pediatric S. pneumoniae infection. If these patients with vasoplegic shock had been excluded as ECMO candidates, our global survival would have been 70% during the global period. No patient died after ECMO decannulation or required a second ECMO run. We noted an improvement in the survival of our patients from 14.3% during the first period to 57.2% during the second period (Table 4).
Of the nine survivors, only one had a small right brain stroke without clinical repercussion. The patient in question was from the first period, none of the patients from the second.
The median time on ECMO was 3.5 days (IQR, 1–5). If we exclude patients decannulated within the first 24 h either for fulminant evolution or due to brain death, the median time on ECMO was 5 days (IQR, 3.5–9) with no differences between AGE groups in any case. The median UCI and hospital LOS were 10 (IQR, 2.3–19) days and 10 (IQR, 2.3–39.5), respectively. Differences were not observed either in MV days, ICU admission, or LOS in the hospital between the neonatal and pediatric groups.
An analysis in order to detect predictors of mortality was performed (Table 4) comparing the previous variables between survival and non-survival groups, for the global patients and for the two time periods. In the global cohort of patients, longer evolution of sepsis and elevated values of MAP prior to ECMO, and persistent high levels of lactate at 48 h of ECMO were of greater note in the non-survivor group. Neither in neonatal nor in pediatric patients was cardiac arrest found to be a mortality predictor. Other variables, such as respiratory support parameters and hemodynamic requirements, had worse values in the mortality group, but without statistically significant differences. Concerning outcomes, no conclusion could be drawn due to premature mortality in the non-survivor group.
Multivariate analysis was not able to define any other independent risk factor for mortality.
Discussion
Our study shows that ECMO may be a useful tool for refractory septic shock. ECMO therapy should be considered in septic children with persistent catecholamine resistance shock. In patients with vasoplegic septic shock, this indication is less clear and should be evaluated with caution. As time might be an important predictor for survival, early transfer of patients with septic shock to an ECMO referral center for further evaluation is in order.
Until the last decade, ECMO for refractory septic shock was known for its high mortality and morbidity; hence, it was not recommended or was even contraindicated. Nevertheless, recent reports from MacLAren et al. included a survival rate between 47 and 75% [11, 19]. This success could be explained by the greater experience of the ECMO reference medical centers and the improvement in the equipment required to implement ECMO. Moreover, a recent Clinical Guideline by the American College of Critical Care Medicine rates ECMO as a suitable therapy in septic shock management [5]. In our study, we saw an improvement in the survival of our patients from 14.3% during the first 7 years to 57.2% during the last 8 years, and none of the survivors in the latter group had any neurological disability. Reliability was related to early retrieval from other centers, better candidate criteria excluding those patient’s affected by S. pneumoniae sepsis, and improved ECMO support.
Sepsis pathogenesis involves modulation of systemic inflammatory response which leads to hemodynamic dysfunction. Myocardial dysfunction occurs in 40–60% of septic patients [9]; it is characterized by ventricular dilatation and reduction of the left ventricle output and is more frequent in newborns and young children. Although ECMO is not curative, this therapy replaces heart and lung function temporarily and can be helpful in refractory septic shock patients with myocardial failure pattern [18]. Other patients, mainly older children and adults, may appear with vasoplegic septic shock. Revealing data suggest that, in these cases, ECMO may not be useful. In addition to age, pathogens may also establish the hemodynamic dysfunction pattern. In our study, S. pneumoniae sepsis, well known for its high cardiac output with refractory vasoplegia, like gram-negative bacteria [1], had a very poor outcome in ECMO (80% mortality). As suggested by MacLaren et al., central cannulation ECMO may be a solution for these cases because increased flows are possible [19].
No clear predictors of positive or negative outcome have been reported besides the association with central cannulation which achieves greater flows and survival [19]. Our patients were in very poor condition with high PRISM III (30.5 (IQR, 22.75–39.75)) and SNAPE II (95 (IQR, 48–103)) scores that predict risk of mortality higher than 80%, as in other reports [1]. In our study, those with longer sepsis evolution prior to ECMO (most of them transferred from other hospitals and with greater respiratory support and worse hemodynamic condition) had significantly less chance of survival. A recent study by Cvetkovic [3] showed that more than a half of the deaths of children referred to PICU with severe sepsis occurred during the first 24 h, and up to 26% of deaths occurred before PICU admission. Therefore, these patients should be transferred precociously to an ECMO center. Another suitable option is early retrieval by an ECMO team using a mobile ECMO service, especially for newborns with pulmonary hypertension and right ventricular failure [4].
