Abstract
In excess of 1 million young children die every year as a consequence of disease caused by Streptococcus pneumoniae, the vast majority in developing countries. Although the first vaccine against the Pneumococcus was produced before the First World War, licensure of the first vaccine with documented efficacy against severe infections in infants and young children did not occur until February 2000 in the United States. This conjugate vaccine consists of purified polysaccharide, from each of seven pneumococcal serotypes, chemically linked to a carrier protein. A high degree of efficacy of the new vaccine against potentially life-threatening infections has been shown in both poor and affluent countries. The vaccine’s potential to protect from acute otitis media, however, is very limited, although encouraging indirect effects, such as reduced antibiotic prescriptions, have been reported. An inherent problem with the new pneumococcal conjugate vaccines is that, while more than 20 pneumococcal serotypes may cause invasive disease, only a more limited number of polysaccharides, 11 or so, can in practice be conjugated to carrier protein as part of a single vaccine formulation. Because of variation in the ranking of serotypes most commonly responsible for pneumococcal disease, by region, age and disease manifestation, compromise was required in selecting serotype-specific saccharides for inclusion. Conclusion: Complex conjugate technology comes at a price, and the present costs keep most of the world’s children far out of reach of an effective vaccine. However, the pneumococcal conjugate vaccine is a highly functional weapon against deadly pneumococcal infections, and strenuous efforts are needed to maximise its accessibility to children most at risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than 1 million infants and children perish each year as a consequence of pneumococcal infection, almost all in ‘countries of the south’ [67]. Recent licensure of a vaccine against Streptococccus pneumoniae infections in the United States (Prevenar (PCV7) a heptavalent pneumococcal conjugate vaccine where saccharides of serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F are individually covalently linked to a carrier consisting of a non-toxic mutant variant of diphtheria toxin CRM197) has raised considerable hope among physicians and the general public [4]. Have we finally got a potent weapon against severe pneumococcal diseases - pneumonia, meningitis, and septicaemia? Can it also reduce the burden of acute otitis media (AOM)?
Results of critical initial efficacy trials with PCV7 are now published and the clarity of the whole picture is fast gaining resolution. The answers we have learnt differ by disease manifestation. From industrialised countries there is clear evidence that deadly invasive pneumococcal diseases can, on the whole, be prevented, but for otitis media, the evidence is much less encouraging. The critical question is, however, what can vulnerable children of the world gain from this new vaccine?
Background to vaccine development
In 1881 Louis Pasteur was among the first to isolate the gram-positive encapsulated bacterium, Streptococcus pneumoniae [46]. By 1911, whole-cell pneumococcal vaccines were being tested in South African gold miners [65]. Some benefit was reported, but the page turned once more when the crucial role of type-specific capsular polysaccharides in the immunology of invasive (bacteraemic) pneumococcal diseases began to be understood [24,27] and a vaccine based on purified polysaccharide was developed. Another early lesson was that the immunological response of infants and small children to pneumococcal polysaccharides was poor [19]. This property is the Achilles’ heel for all polysaccharide antigens. They induce a humoral (B-cell) response only in older children (aged >18 months). However, conjugation to a protein overcomes this problem [7].
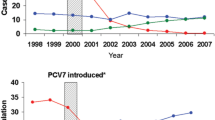
Vaccines for humans consisting of capsular polysaccharide (unconjugated) were produced before the Second World War. However, an intrinsic problem with the pneumococcus then (and now) was that there are 90 different serotypes with dissimilar capsular polysaccharides, and most may cause disease. Although, not all serotypes are equally prevalent [6,26], the most common pneumococci are, unfortunately, not the same throughout the world (Fig. 1) [6, 13, 14, 26, 32, 34, 42, 44, 63] and not in all disease manifestations and age groups [21, 22,67]. All this has posed a major challenge to vaccine developers. In the United States, types 4, 6B, 9V, 14, 18C, 19F, and 23F (which PCV7 covers) account for 86% of invasive diseases, but only 65% of pneumococcal acute otitis [26]. Worldwide these seven serotypes cover only about 50% of invasive cases.
