Abstract
HMV (home mechanical ventilation) in children has increased over the last years. The aim of the study was to assess perceived quality of life (QOL) of these children and their families as well as the problems they face in their daily life.
We performed a multicentric cross-sectional study using a semi-structured interview about the impact of HMV on families and an evaluation questionnaire about perceived QOL by the patient and their families (pediatric quality of life questionnaire (PedsQL4.0)). We studied 41 subjects (mean age 8.2 years). Global scores in PedsQL questionnaire for subjects (median 61.4), and their parents (median 52.2) were below those of healthy children. 24.4% received medical follow-up at home and 71.8% attended school. Mothers were the main caregivers (75.6%), 48.8% of which were fully dedicated to the care of their child. 71.1% consider economic and healthcare resources insufficient. All families were satisfied with the care they provide to their children, even though it was considered emotionally overwhelming (65.9%). Marital conflict and neglect of siblings appeared in 42.1 and 36% of families, respectively.
Conclusions: Perceived QOL by children with HMV and their families is lower than that of healthy children. Parents are happy to care for their children at home, even though it negatively affects family life.
What is Known: • The use of home mechanical ventilation (HMV) in children has increased over the last years. • Normal family functioning is usually disrupted by HMV. |
What is New: • The aim of HMV is to provide a lifestyle similar to that of healthy children, but perceived quality of life by these patients and their parents is low. • Most of the families caring for children on HMV agree that support and resources provided by national health institutions is insufficient. |
Similar content being viewed by others
Introduction
Home mechanical ventilation (HMV) in pediatric patients has increased over the last years [9, 10, 28]. HMV allows the patient to enjoy a lifestyle that tries to resemble that of healthy individuals at the cost of significant changes in family life [3, 5, 7, 12, 17, 18, 20,21,22, 32, 34]. HMV is supposed to improve the patients’ quality of life, but it has important social, psychological, physical, and financial consequences for the caregiver and the family. However, very few studies have objectively evaluated the quality of life of these patients and the impact of HMV on their caregivers [7, 12, 18, 22,23,24, 34, 35].
The establishment of healthcare policies with enough resources to guarantee timely provision of their needs for material and assistance directly influences the quality of care, impact on the families, and perceived quality of life. There are very few studies that evaluate the existence, effectiveness, and efficiency of these resources in children with HMV [5, 12, 21, 28, 31]. Some authors describe that the impact on the families is not related solely to the use of mechanical ventilation itself. It is probably more related to the severity of the child’s underlying condition and to the emotional functioning of the parents [13]. Despite these findings, it seems clear that HMV might add an extra burden to daily life in families with children on HMV.
Spain counts with a National Health, Social Services, and Equity Ministry. Nevertheless, public healthcare is provided by each of the 17 autonomous communities through their Regional Health Services (RHS). Each RHS may have its own specific attention programs, but global policies for attending technology-dependent population are very similar. Reference hospitals and subcontracted private companies are usually in charge of the care of home-ventilated patients. Medical care and nursing are usually provided by a primary care practitioner and hospital personnel through home hospitalization programs, palliative care programs, or through Intensive Care or Pneumology Departments giving ambulatory assistance. Only a few cases count with specific domiciliary attention programs. Ventilation devices, oxygen supply, and disposable material are home delivered by different private companies hired by each RHS. These companies must fulfill several requirements established by the regional administration. As healthcare service expenses are charged directly to the RHS, patients do not have to provide any funding. Some patients receive social and economic benefits from the regional administration due to their dependent condition. Financial burdens for both the public administrations and the families have been described by several authors [10, 11, 15, 28, 30, 31, 41].
The main objective of the study was to assess perceived quality of life of children with HMV and their families. The secondary objectives were to analyze the most frequent needs and problems that families face in their daily life and to evaluate satisfaction and functioning disruption experienced by these families.
Material and methods
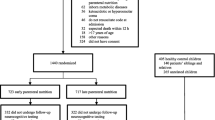
A multicentric cross-sectional study was carried out including 41 subjects between 1 month and 18 years of age with invasive and non-invasive HMV.