Cardiac arrest before ECMO is considered by some adult reports a contraindication for ECMO as it is recognized as a mortality risk factor [14]. As in other recently published papers [20], our results, with a survival rate of 52.4%, show that cardiac arrest should not be an exclusion criterion in pediatric patients for ECMO therapy although neurological review should be done precociously.
The only infection-related mortality risk factor identified was the S. pneumoniae infection. Multivariate analysis was not able to define any other independent risk factor for mortality.
In our series, while PICU patients had a longer evolution in hours of sepsis, NICU patients had a worse condition before ECMO placement, in terms of oxygenation status and myocardial dysfunction, with higher lactate, but with no differences in survival. This could be explained by the presence of pulmonary hypertension as a sepsis response in this age group, which worsens the oxygenation status but is rapidly improved once ECMO is placed [16], leading to a better result once the patient is placed in ECMO, as explained above.
Our study has several important weaknesses. First, it is limited by its retrospective, observational, and single-center design. Data were collected from medical records which means that some data could be missing. Second, there is the limited meaning of performing statistical assessment on such a small sample. Nevertheless, apart from the McLaren group [2, 12], no larger series have been published. We acknowledge this, but we believe this is offset by the utility of these data.
In conclusion, patients with refractory septic shock should be transferred within hours of diagnosis to a referral ECMO center. However, therapy should be used with caution in patients with vasoplegic pattern shock, gram-negative infection, or S. pneumoniae sepsis. Further studies are required in order to detect other variables that could predict mortality.
Abbreviations
- CA:
-
Cardiac arrest
- CI:
-
Cardiac Index
- CVVHDF:
-
Continuous veno-venous hemodiafiltration
- ELSO:
-
Extracoporeal Life Support Organization
- iNO:
-
Inhaled nitric oxide
- LOS:
-
Hospital length of stay
- LVEF:
-
Left ventricle ejection fraction
- MAP:
-
Mean airway pressure
- MV:
-
Mechanical ventilation
- NICU:
-
Neonatal intensive care unit
- OI:
-
Oxygenation Index
- PCR:
-
Polymerase chain reaction
- PCT:
-
Procalcitonin
- PICU:
-
Pediatric intensive care unit
- PEEP:
-
Positive end-expiratory pressure
- PRISM III:
-
Pediatric Risk Score of Mortality III (PRISM III)
- SNAPPE II:
-
Score for Neonatal Acute Physiology Perinatal Extension II
- SOFA:
-
Sepsis Organ Failure Assessment score
- VA ECMO:
-
Veno-arterial extracorporeal membrane oxygenation
- VIS:
-
Vasoactive-Inotropic Score
- VV ECMO:
-
Veno-venous extracorporeal membrane oxygenation
References
Askim A, Mehl A, Paulsen J, DeWan AT, Vestrhiem DF, Asvold BO et al (2016) Epidemiology and outcome of sepsis in adult patients with Streptococcus pneumoniae infection in a Norwegian country 1993-2011: an observational study. BMC Infect Dis 16:223
Beca J, Butt W (1994) Extracorporeal membrane oxygenation for refractory septic shock in children. Pediatrics 93(5):726–729
Cvetkovic M, Lutman D, Ramnarayan P, Pathan N, Inwald DP, Peters MJ (2015) Timing of death in children referred for intensive care with severe sepsis: implications for interventional studies. Pediatr Crit Care Med 16:410–417
d’Aranda E, Pastene B, Ughetto F, Cotte J, Esnault P, Fouilloux V, Mazzeo C, Mancini J, Lebel S, Paut O (2016) Outcome comparison in children undergoing extracorporeal life support initiated at a local hospital by mobile cardiorespiratory assistance unit or at a referral center. Pediatr Crit Care Med 17(10):992–997
Davis LA, Carcillo JA, Aneja RK, Deymann AJ, Lin JC, Nguyen TC et al (2017) American college of critical care medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit Care Med 45(6):1061–1093
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM et al (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Intensive Care Med 39(2):165–228
Extracorporeal Life Support Organization (ELSO) (2018) ECLS registry, International summary
Goldstein B, Giroir B, Randolph A (2005) International Consensus Conference on Pediatric Sepsis: international pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 6(1):2–8
Inwald DP, Tasker RC, Peters MJ, Nadel S (2009) Emergency management of children with severe sepsis in the United Kingdom: the results of the Paediatric Intensive Care Society sepsis audit. Arch Dis Child 94(5):348–353