Clinical protection against pneumonia was demonstrated in military recruits in the 1940s [40]. The polysaccharide vaccine produced antibodies that were shown to persist at least for 5–8 years [28]. Following World War 2, tetravalent, and soon hexavalent, vaccines were licensed in the United States. However, the licenses to manufacture were later allowed to lapse because the revolutionary new sulphonamides and (later) penicillin were thought to solve the problem with pneumococcal infections [5]. That this was wrong eventually became apparent—patients continued to contract and die from serious pneumococcal infections, so a reappraisal of polysaccharide vaccines was in order.
The number of serotypes incorporated in vaccines was increased gradually to the current 23 while the amount of each polysaccharide was reduced to 25 µg instead of the earlier 50 µg. There is no known limit for the number of polysaccharides one can add to a vaccine, but this amount was considered a compromise between epidemiology, need, and costs. Interestingly enough, the overall efficacy for prevention of severe infections in patients older than 5 years increased only from 53% (95% CI 38%–64%) to 60% (95% CI 30%–77%), when the 14-valent and the 23-valent vaccines were compared [12].
Immunogenicity, which has proven difficult to measure adequately [37,43], is not the same for each polysaccharide, but 80% of adult vaccinees in one study showed at least a two-fold rise in specific antibody concentration to each vaccine component [43]. Type 6A especially is a poor immunogen, whereas types 3 and 18C elicit fairly good antibody production even in infants [36]. Poor immunogenicity, especially in infants and young children, remained the main obstacle, and polysaccharides have never been used to a significant extent in infants.
Effectiveness of polysaccharide vaccine
Table 1 outlines known data on the effectiveness of polysaccharides in children. Direct comparison of results is difficult because the quality of data collection and the follow-up periods have varied, but one can conclude that the vaccine effectiveness is 40%–60% against severe infections in children older than about 2 years. No data exist on infants, which is lamentable since the incidence of pneumococcal meningitis is then at its highest. One may expect low effectiveness because of the poor immunogenicity of polysaccharides in infancy [40,67]. AOM is poorly prevented, the efficacy varying from 0% to around 60%, depending on whether all AOM, or AOM caused only by vaccine strains is considered [20, 29, 41,54]. Furthermore, polysaccharides have only a modest, if any, effect on nasopharyngeal carriage [36].
Despite several shortcomings, polysaccharides have, however, one indisputable advantage; they are rather inexpensive vaccines, thanks partly to the less complex manufacturing process. Since economic constraints pose a fundamental issue in less privileged countries [59], expanded use of these vaccines in developing countries remains promising and worthy of further research [56]. Polysaccharide vaccine continues to be recommended in the United States [2] and elsewhere for children 2 years of age and older who have medical conditions placing them at increased risk of invasive pneumococcal disease (e.g. sickle cell disease, HIV infection). Importantly, polysaccharide vaccine can be used successfully in conjunction with conjugate vaccines to expand serotype coverage [8] or as a booster [14]. The vaccine is well tolerated, including in young children [20,29].
Conjugate vaccines
The conjugation technique by which T-cell independent antigen (polysaccharide) is made T-cell dependent through covalent linkage of polysaccharide with a carrier protein (several types can be used) has been successfully applied to the pneumococcus. The spectacular success of Haemophilus influenzae type b (Hib) conjugates in many countries [47] gave reason to believe that pneumococcal disease, too, could be prevented by vaccines manufactured using this ‘new’ (rediscovered) technique. As was predicted from the experience with Hib conjugates [30], pneumococcal conjugates are potent immunogens in infants [1,58]. However, the practical limitation is that only a limited number of polysaccharides may be conjugated to a carrier. The largest clinical trials so far have used a 7- or 9-valent vaccine, and an 11-valent conjugate is about the maximum currently feasible. Hence, a conjugate vaccine needs to be better tailored to the local requirements (in terms of the serotypes covered) than the 23-valent polysaccharide vaccine.