Subjects were selected from a 167-patient cohort of a previous multicentric study in which the epidemiology of pediatric HMV in Spain was described [9]. Twenty-five percent of the subjects recruited in the first study were included. Subjects belonged to 16 different hospitals, and the distribution of the subjects among hospitals was similar to that of the initial cohort. The physician in charge of their HMV follow-up selected the subjects.
Subjects and their parents were interviewed during their scheduled follow-up visits by the healthcare provider in charge of their HMV follow-up. The interview had two parts: first, the child and his parents completed the pediatric quality of life questionnaire (PedsQL) 4.0 [4, 36,37,38,39,40]. This questionnaire was designed and validated to assess health-related quality of life in pediatric patients. Second, a semi-structured open questionnaire was given to each participant (Table 1).
The PedsQL 4.0 questionnaire has several self-evaluating age-adapted questions about the child’s condition concerning different aspects: physical, emotional, social, and school. Global score and a specific psychosocial score including the emotional, social, and school dimensions can be calculated. Potential score ranges from 0 to 100 points. Higher scores reflect a better-perceived quality of life. PedsQL 4.0 questionnaire discriminates between healthy children and those with chronic health problems, reflecting the severity of their condition. The cut-off point for lesser quality of life has been set at a standard deviation below the mean population score: 83 ± 14.8 for self-reporting questions and 87.6 ± 12.3 for parent-reported questions [38]. Children with cognitive impairment who were not able to understand the age-appropriate questionnaire were asked to fill in the preceding age group questionnaire, as recommended by the PedsQL 4.0 administration guidelines. Even so, some patients with severe cognitive impairment were not able to understand any of the age group questionnaires. These cases were excluded from the analysis that compared self-reported scores and parent-proxy reported scores (as there were no self-reported scores).
The semi-structured open questionnaire was elaborated by the research team. Questions were focused on everyday organization of care at home, domiciliary medical follow-up and material delivery, patient’s daily activities, and the impact of domiciliary care on family life. The questions were based on previous reports on this topic and on the main difficulties that these families face according to the experience of the health providers in charge of their follow-up. The interviewer was provided with a booklet with the semi-structured open questionnaire for each patient. The booklet included blank spaces after each question. The nurse or doctor in charge of the patient carried out the interviews during a scheduled follow-up visit to the hospital. Interviewees were able to freely express themselves without time restrictions. Interviewers were instructed to conduct the interviews following the different topic blocks in the questionnaire and to write down detailed notes with their answers in the booklet. All completed booklets were then submitted to a single researcher who retrieved the data for analysis. This researcher analyzed all the notes in order to identify recurrent topics and similar responses between the different patients. Thus, some answers were categorized for semi-quantitative analysis.
SPSS 20.0 statistical package was used for the statistical analysis. Mean, median, and interquartile ranges were studied for each module in the PedsQL 4.0. Student’s t test was used to compare mean PedsQL scores with healthy population scores [39] after normal distribution of scores was confirmed using a Kolmogorv-Smirnov test. Ninety-five percent confidence intervals for the differences of means were calculated. The Mann-Whitney U test was used to compare mean scores between the different groups, and the Wilcoxon signed-rank test was used to compare self-reported and parent-reported paired scores. Statistical significance was considered for p < 0.05. Frequencies are described as both percentages and proportions expressing number of subjects and total responders.
Local Ethics Committee in each participating hospital approved the study, and written informed consent was obtained from the participants.
Results
Subjects and characteristics of families
Main patient’s characteristics are shown in Table 2. The most frequent underlying conditions were neuromuscular disease (56.1%, 23/41), encephalopathy (12.2%, 5/41), central hypoventilation syndrome (12.2%, 5/41), apnea-hypopnea sleep syndrome (4.9%, 2/41), and chronic respiratory disease (4.9%, 2/41). Other underlying conditions were present in 9.8% (4/41) of the subjects. Patient’s age was lower in the invasive ventilation group (median 6.1 IQR 2.9–8.8) than in the non-invasive ventilation group (median 10.1 IQR 7.1–13.0) (p = 0.016).
