Abstract
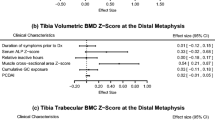
Low bone mineral density (BMD) and an increased fracture incidence are two extraintestinal complications associated with inflammatory bowel disease (IBD). We aimed to evaluate musculoskeletal traits and assess vertebral fracture (VF) rate in children and adolescents with IBD. Seventy patients with IBD with a median age of 13.8 years were included. The BMD and geometric parameters of the non-dominant tibia were assessed using pQCT. Dynamic muscle functions were evaluated using jumping mechanography. VFs were assessed according to the semiquantitative standardized method by Genant. The muscle functions adjusted for the patients’ weight did not differ from the reference population. A low trabecular BMD (Z-score − 1.6; p < 0.001) and cortical thickness (Z-score − 0.7; p < 0.001) were found in children and adolescents with IBD. Conversely, an increased cortical BMD (Z-score 1.1; p < 0.001) was noted. No significant association was found between the 25-OHD serum levels and the bone or muscle measurements. One patient with asymptomatic VF was identified.
Conclusion: IBD in childhood or adolescents affects bones but not muscles. Bone changes are independent of the 25-OHD serum level. A thoracolumbar spine X-ray should not be routinely recommended in children with IBD.
What is Known: • Low bone mineral density and an increased fracture rate are the complications associated with IBD. • Bone strength and structural development is strongly dependent on skeletal muscle stimulation. |
What is New: • Children with IBD have altered bone density and geometry but normal dynamic muscle functions. • Thoracolumbar spine X-ray should be indicated on an individual basis in children with IBD. |


Similar content being viewed by others
Abbreviations
- 25-OHD:
-
25-hydroxycholecalciferol
- BMC:
-
Bone mineral content
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- CRP:
-
C-reactive protein
- CSA:
-
Cross-sectional area
- DXA:
-
Dual energy X-ray absorptiometry
- F-calprotectin:
-
Fecal calprotectin
- IBD:
-
Inflammatory bowel disease
- M1LH:
-
Multiple one-legged hopping
- PCDAI:
-
Pediatric Crohn’s Disease Activity Index
- pQCT:
-
Peripheral quantitative computed tomography
- PTH:
-
Parathormone
- PUCAI:
-
Pediatric Ulcerative Colitis Activity Index
- S2LJ:
-
Single two-legged jump
- SSI:
-
Polar strength strain index
- VF:
-
Vertebral fracture
References
Levine A, Koletzko S, Turner D et al (2014) ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr 58:795–806. doi:10.1097/MPG.0000000000000239
Ruemmele FM, Veres G, Kolho KL et al (2014) Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J Crohn's Colitis 8:1179–1207. doi:10.1016/j.crohns.2014.04.005
Turner D, Levine A, Escher JC et al (2012) Management of Pediatric Ulcerative Colitis. J Pediatr Gastroenterol Nutr 55:340–361. doi:10.1097/MPG.0b013e3182662233
Song SM, Kim Y, Oh SH, Kim KM (2014) Nutritional status and growth in Korean children with Crohn’s disease: a single-center study. Gut Liver 8:500–507. doi:10.5009/gnl13183
Harpavat M, Greenspan SL, O’Brien C et al (2005) Altered bone mass in children at diagnosis of Crohn disease: a pilot study. J Pediatr Gastroenterol Nutr 40:295–300. doi:10.1097/01.mpg.0000153278.98861.32
Bechtold S, Alberer M, Arenz T et al (2010) Reduced muscle mass and bone size in pediatric patients with inflammatory bowel disease. Inflamm Bowel Dis 16:216–225. doi:10.1002/ibd.21021
Sabatier JP, Guaydier-Souquieres G, Laroche D et al (1996) Bone mineral acquisition during adolescence and early adulthood: a study in 574 healthy females 10–24 years of age. Osteoporos Int 6:141–148. doi:10.1007/bf01623938
Pappa H, Thayu M, Sylvester F et al (2011) Skeletal health of children and adolescents with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 53:11–25. doi:10.1097/MPG.0b013e31821988a3
Weinstein R, Jilka R, Parfitt A, Manolagas S (1998) Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. Potencial mechanism of their deleterious effects on bone. J Clin Invest 102:274–282. doi:10.1172/jci2799
Burnham JM, Shults J, Semeao E et al (2004) Whole body BMC in pediatric Crohn disease: independent effects of altered growth, maturation, and body composition. J Bone Min Res 19:1961–1968. doi:10.1359/jbmr.040908
Abraham BP, Prasad P, Malaty HM (2014) Vitamin D deficiency and corticosteroid use are risk factors for low bone mineral density in inflammatory bowel disease patients. Dig Dis Sci 59:1878–1884. doi:10.1007/s10620-014-3102-x