MacLaren G, Butt W (2011) Central extracorporeal membrane oxygenation for refractory pediatric septic shock. Pediatr Crit Care Med 12(5):606–607
MacLaren G, Butt W, Best D, Donath S, Taylor A (2007) Extracorporeal membrane oxygenation for refractory septic shock in children: one institution's experience. Pediatr Crit Care Med 8(5):447–451
McCune S, Short BL, Mille MK, Lotze A, Anderson KD (1990) Extracorporeal membrane oxygenation therapy in neonates with septic shock. J Pediatr Surg 25(5):479–482
Odetola FO, Gebremariam A, Freed GL (2007) Patient and hospital correlates of clinical outcomes and resource utilization in severe pediatric sepsis. Pediatrics 119:487–494
Park TK, Yang JH, Jeon K, Choi SH, Choi JH, Gwon HC et al (2014) Extracorporeal membrane oxygenation for refractory septic shock in adults. Eur J Cardiothorac Surg 47(2):68–74
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R et al (2017) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Crit Care Med 41(2):580–637
Roberts N, Westrope C, Pooboni SK, Mulla J, Peek GJ, Sosnowski AW et al (2003) Venovenous extracorporeal membrane oxygenation for respiratory failure in inotrope dependent neonates. ASAIO J 49(5):568–571
Shime N, Kawasaki T, Saito O, Akamine Y, Toda Y, Takeuchi M, Sugimura H, Sakurai Y, Iijima M, Ueta I, Shimizu N, Nakagawa S (2012) Incidence and risk factors for mortality in paediatric severe sepsis: results from the national paediatric intensive care registry in Japan. Intensive Care Med 38:1191–1197
Sivarajan VB, Almodovar MC, Rodefeld MD, Laussen PC (2013) Pediatric extracorporeal life support in specialized situations. Pediatr Crit Care Med 14(5_suppl):S51–S61
Tembo M, Harvey C, Duthie M, Pooboni S, Whitelaw J, Pandya H et al (2009) Extracorporeal membrane oxygenation for refractory septic shock in children: one institution’s experience. Pediatr Crit Care Med 10(4):534–535
Torres-Andres F, Fink EL, Bell MJ, Sharma MS, Yablonsky EJ, Sanchez-de-Toledo J (2018) Survival and long-term functional outcomes for children with cardiac arrest treated with extracorporeal cardiopulmonary resuscitation. Pediatr Crit Care Med 19:451–458. https://doi.org/10.1097/PCC.0000000000001524
Watson RS, Carcillo JA (2005) Scope and epidemiology of pediatric sepsis. Pediatr Crit Care Med 6(3):3–5
Acknowledgments
On behalf of the HSJD ECMO team, we thank Ana Morillo, Africa Pertierra, Cristina Carrasco, Ruth del Rio, Ana Alarcón, Mar Reyné, Montse Izquierdo, Marta Camprubí, Javier Mayol, Montse Castañón and all the nurse staffing. To all the children and their families treated by the HSJD ECMO team.
Author information
Authors and Affiliations
Contributions
Anna Solé, Sara Bobillo, Javier Rodríguez-Fanjul, and Iolanda Jordan conceived and designed the experiments. Anna Solé, Javier Rodríguez-Fanjul, Iolanda Jordan, and Monica Balaguer analyzed the data. Anna Solé, Javier Rodríguez-Fanjul, Julio Moreno, and Iolanda Jordan wrote the first draft of the manuscript. Susana Segura, Lluisa Hernandez-Platero, Francisco Jose Cambra, and Elisabeth Esteban contributed to the writing of the manuscript. All authors agree with the manuscript results and conclusions, jointly developed the structure and arguments for the paper, made critical revisions, and reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
This study was performed in its entirety at Hospital Sant Joan de Déu. The study was was carried out in accordance with the Helsinki Declaration and was approved by the Sant Joan de Déu Ethical Investigational Committee. The ECMO database was historically approved by the Institutional Review Board. Written informed consent was not required due to the retrospective nature of the study and the previous database approval.
Conflict of interest
The authors declare they have no conflict of interest.
Additional information
Communicated by Piet Leroy
Children and newborns with sepsis have significant mortality rates due to development of shock. ECMO is recommended in septic shock management but estimated survival is lower than 50%. It has not been stratified according to germ. In the present study, we have demonstrated that children with vasoplegic pattern shock or S. pneumoniae sepsis infection have poor outcomes while children with cold or warm septic shock achieve better outcomes.
Rights and permissions
About this article
Cite this article
Solé, A., Jordan, I., Bobillo, S. et al. Venoarterial extracorporeal membrane oxygenation support for neonatal and pediatric refractory septic shock: more than 15 years of learning. Eur J Pediatr 177, 1191–1200 (2018). https://doi.org/10.1007/s00431-018-3174-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3174-2