Perceived quality of life
Parent-proxy report was obtained in all subjects. Child report was obtained in 20 patients. Eight children were not able to answer any age group questionnaires due to severe cognitive impairment. Preceding age-group questionnaire was administered to one child with moderate cognitive impairment. Table 3 shows the scores for the PedsQL questionnaire and compares global and psychosocial scores of children and parents’ modules. Comparison is also made between the different age groups. Most dimensions scored low, but the physical health dimension scored the lowest in the evaluation of both patients and parents. Scores given by the patients were significantly higher than those given by the parents, although these differences were not found in children less than 13 years of age.
Table 4 compares, as described by Varny et al. [39], child and parent scores between ventilated patients and a healthy population sample. When comparing our results to those of chronic patients described by Varny et al. [39], our patients showed lower scores in all domains (p < 0.05) except for emotional functioning (p = 0.071), and school functioning (p = 0.058) in self-reports and for emotional functioning (p = 0.202) in parent reports.
No differences were found between different HMV modalities (Table 5), except in the physical health dimension in self-reported evaluations, where the scores given by non-invasively ventilated subjects were lower (12.5 points) than invasively ventilated subjects (75 points). There were no differences between groups in terms of daily time of ventilation.
Global scores given by the parents of patients with central hypoventilation syndrome were higher (p = 0.006) (median 75 IQR 67.1–90.4) than in the rest of diagnostic categories (median 49.7 IQR 39.1–68).
Global parent reported scores were lower in patients receiving specific domiciliary healthcare assistance (median 42 points IQR 33.7–51.2 points) than in those without it (median 59.8 IQR 42.8–71.7) (p = 0.05). Families receiving institutional social assistance had higher scores in the emotional domain (median 90 IQR 75–90) than those not receiving such assistance (median 75 IQR 50–80) (p = 0.013). The perception of domiciliary care as a financial burden was not related to higher or lower scores in any of the domains.
Results of the semi-structured open questionnaire:
Organization of domiciliary care, medical and respiratory company follow-up, and healthcare assistance
Table 6 shows how care is organized at home, how medical and respiratory companies program their follow-up visits, and what families do when an acute problem arises.
Daily life adaptation and schooling
Figure 1 shows how well HMV patients perform in everyday activities. Out of 33 (81.8%) school-aged patients (over 3 years old in Spain), 27 attended school, and 75% (25/33) of them had special education needs. Schooled subjects were in their corresponding grade in 65.4% of cases (17/26). Of 30 patients, 12 (40%) attended special education centers, and 21.2% (7/33) received classes at home. Among patients receiving classes at home, families were satisfied with the schooling they received in 71.4% of cases (5/7).
Of 41 families (70.7%), 29 were able to go out on vacation. The rest did not do so because of the medical condition of the patient. Only 2 of the 41 families (4.9%) received some assistance in order to be able to go on vacation.
Ten percent (4/40) of the interviewed caregivers reported behavioral problems in their children, and 7.5% (3/40) considered that it is difficult to look after them. Of 38 (10.5%) responders, 4 say that their children get upset very often. Most of the subjects (74.3%, 26/35) did not complain about being ill, and 12.7% (4/34) confessed being afraid of their own illness.
Social and institutional support
The assistance the families receive is perceived as insufficient by 53.8% (21/39) of them: 31.2% (9/28) considered they need a healthcare assistant, 28.6% (8/28) demand more economic benefits or transfer-related assistance, and 28.6% (8/28) need their home adapted.
Of 39 (59%) families, 23 claimed that the social assistance they receive from different institutions is insufficient, and 71.1% (27/38) of them consider that the economic benefits are also insufficient. Taking care of these patients at home is an economic burden for 70% (28/40) of the families.
