Abstract
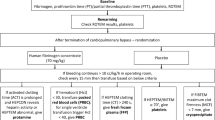
Transfusion guidelines have been produced for the evidence-based use of fresh frozen plasma (FFP). However, the inappropriate use of FFP is still a worldwide problem, especially in the prophylactic settings. In the present study, 100 cyanotic pediatric patients (age 6 months to 3 years) undergoing cardiac surgery with cardiopulmonary bypass (CPB) were randomized to receive either 10–20 ml/kg FFP (FFP group, n = 50) or 10–20 ml/kg 4 % succinylated gelatin (Gelofusine, GEL group, n = 50) in the priming solution. Rapid thromboelastography (r-TEG) was measured before skin incision and 15 min after heparin neutralization. Postoperative renal and hepatic function, mediastinal chest tube drainage, transfusion requirements, and recovery time were observed. The relationships between hematologic and demographic data and postoperative bleeding volume were also analyzed. The results showed that there were significantly elevated levels of fibrinogen (r-TEG parameters: fibrinogen contribution to maximal amplitude (MAf) and fibrinogen level (FLEV)) in the FFP group compared to the GEL group. The postoperative blood loss, total transfusion requirements, and recovery time were not significantly different between the two groups, indicating that there were no obvious clinical benefits of using FFP in the priming. The maximal amplitude (MA) of r-TEG measured after heparin neutralization was correlated with the 6-h postoperative bleeding volume. In addition, preoperative fibrinogen level rather than FFP priming was an independent predictor of postoperative blood loss. Conclusion: Prophylactic use of FFP in the priming solution does not have obvious clinical benefits in cyanotic congenital heart disease (CCHD) patients. Gelofusine, an artificial colloid, is a safe and effective substitute of FFP in the priming solution. Furthermore, r-TEG can be used as a “real-time” assessment tool to evaluate postoperative bleeding and guide transfusion after cardiac surgery in pediatric patients.

Similar content being viewed by others

Abbreviations
- CPB:
-
Cardiopulmonary bypass
- CCHD:
-
Cyanotic congenital heart disease
- FFP:
-
Fresh frozen plasma
- FLEV:
-
Fibrinogen level
- MA:
-
Maximal amplitude
- MAf:
-
Fibrinogen contribution to maximal amplitude
- MAp:
-
Platelet contribution to maximal amplitude
- R :
-
Reaction time
- r-TEG:
-
Rapid thromboelastography
References
Cui Y, Hei F, Long C, Feng Z, Zhao J, Yan F, Wang Y, Liu J (2010) Perioperative monitoring of thromboelastograph on blood protection and recovery for severely cyanotic patients undergoing complex cardiac surgery. Artif Organs 34:955–960. doi:10.1111/j.1525-1594.2010.01148.x
Eaton MP, Iannoli EM (2011) Coagulation considerations for infants and children undergoing cardiopulmonary bypass. Paediatr Anaesth 21:31–42. doi:10.1111/j.1460-9592.2010.03467.x
Gielen C, Dekkers O, Stijnen T, Schoones J, Brand A, Klautz R, Eikenboom J (2013) The effects of pre- and postoperative fibrinogen levels on blood loss after cardiac surgery: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. doi:10.1093/icvts/ivt506
Girdauskas E, Kempfert J, Kuntze T, Borger MA, Enders J, Fassl J, Falk V, Mohr FW (2010) Thromboelastometrically guided transfusion protocol during aortic surgery with circulatory arrest: a prospective, randomized trial. J Thorac Cardiovasc Surg 140(1117–1124):e1112. doi:10.1016/j.jtcvs.2010.04.043
Golab HD, Bogers JJ (2009) Small, smaller, smallest. Steps towards bloodless neonatal and infant cardiopulmonary bypass. Perfusion 24:239–242. doi:10.1177/0267659109348722
Golab HD, Takkenberg JJ, Bogers AJ (2010) Specific requirements for bloodless cardiopulmonary bypass in neonates and infants; a review. Perfusion 25:237–243. doi:10.1177/0267659110375862
Goldschmidt B (1973) Blood coagulation and platelet abnormalities in cyanotic congenital heart-disease. Lancet 1:607
Gurbuz HA, Durukan AB, Salman N, Tavlasoglu M, Durukan E, Ucar HI, Yorgancioglu C (2013) Hydroxyethyl starch 6 %, 130/0.4 vs. a balanced crystalloid solution in cardiopulmonary bypass priming: a randomized, prospective study. J Cardiothorac Surg 8:71. doi:10.1186/1749-8090-8-71
