Abstract
Objective
Several strategies are employed for administering fresh frozen plasma (FFP) during weaning from cardiopulmonary bypass (CPB). This study evaluated by coagulation function aimed to compare two strategies of administering FFP in cardiovascular surgery: administering 4 units of FFP before separating from CPB or administering it after weaning from CPB.
Methods
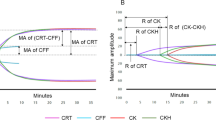
Thirty patients who underwent CPB and were expected to receive 8 units of FFP and 20 units of platelet concentrate were randomly allocated into group A (8 units of FFP and 20 units of platelet concentrate administered after separating from CPB) and group B (4 units of FFP administered before separation, and 4 units of FFP and 20 units of platelet concentrate administered after separating from CPB). Thromboelastography (TEG6s®, HAEMONETICS Japan GK, Tokyo, Japan) was conducted at four time points before and after separation. Blood test results, blood loss, and required amounts of blood transfusion were compared. The primary outcome was the difference in coagulation function evaluated by TEG6s 90 min after protamine administration.
Results
Twenty-eight patients were enrolled in the study. Coagulation function after separating from CPB was not significantly different between the groups. Additionally, no significant differences were found in intensive care unit outcomes, such as 24-h transfusion requirements.
Conclusions
Coagulation function 90 min after separating from CPB was not significantly different between the groups. Prior FFP administration before separation did not provide significant improvement in coagulation function.




Similar content being viewed by others
References
Guan XL, Wang XL, Liu YY, Lan F, Gong M, Li HY, Liu O, Jiang WJ, Liu YM, Zhu JM, Sun LZ, Zhang HJ. Changes in the hemostatic system of patients with acute aortic dissection undergoing aortic arch surgery. Ann Thorac Surg. 2016;101:945–51.
Westaby S. Anti-fibrinolytic therapy in thoracic aortic surgery. Ann Thorac Surg. 1999;67:1983–5 (discussion 1997–8).
Nomura F, Tamura K, Yoshitatsu M, Katayama A, Katayama K, Ihara K. Changes in coagulation condition, cytokine, adhesion molecule after repair of type A aortic dissection. Eur J Cardiothorac Surg. 2004;26:348–50.
Colson PH, Gaudard P, Fellahi JL, Bertet H, Faucanie M, Amour J, et al. Active bleeding after cardiac surgery: a prospective observational multicenter study. PLoS ONE. 2016;11:e0162396.
Nakayama Y, Nakajima Y, Tanaka KA, Sessler DI, Maeda S, Iida J, et al. Thromboelastometry-guided intraoperative haemostatic management reduces bleeding and red cell transfusion after paediatric cardiac surgery. Br J Anaesth. 2015;114:91–102.
Weber CF, Gorlinger K, Meininger D, Herrmann E, Bingold T, Moritz A, et al. Point-of-care testing: a prospective, randomized clinical trial of efficacy in coagulopathic cardiac surgery patients. Anesthesiology. 2012;117:531–47.
TEG6s, Haemonetics Inc. https://teg.haemonetics.com/en-gb/teg-6s-hemostasis-analyzer. Accessed 16 Mar 2020.
Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat. 2005;4:287–91.
Tamura T. Predicting results of fibrinogen and platelet levels by TEG6s during cardiopulmonary bypass: a pilot study. J Clin Anesth. 2019;58:59–60.
Tamura T, Imaizumi T, Kubo Y, Waters JH, Nishiwaki K. Prompt prediction of fibrinogen concentration during cardiopulmonary bypass: a pilot study. Nagoya J Med Sci. 2020;82. (in press).
Tamura T, Waters JH, Nishiwaki K. Heparin concentration in cell salvage during heparinization: a pilot study. Nagoya J Med Sci. 2020;82. (in press).
Westbrook AJ, Olsen J, Bailey M, Bates J, Scully M, Salamonsen RF. Protocol based on thromboelastograph (TEG) out-performs physician preference using laboratory coagulation tests to guide blood replacement during and after cardiac surgery: a pilot study. Heart Lung Circ. 2009;18:277–88.
Girdauskas E, Kempfert J, Kuntze T, Borger MA, Enders J, Fassl J, et al. Thromboelastometrically guided transfusion protocol during aortic surgery with circulatory arrest: a prospective, randomized trial. J Thorac Cardiovasc Surg. 2010;140(1117–24):e2.
Kozek-Langenecker SA, Ahmed AB, Afshari A, Albaladejo P, Aldecoa C, Barauskas G, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology: First update 2016. Eur J Anaesthesiol. 2017;34:332–95.
American Society of Anesthesiologists Task Force on Perioperative Blood Management. Practice guidelines for perioperative blood management: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management. Anesthesiology. 2015;122:241–75.
Karkouti K, Callum J, Crowther MA, McCluskey SA, Pendergrast J, Tait G, et al. The relationship between fibrinogen levels after cardiopulmonary bypass and large volume red cell transfusion in cardiac surgery: an observational study. Anesth Analg. 2013;117:14–22.
Maeda T, Miyata S, Usui A, Nishiwaki K, Tanaka H, Okita Y, et al. Safety of fibrinogen concentrate and cryoprecipitate in cardiovascular surgery: multicenter database study. J Cardiothorac Vasc Anesth. 2019;33:321–7.
Hou X, Yang F, Liu R, Yang J, Zhao Y, Wan C, et al. Retrograde autologous priming of the cardiopulmonary bypass circuit reduces blood transfusion in small adults: a prospective, randomized trial. Eur J Anaesthesiol. 2009;26:1061–6.
Joosten A, Huynh T, Suehiro K, Canales C, Cannesson M, Rinehart J. Goal-directed fluid therapy with closed-loop assistance during moderate risk surgery using noninvasive cardiac output monitoring: a pilot study. Br J Anaesth. 2015;114:886–92.
Bianchi P, Cotza M, Beccaris C, Silvetti S, Isgrò G, Pomè G, et al. Surgical and Clinical Outcome REsearch (SCORE) group Early or late fresh frozen plasma administration in newborns and small infants undergoing cardiac surgery: the APPEAR randomized trial. Br J Anaesth. 2017;118:788–96.
Desborough M, Sandu R, Brunskill SJ, Doree C, Trivella M, Montedori A, et al. Fresh frozen plasma for cardiovascular surgery. Cochrane Database Syst Rev. 2015;Cd007614.
Acknowledgements
We thank all cardiovascular surgery and anesthesiology medical staff members and all extra-corporeal technology staff at Japanese Red Cross Nagoya Daiichi Hospital.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JHW is a member of the advisory committee for Haemonetics, Inc. Other authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tamura, T., Yokota, S., Ito, T. et al. Coagulation ability when separating from cardiopulmonary bypass with and without fresh frozen plasma: a pilot study. Gen Thorac Cardiovasc Surg 68, 1361–1368 (2020). https://doi.org/10.1007/s11748-020-01372-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-020-01372-9