Families stayed in contact with different patient support groups and organizations in 35.9% (14/39) of the cases, and 43.6% (17/39) of them did so with other families with children on HMV. Friends and relatives perceived the situation with normality in 42.9% (15/35) of the cases, with resignation in 17.1% (6/35), and it was considered a problem for 14.3% (5/35) of them. Interviewees considered in 11.4% (4/35) that the rest of the family and friends were not sufficiently involved in the care of these patients.
Satisfaction and repercussions on the families
All the interviewed families were happy to have their child at home, and they thought it was the best option for the welfare of their child. Nevertheless, one family out of 39 (2.6%) confessed it was not the best situation for the family. Families felt that they had been part of the decision of caring for their child at home in 88.9% of cases (32/36).
Their greatest concern was the progression of the disease of their child (47.1%, 16/34), the onset of life-threatening situations (17.6%, 6/34), the impossibility of having a normal lifestyle (11.8%, 4/34), and the impossibility of providing appropriate care (11.8%, 4/34). 32.4% (11/34) of them confessed that this concern affected them continuously.
The care for these patients at home was considered an emotional burden for 65.9% (27/41) of the families, requiring psychological assistance in 24.4% (10/41) of the cases. It caused marital conflicts in 42.1% (16/38) of the families, and 12.5% (3/24) of the parents with other children felt they did not provide enough care for their other children. Siblings demanded more attention from their parents in 36% (9/25).
Discussion
Reported median PedsQL 4.0 global scores from our population (both child and parent-reported) were below those reported by healthy population [39]. Moreover, perceived quality of life in our sample was lower than that of other patients with chronic conditions. All our patients are HMV users, but we cannot assume that HMV is the only determinant for a decreased perceived quality of life. Perhaps, the underlying medical condition that leads to the need of respiratory support plays an important role in a decreased perceived quality of life.
More than half of the patients in our study with HMV had neuromuscular diseases, which is in accordance with other studies [1, 2, 6, 8, 10, 15, 16, 26, 28, 29, 41]. Global scores for perceived quality of live given by the parents were below those reported by the patients [38, 39]. Scores were low in all age groups. It is important to highlight that the scores concerning the physical sphere were lower than the other domains. Interestingly, this score is even lower in children with non-invasive mechanical ventilation (NIMV).
It is not clear how age affects the perception of health-related quality of life. According to our data, perceived quality of life differs in the different age groups: scores on the physical dimension seem to decrease as age increases. This does not seem to occur in the other dimensions. Perhaps being older and more aware of their situation has a negative impact in their perceived quality of life, or, perhaps, the underlying disease is different in older patients. Nevertheless, the scores given by their families were also lower in children with NIMV. Perhaps, older children have a longer time of progression of the disease and a worse clinical condition. Moreover, the use of NIMV is a palliative resource in some patients with degenerative diseases. This might explain, in part, the differences in perceived quality of life at different ages. Specific needs in the physical, social, and emotional spheres are different and are influenced by different factors at different ages. Smaller children are probably less affected in the social and emotional dimension, as their social interactions are limited, basically, to family members, whereas the social circle of older children is broader and includes people outside the family not directly involved with their care.
It is also interesting that parents perceived a worse quality of life than the patients themselves did. Several studies have explored this fact. Noyes used the KINDL questionnaire to compare perceived quality of life in 17 pairs of parents and ventilator-dependent children [24]. This study did not find any differences in overall scores, but they did in social (relationships with friends) and disease scores in which parents reported lower scores than children. Paditz et al. developed their own questionnaire to assess health-related quality of life in 62 German children with ventilation (mostly non-invasive) with a mean age of 14.8 years [27]. They found that children felt better about their lives than what parents thought. Lumeng et al. also used their own questionnaire to evaluate 38 children in the USA [19]. In this case, self-report was only given to children over 12 years, and they did not find any differences between parent and child reports. Our study includes a wider range of patient age than the studies of Paditz and Lumeng et al. It also includes a wider range of ventilation modalities than Noyes and Paditz studies. We did find differences in the overall scores given by the children and by the parents in all except the 8–12-year group. We also found that reported psychosocial, emotional, and social scores were significantly lower by the parents of children over 12 years, which supports the conclusions of Noyes’s study. Some may think that smaller children are not aware of their limitations, but our data show a different interpretation of this fact, since these differences are more obvious and more significant in children older than 13 years. Perhaps parents are more aware that their children are supposed to be more independent at this age.