Veerappan SG, O’Morain CA, Daly JS, Ryan BM (2011) Review article: the effects of antitumour necrosis factor-α on bone metabolism in inflammatory bowel disease. Aliment Pharmacol Ther 33:1261–1272. doi:10.1111/j.1365-2036.2011.04667.x
Tsampalieros A, Berkenstock MK, Zemel BS et al (2014) Changes in trabecular bone density in incident pediatric Crohn’s disease: a comparison of imaging methods. Osteoporos Int 25:1875–1883. doi:10.1007/s00198-014-2701-x
Laakso S, Valta H, Verkasalo M, et al (2014) Compromised peak bone mass in patients with inflammatory bowel disease-a prospective study. J Pediatr 164:1436 – 1443.e1. doi: 10.1016/j.jpeds.2014.01.073
Ward LM, Rauch F, Matzinger MA et al (2010) Iliac bone histomorphometry in children with newly diagnosed inflammatory bowel disease. Osteoporos Int 21:331–337. doi:10.1007/s00198-009-0969-z
Dubner SE, Shults J, Baldassano RN et al (2009) Longitudinal assessment of bone density and structure in an incident cohort of children with Crohn’s disease. Gastroenterology 136:123–130. doi:10.1053/j.gastro.2008.09.072
Schmidt S, Mellström D, Norjavaara E et al (2009) Low bone mineral density in children and adolescents with inflammatory bowel disease: a population-based study from western Sweden. Inflamm Bowel Dis 15:1844–1850. doi:10.1002/ibd.20962
Wong SC, Catto-Smith AGA, Zacharin M (2014) Pathological fractures in paediatric patients with inflammatory bowel disease. Eur J Pediatr 173:141–151. doi:10.1007/s00431-013-2174-5
Cowan FJ, Parker DR, Jenkins HR (1995) Osteopenia in Crohn’s disease. Arch Dis Child 73:255–256
Semeao E, Stallings V, Peck S, Piccoli D (1997) Vertebral compression fractures in pediatric patients with Crohn’s disease. Gastroenterology 112:1710–1713. doi:10.1016/s0016-5085(97)70055-6
Lucarelli S, Borrelli O, Paganelli M et al (2006) Vertebral fractures and increased sensitivity to corticosteroids in a child with ulcerative colitis: successful use of pamidronate. J Pediatr Gastroenterol Nutr 43:533–535. doi:10.1097/01.mpg.0000249535.34676.d4
Thearle M, Horlick M, Bilezikian JP et al (2000) Osteoporosis: an unusual presentation of childhood Crohn’s disease. J Clin Endocrinol Metab 85:2122–2126. doi:10.1210/jc.85.6.2122
Kappelman MD, Galanko JA, Porter CQ, Sandler RS (2011) Risk of diagnosed fractures in children with inflammatory bowel diseases. Inflamm Bowel Dis 17:1125–1130. doi:10.1002/ibd.21472
Klaus J, Armbrecht G, Steinkamp M et al (2002) High prevalence of osteoporotic vertebral fractures in patients with Crohn’s disease. Gut 51:654–658. doi:10.1136/gut.51.5.654
Vestergaard P, Krogh K, Rejnmark L et al (2000) Fracture risk is increased in Crohn’s disease, but not in ulcerative colitis. Gut 46:176–181. doi:10.1136/gut.46.2.176
van Staa TP, Cooper C, Brusse LS et al (2003) Inflammatory bowel disease and the risk of fracture. Gastroenterology 125:1591–1597. doi:10.1053/j.gastro.2003.09.027
Frost HM (1987) Bone “mass” and the “mechanostat”: a proposal. Anat Rec 219:1–9. doi:10.1002/ar.1092190104
Hughes JM, Petit MA (2010) Biological underpinnings of frost’s mechanostat thresholds: the important role of osteocytes. J Musculoskelet Neuronal Interact 10:128–135
Boot AM, Bouquet J, Krenning EP, de Muinck Keizer-Schrama SM (1998) Bone mineral density and nutritional status in children with chronic inflammatory bowel disease. Gut 42:188–194. doi:10.1136/gut.42.2.188
Werkstetter KJ, Ullrich J, Schatz SB et al (2012) Lean body mass, physical activity and quality of life in paediatric patients with inflammatory bowel disease and in healthy controls. J Crohn's Colitis 6:665–673. doi:10.1016/j.crohns.2011.11.017
Thayu M, Denson LA, Shults J et al (2010) Determinants of changes in linear growth and body composition in incident pediatric Crohn’s disease. Gastroenterology 139:430–438. doi:10.1053/j.gastro.2010.04.044
Burnham JM, Shults J, Semeao E et al (2005) Body-composition alterations consistent with cachexia in children and young adults with Crohn disease. Am J Clin Nutr 82:413–420
Van Langenberg DR, Gatta P Della, Hill B, et al (2014) Delving into disability in Crohn’s disease: dysregulation of molecular pathways may explain skeletal muscle loss in Crohn’s disease. J Crohn's Colitis 8:626–634. doi: 10.1016/j.crohns.2013.11.024
Van Langenberg DR, Della Gatta P, Warmington SA et al (2014) Objectively measured muscle fatigue in Crohn’s disease: correlation with self-reported fatigue and associated factors for clinical application. J Crohn's Colitis 8:137–146. doi:10.1016/j.crohns.2013.07.006