Holcomb JB, Minei KM, Scerbo ML, Radwan ZA, Wade CE, Kozar RA, Gill BS, Albarado R, McNutt MK, Khan S, Adams PR, McCarthy JJ, Cotton BA (2012) Admission rapid thrombelastography can replace conventional coagulation tests in the emergency department: experience with 1974 consecutive trauma patients. Ann Surg 256:476–486. doi:10.1097/SLA.0b013e3182658180
Lang T, Bauters A, Braun SL, Potzsch B, von Pape KW, Kolde HJ, Lakner M (2005) Multi-centre investigation on reference ranges for ROTEM thromboelastometry. Blood Coagul Fibrinolysis 16:301–310
Lee JW, Yoo YC, Park HK, Bang SO, Lee KY, Bai SJ (2013) Fresh frozen plasma in pump priming for congenital heart surgery: evaluation of effects on postoperative coagulation profiles using a fibrinogen assay and rotational thromboelastometry. Yonsei Med J 54:752–762. doi:10.3349/ymj.2013.54.3.752
McCall MM, Blackwell MM, Smyre JT, Sistino JJ, Acsell JR, Dorman BH, Bradley SM (2004) Fresh frozen plasma in the pediatric pump prime: a prospective, randomized trial. Ann Thorac Surg 77:983–987. doi:10.1016/j.athoracsur.2003.09.030, discussion 987
Oliver WC Jr., Beynen FM, Nuttall GA, Schroeder DR, Ereth MH, Dearani JA, Puga FJ (2003) Blood loss in infants and children for open heart operations: albumin 5 % versus fresh-frozen plasma in the prime. Ann Thorac Surg 75:1506–1512. doi:10.1016/S0003-4975(02)04991-3
O'Shaughnessy DF, Atterbury C, Bolton Maggs P, Murphy M, Thomas D, Yates S, Williamson LM, British Committee for Standards in Haematology BTTF (2004) Guidelines for the use of fresh-frozen plasma, cryoprecipitate and cryosupernatant. Br J Haematol 126(1):11–28. doi:10.1111/j.1365-2141.2004.04972.x
Puetz J, Witmer C, Huang YS, Raffini L (2012) Widespread use of fresh frozen plasma in US children’s hospitals despite limited evidence demonstrating a beneficial effect. J Pediatr 160(210–215):e211. doi:10.1016/j.jpeds.2011.08.013
Stanworth SJ, Brunskill SJ, Hyde CJ, McClelland DB, Murphy MF (2004) Is fresh frozen plasma clinically effective? A systematic review of randomized controlled trials. Br J Haematol 126:139–152. doi:10.1111/j.1365-2141.2004.04973.x
Stanworth SJ, Grant-Casey J, Lowe D, Laffan M, New H, Murphy MF, Allard S (2011) The use of fresh-frozen plasma in England: high levels of inappropriate use in adults and children. Transfusion 51:62–70. doi:10.1111/j.1537-2995.2010.02798.x
Tempe DK, Virmani S (2002) Coagulation abnormalities in patients with cyanotic congenital heart disease. J Cardiothorac Vasc Anesth 16:752–765. doi:10.1053/jcan.2002.128436
Vlaar AP, Juffermans NP (2013) Transfusion-related acute lung injury: a clinical review. Lancet 382:984–994. doi:10.1016/S0140-6736(12)62197-7
Vogel AM, Radwan ZA, Cox CS Jr., Cotton BA (2013) Admission rapid thrombelastography delivers real-time “actionable” data in pediatric trauma. J Pediatr Surg 48:1371–1376. doi:10.1016/j.jpedsurg.2013.03.036
Westbury SK, Lee K, Reilly-Stitt C, Tulloh R, Mumford AD (2013) High haematocrit in cyanotic congenital heart disease affects how fibrinogen activity is determined by rotational thromboelastometry. Thromb Res 132:e145–e151. doi:10.1016/j.thromres.2013.07.006
Yang L, Stanworth S, Hopewell S, Doree C, Murphy M (2012) Is fresh-frozen plasma clinically effective? An update of a systematic review of randomized controlled trials. Transfusion 52:1673–1686. doi:10.1111/j.1537-2995.2011.03515.x, quiz 1673
Ethical statement
The present study protocol was approved by the Ethics Committee of Fuwai Hospital, the Chinese Academy of Medical Sciences, and the Peking Union Medical College, and related informed written consent was obtained from the parents or guardians of each patient.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Jaan Toelen
Rights and permissions
About this article
Cite this article
Miao, X., Liu, J., Zhao, M. et al. The influence of cardiopulmonary bypass priming without FFP on postoperative coagulation and recovery in pediatric patients with cyanotic congenital heart disease. Eur J Pediatr 173, 1437–1443 (2014). https://doi.org/10.1007/s00431-014-2335-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-014-2335-1