Graham et al. [12] have recently published a study evaluating health-related quality of life on a cohort of 86 children on home mechanical ventilation and their caregivers. They used the Child Health Ratings Inventories to evaluate health-related quality of life, which is a validated tool including 20 items regarding three dimensions (physical function, role function, and emotional well-being) with different age-adapted versions. Our study has a similar proportion of patients ventilated through tracheostomy (50%) and patients with congenital diseases (69%). As an important difference, our study has evaluated and compared patient’s self-reported and parent proxy-reported quality of life. Both studies show lower scores than those obtained by healthy children and other patients with chronic conditions. As another remarkable difference, our study includes patients from multiple centers and different regions as opposed to Graham’s single-center study, thus reflecting geographical and clinical variations in the management and care of these patients.
The mother usually assumes the role of the main caregiver. As these patients require full attention during many hours a day, main caregivers are usually forced to quit their jobs, as reported by different studies [12, 18, 21, 22, 32, 33]. Meltzer et al. found that caring for a child with chronic medical conditions causes an alteration in the sleep pattern of the mother, which is associated with depression and fatigue [21, 22]. Other studies report a negative impact on the mother concerning healthy habits [18], employment, and health [32, 33].
Very few patients have health assistance from outside the family on a daily basis, even though most of them receive economic benefits from the government. Financial and human resources are insufficient, as perceived by most of the families in our studies, as reported by other studies [3, 7, 20, 21, 25, 31, 32]. It is important to point out that Spain accounts with different RHS. This means that, even though there are some national regulations about the care of the dependent patient, each region provides its own resources, and there are no nationwide standards about how this care should be provided. Establishing nationwide standards of care could improve attention of HMV patients making the access to the different resources more equitable and accessible. Our study shows that more attention should be paid to home medical follow-up, as only a small number of patients benefit from it. On the other hand, a high percentage of families are satisfied with the performance of respiratory device companies. Most of the patients in our study assisted school. Thus, human and material resources should be destined to adapt education centers to the special needs of these patients.
Our study shows that subjects with HMV have a great dependence in activities of daily living. This dependency causes an overwhelming feeling of responsibility on caregivers that may lead to a negative way of experiencing this situation [5]. Families report insufficient social and institutional support. In many occasions, they find support in patient associations or other families of children with similar conditions. Mah et al. report the importance of minimizing the isolation of these families in order to control the stress derived from the care of these patients [20]. O’Brien et al. highlight the importance of preserving social and family relationships in order to diminish the feeling of isolation. They also insist in the benefit of keeping contact with other families in similar conditions to share experiences, information on different treatments, care, and family functioning [25].
Our study shows that these families are satisfied with the fact of being responsible for the care of their children. Although only a few caregivers show concerns about giving an appropriate care (from the parent’s point of view), most of them point out important difficulties and burdens related to the care of HMV children. Caring for their children has negative implications such as marital conflict, emotional overload, or the feeling of neglecting their other children. Several factors beside the clinical condition of the child have been proposed to be involved in the negative effect of HMV in family functioning. Increased family expenditures directly related to the costs of home care and decreased incomes due to caregiver voluntary or involuntary loss of employment have been described as strong factors of family dysfunction. Other emotional factors as chronic fatigue or facing stressful situations like medical emergencies or life-threatening events might as well be involved [3, 5, 12,13,14, 17, 25, 32, 34]. A high proportion of the caregivers in our study were concerned about the appearance of marital conflicts or about neglecting other siblings. This can be interpreted as a sign of family dysfunction and can be due, in part, to the lack of support that caregivers receive [21]. Other authors have also reported these negative consequences on caregivers, revealing the need to establish social and psychological support for these families [3, 20, 25]. Caregiver emotional functioning is directly related to family functioning, as described in many studies. The way the caregiver perceives their child’s quality of life is affected by the caregiver’s own emotional functioning [12, 13]. This relationship probably works in both directions: children with better perceived quality of life would have parents with better emotional functioning and parents with better emotional skills would, presumably, be able to provide better care for their children, thus improving their quality of life. Resources should be granted not only to guarantee good medical attention and provide respiratory care supplies for the patient, but to prevent or minimize the negative effects on family functioning.