Ahmed TA, Buzzelli MD, Lang CH et al (2007) Interleukin-6 inhibits growth hormone-mediated gene expression in hepatocytes. Am J Physiol - Gastrointest Liver Physiol 292:1793–1803. doi:10.1152/ajpgi.00547.2006
Kobzova J, Vignerova J, Blaha P et al (2004) The 6th nationwide anthropological survey of children and adolescents in the Czech Republic in 2001. Cent Eur J Public Health 12:126–130
Veilleux LN, Rauch F (2010) Reproducibility of jumping mechanography in healthy children and adults. J Musculoskelet Neuronal Interact 10:256–266
Sumnik Z, Matyskova J, Hlavka Z et al (2013) Reference data for jumping mechanography in healthy children and adolescents aged 6–18 years. J Musculoskelet Neuronal Interact 13:297–311
Moyer-Mileur LJ, Quick JL, Murray MA (2008) Peripheral quantitative computed tomography of the tibia: pediatric reference values. J Clin Densitom 11:1–12. doi:10.1016/j.jocd.2007.11.002
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148. doi:10.1002/jbmr.5650080915
Hyams JS, Ferry GD, Mandel FS et al (1991) Development and validation of a pediatric Crohn’s disease activity index. J Pediatr Gastroenterol Nutr 12:439–447
Turner D, Otley AR, Mack D et al (2007) Development, validation, and evaluation of a pediatric ulcerative colitis activity index: a prospective multicenter study. Gastroenterology 133:423–432. doi:10.1053/j.gastro.2007.05.029
Munns CF, Shaw N, Kiely M et al (2016) Global consensus recommendations on prevention and management of nutritional rickets. Horm Res Paediatr 85:83–106. doi:10.1159/000443136
R Core Team (2015) R: a language and environment for statistical computing.
Werkstetter KJ, Schatz SB, Alberer M et al (2013) Influence of exclusive enteral nutrition therapy on bone density and geometry in newly diagnosed pediatric Crohn’s disease patients. Ann Nutr Metab 63:10–16. doi:10.1159/000350369
Rauch F, Neu CM, Wassmer G et al (2002) Muscle analysis by measurement of maximal isometric grip force: new reference data and clinical applications in pediatrics. Pediatr Res 51:505–510. doi:10.1203/00006450-200204000-00017
Soucek O, Matyskova J, Anliker E et al (2015) The muscle-bone interaction in Turner syndrome. Bone 74:160–165. doi:10.1016/j.bone.2015.01.017
Anliker E, Rawer R, Boutellier U, Toigo M (2011) Maximum ground reaction force in relation to tibial bone mass in children and adults. Med Sci Sports Exerc 43:2102–2109. doi:10.1249/mss.0b013e31821c4661
Griffin LM, Thayu M, Baldassano RN et al (2015) Improvements in bone density and structure during snti-TNF-alpha therapy in pediatric Crohn’s disease. J Clin Endocrinol Metab 100:2630–2639. doi:10.1210/jc.2014-4152
Hradsky O, Soucek O, Maratova K et al (2017) Inflammatory Bowel Diseases Supplementation with 2 000 IU of cholecalciferol is associated with improvement of trabecular bone mineral density and muscle power in pediatric patients with IBD. Inflamm Bowel Dis 23:514–523. doi:10.1097/MIB.0000000000001047
Vázquez MA, Lopez E, Montoya MJ et al (2012) Vertebral fractures in patients with inflammatory bowel disease compared with a healthy population: a prospective case-control study. BMC Gastroenterol 12:47. doi:10.1186/1471-230x-12-47
Acknowledgements and funding
We would like to acknowledge all patients and their families who have participated in this study. Many thanks to Dr. Renata Mynarova for her expert vertebral fracture assessment as well as for scoring the deformities according to Genant.
This project was partially supported by the Ministry of Health, Czech Republic (Project for conceptual development of research organization 00064203; Motol University Hospital, Prague, Czech Republic) and by the Charles University Grant Agency (GAUK No. 136215, and No. 246216).
Authors’Contributions
Klara Maratova and Jana Matyskova performed the pQCT and mechanography assessment. Ondrej Hradsky provided the statistical analyses. Ivana Copova, Ondrej Hradsky, and Jiri Bronsky recruited the patients. Ondrej Soucek, Zdenek Sumnik, and Klara Maratova were responsible for interpretation of the data and drafted the paper. All co-authors revised the final version of the manuscript and approved it for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Peter de Winter
Rights and permissions
About this article
Cite this article
Maratova, K., Hradsky, O., Matyskova, J. et al. Musculoskeletal system in children and adolescents with inflammatory bowel disease: normal muscle force, decreased trabecular bone mineral density and low prevalence of vertebral fractures. Eur J Pediatr 176, 1355–1363 (2017). https://doi.org/10.1007/s00431-017-2988-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-017-2988-7