Study limitations
Our study has several limitations. Our sample is relatively small, though larger than other studies [3, 7, 20]. Ideally, all the patients from initial cohort of 167 patients [9] should be included in this study. This was not possible due to limited resources, so the actual study population was set at 25% of the previous one. In order to minimize patient selection bias, the proportion of subjects was preserved like that of the previous study. Nevertheless, the physicians in charge of their follow-up selected the patients, and their participation was voluntary. Thus, a biased selection cannot be discarded.
The use of a semi-structured questionnaire interview as a mean to obtain information about the impact of HMV on family functioning might condition parents to focus their attention on several topics proposed by the investigators and thus leaving other topics out of the interview.
Finally, the study is based on a Spanish pediatric population with HMV. For this reason, the results should be extrapolated carefully to other countries with different social and healthcare resources and infrastructure.
Conclusions
Perceived quality of life of children with HMV and their parents is significantly worse than that of healthy children. Parents are satisfied with caring for them at home, but it has a negative impact on their personal and family life. This is probably due to an insufficient support from institutions. Thus, it is imperative to develop and implement specific programs involving health, financial, psychological, and social (including school) resources to support patients with HMV and their families.
Abbreviations
- HMV:
-
Home mechanical ventilation
- IQR:
-
Interquartile range
- NIMV:
-
Non-invasive mechanical ventilation
- QOL:
-
Quality of life
- RHS:
-
Regional Health Service
References
Appierto L, Cori M, Bianchi R, Onofri A, Catena S, Ferrari M, Villani A (2002) Home care for chronic respiratory failure in children: 15 years experience. Paediatr Anaesth 12:345–350
Bertrand P, Fehlmann E, Lizama M, Holmgren N, Silva M, Sánchez I (2006) Home ventilatory assistance in Chilean children: 12 years’ experience. Arch Bronconeumol 42:165–170
Carnevale FA, Alexander E, Davis M, Rennick J, Troini R (2006) Daily living with distress and enrichment: the moral experience of families with ventilator-assisted children at home. Pediatrics 117:e48–e60. doi:10.1542/peds.2005-0789
Chan KS, Mangione-Smith R, Burwinkle TM, Rosen M, Varni JW (2005) The PedsQL: reliability and validity of the short-form generic core scales and Asthma Module. Med Care 43:256–265
Dybwik K, Tollåli T, Nielsen EW, Brinchmann BS (2011) “Fighting the system”: families caring for ventilator-dependent children and adults with complex health care needs at home. BMC Health Serv Res 11:156. doi:10.1186/1472-6963-11-156
Edwards EA, Hsiao K, Nixon GM (2005) Paediatric home ventilatory support: the Auckland experience. J Paediatr Child Health 41:652–658. doi:10.1111/j.1440-1754.2005.00753.x
Evans R, Catapano MA, Brooks D, Goldstein RS, Avendano M (2012) Family caregiver perspectives on caring for ventilator-assisted individuals at home. Can Respir J 19:373–379
Fauroux B, Boffa C, Desguerre I, Estournet B, Trang H (2003) Long-term noninvasive mechanical ventilation for children at home: a national survey. Pediatr Pulmonol 35:119–125. doi:10.1002/ppul.10237
González Cortés R, Bustinza Arriortua A, Pons Ódena M, García Teresa MA, Cols Roig M, Gaboli M, García Martinez S, Oñate Vergara E, García Urabayen D, Castillo Serrano A et al (2013) Domiciliary mechanical ventilation in children: a Spanish multicentre study. An Pediatr (Barc) 78:227–233. doi:10.1016/j.anpedi.2012.06.011
Graham RJ, Fleegler EW, Robinson WM (2007) Chronic ventilator need in the community: a 2005 pediatric census of Massachusetts. Pediatrics 119:e1280–e1287. doi:10.1542/peds.2006-2471
Graham RJ, McManus ML, Rodday AM, Weidner RA, Parsons SK (2017) Chronic respiratory failure: utilization of a pediatric specialty integrated care program. Healthc (Amst) 5:23–28. doi:10.1016/j.hjdsi.2016.04.002
Graham RJ, Rodday AM, Parsons SK (2014) Family-centered assessment and function for children with chronic mechanical respiratory support. J Pediatr Health Care 28:295–304. doi:10.1016/j.pedhc.2013.06.006
Graham RJ, Rodday AM, Weidner RA, Parsons SK (2016) The impact on family of pediatric chronic respiratory failure in the home. J Pediatr 175:40–46. doi:10.1016/j.jpeds.2016.05.009
Heaton J, Noyes J, Sloper P, Shah R (2005) Families’ experiences of caring for technology-dependent children: a temporal perspective. Health Soc Care Community 13:441–450. doi:10.1111/j.1365-2524.2005.00571.x
Jardine E, O’Toole M, Paton JY, Wallis C (1999) Current status of long term ventilation of children in the United Kingdom: questionnaire survey. BMJ 318:295–299
Kamm M, Burger R, Rimensberger P, Knoblauch A, Hammer J (2001) Survey of children supported by long-term mechanical ventilation in Switzerland. Swiss Med Wkly 131:261–266
Kuster PA, Badr LK (2006) Mental health of mothers caring for ventilator-assisted children at home. Issues Ment Health Nurs 27:817–835. doi:10.1080/01612840600840588
Kuster PA, Badr LK, Chang BL, Wuerker AK, Benjamin AE (2004) Factors influencing health promoting activities of mothers caring for ventilator-assisted children. J Pediatr Nurs 19:276–287. doi:10.1016/j.pedn.2004.05.009
Lumeng JC, Warschausky SA, Nelson VS, Augenstein K (2001) The quality of life of ventilator-assisted children. Pediatr Rehabil 4:21–27
Mah JK, Thannhauser JE, McNeil DA, Dewey D (2008) Being the lifeline: the parent experience of caring for a child with neuromuscular disease on home mechanical ventilation. Neuromuscul Disord 18:983–988. doi:10.1016/j.nmd.2008.09.001
Meltzer LJ, Boroughs DS, Downes JJ (2010) The relationship between home nursing coverage, sleep, and daytime functioning in parents of ventilator-assisted children. J Pediatr Nurs 25:250–257. doi:10.1016/j.pedn.2009.01.007
Meltzer LJ, Mindell JA (2006) Impact of a child’s chronic illness on maternal sleep and daytime functioning. Arch Intern Med 166:1749–1755. doi:10.1001/archinte.166.16.1749
Noyes J (2006) Health and quality of life of ventilator-dependent children. J Adv Nurs 56:392–403. doi:10.1111/j.1365-2648.2006.04014.x
Noyes J (2007) Comparison of ventilator-dependent child reports of health-related quality of life with parent reports and normative populations. J Adv Nurs 58:1–10. doi:10.1111/j.1365-2648.2006.04191.x
O’Brien ME (2001) Living in a house of cards: family experiences with long-term childhood technology dependence. J Pediatr Nurs 16:13–22. doi:10.1053/jpdn.2001.20548
Oktem S, Ersu R, Uyan ZS, Cakir E, Karakoc F, Karadag B, Kiyan G, Dagli E (2008) Home ventilation for children with chronic respiratory failure in Istanbul. Respiration 76:76–81. doi:10.1159/000110801
Paditz E, Zieger S, Bickhardt J, Bockelbrink A, Grieben U, Hammer J, Kemper A, Knape H, Laier-Groeneveld G, Mellies U et al (2000) Self-reported quality of life in home mechanical ventilation in childhood, adosescence and young adulthood: differences between parents and children. Somnologie 4:13–19. doi:10.1046/j.1439-054x.2000.00118.x
Paulides FM, Plötz FB, Verweij-van den Oudenrijn LP, van Gestel JPJ, Kampelmacher MJ (2012) Thirty years of home mechanical ventilation in children: escalating need for pediatric intensive care beds. Intensive Care Med 38:847–852. doi:10.1007/s00134-012-2545-9
Racca F, Bonati M, Del Sorbo L, Berta G, Sequi M, Capello EC, Wolfler A, Salvo I, Bignamini E, Ottonello G et al (2011) Invasive and non-invasive long-term mechanical ventilation in Italian children. Minerva Anestesiol 77:892–901
Rodday AM, Graham RJ, Weidner RA, Terrin N, Leslie LK, Parsons SK (2017) Predicting health care utilization for children with respiratory insufficiency using parent-proxy ratings of children’s health-related quality of life. J Pediatr Health Care. doi:10.1016/j.pedhc.2017.04.021
Sevick MA, Kamlet MS, Hoffman LA, Rawson I (1996) Economic cost of home-based care for ventilator-assisted individuals: a preliminary report. Chest 109:1597–1606
Thyen U, Kuhlthau K, Perrin JM (1999) Employment, child care, and mental health of mothers caring for children assisted by technology. Pediatrics 103:1235–1242
Thyen U, Terres NM, Yazdgerdi SR, Perrin JM (1998) Impact of long-term care of children assisted by technology on maternal health. J Dev Behav Pediatr 19:273–282
Toly VB, Musil CM, Carl JC (2012) Families with children who are technology dependent: normalization and family functioning. West J Nurs Res 34:52–71. doi:10.1177/0193945910389623
Toly VB, Musil CM, Carl JC (2012) A longitudinal study of families with technology-dependent children. Res Nurs Health 35:40–54. doi:10.1002/nur.21454
Varni JW, Burwinkle TM, Seid M, Skarr D (2003) The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 3:329–341
Varni JW, Limbers CA (2009) The PedsQL 4.0 generic core scales young adult version: feasibility, reliability and validity in a university student population. J Health Psychol 14:611–622. doi:10.1177/1359105309103580
Varni JW, Seid M, Knight TS, Uzark K, Szer IS (2002) The PedsQL 4.0 generic core scales: sensitivity, responsiveness, and impact on clinical decision-making. J Behav Med 25:175–193
Varni JW, Seid M, Kurtin PS (2001) PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 39:800–812
Varni JW, Seid M, Rode CA (1999) The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 37:126–139
Wallis C, Paton JY, Beaton S, Jardine E (2011) Children on long-term ventilatory support: 10 years of progress. Arch Dis Child 96:998–1002. doi:10.1136/adc.2010.192864
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study design and data collection. Each author collected data from the patients of their respective setting. Rafael González, Amaya Bustinza, Sarah N. Fernández, and Jesús López-Herce elaborated the manuscript drafting. All authors were able to propose changes on manuscript draft and approved final version of the manuscript.
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Local Ethics Committee in each participating hospital approved the study, and written informed consent was obtained from the participants.
Conflict of interest
The authors declare that they have no conflicts of interest.
Financial support
This study has been performed by grant (2009/024) from SEPAR (Spanish Society of Pneumology and Thoracic Surgery). Funding source had no involvement either on study design, collection, analysis and interpretation of data, manuscript writing or article submission for publishing.
Additional information
Communicated by Patrick Van Reempts
Rights and permissions
About this article
Cite this article
González, R., Bustinza, A., Fernandez, S.N. et al. Quality of life in home-ventilated children and their families. Eur J Pediatr 176, 1307–1317 (2017). https://doi.org/10.1007/s00431-017-2983-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-017-2983-z