This requirement causes problems. In Israel, 65% of paediatric infections are caused by six types (4, 8, 17, 9, 10, and 26) [16], and 35% of cases are due only to types 1 and 5 - both rare in Western Europe and North America. In Finland [22], the five most common serotypes in childhood meningitis are types 6, 19, 7, 9, and 4, pneumonia is mainly caused by types 7, 19, 14, 6, and bacteraemia by types 14, 6, 19, 18, and 9. In Pakistan [42], 70% of paediatric acute lower respiratory tract infections are attributable to only four types (9A, 16, 19A, and 19F). An appropriately tailored tetravalent vaccine (including types 1, 5, 6, and 14) for Kenya [55] would cover 52% of their severe pneumococcal infections. A list of the optimum vaccines for each region, disease manifestation, and age group could be endless, and all expectations cannot be met; compromise is needed.
Such a compromise is the heptavalent vaccine, PCV7 or Prevenar (Wyeth Laboratories, Pearl River, NY, USA), the first conjugate on the market, that was approved by the USA Food and Drug Administration in 2000. It uses a non-toxic protein CRM197 of mutant Corynebacterium diphtheriae as carrier. This vaccine is composed of polysaccharides 4, 6B, 9V, 14, 19F, and 23, and of oligosaccharide type 18C, a constellation which fits fairly well the disease profile in North American children. The amount of each antigen is 2 µg, except type 6B, for which it is 4 µg. In addition, there is 20 µg of CRM197 carrier protein, and 0.125 mg of aluminium phosphate as adjuvant. The vaccine is a liquid preparation (white suspension after shaking), and a dose is 0.5 ml, which is to be injected intramuscularly.
The Committee on Infectious Diseases of the American Academy of Pediatrics recommends pneumococcal conjugate for universal use in children aged 23 months and younger [3]. For infants, four vaccine doses should be given, the first three at the age of 2, 4, and 6 months, with a booster at the age of 12–15 months. For those 7 to 12 months of age, two doses are recommended, followed by a third dose after the 1st birthday. After this age, only two doses are deemed sufficient. The doses should be separated by an interval of 6 to 8 weeks. For children aged 24 to 59 months who are at high risk, two doses are recommended, and for these subgroups, the 23-valent polysaccharide vaccine should also be administered (to expand coverage).
PCV7’s coverage has already been added to, by the inclusion of serotypes 1 and 5, making a nonavalent conjugate; an 11-valent vaccine (serotypes 3 and 7 added) is also being tested. Serotypes 1, 3, 4, 5, 6B, 7F, 9V, 14, 18C, 19F, and 23F would cover approximately 75% of pneumococcal disease worldwide [43]. PCV7 covers only about 50% of clinically important pneumococcal disease worldwide.
Safety
Being highly purified products, pneumococcal conjugates are well tolerated [1,58], the post-vaccination symptoms and signs differing little from those seen following Hib conjugate vaccine. In a randomised, double-blind controlled study conducted at 23 sites within the Northern California Kaiser Permanente Health Maintenance Organisation, four doses of heptavalent vaccine were administered at the age of 2, 4, 6, and 12 to 15 months [9,57]. Both the pneumococcal and control vaccine (a serogroup C meningococcus conjugate vaccine) used the same CRM197 carrier protein. Local swelling and redness, and fever were more common ( P <0.05) in pneumococcal than meningococcal C conjugate vaccinees but no significant difference was observed in more severe reactions [58]. However, fever exceeding 38°C developed more often with PCV7. Long-term safety data, particularly in relation to rare events, is awaited.
Efficacy
Invasive disease
The first field trials have understandably focused on the main manifestations of invasive pneumococcal disease (e.g. meningitis, bacteraemia, septicaemia). The current data are derived from the United States [9,57], Finland [14,23] Israel [15,17] and South Africa [33,35]; a summary of the results is presented in Table 2.
The primary endpoint of the Californian trial was invasive disease defined as a positive culture for S. pneumoniae from a normally sterile body fluid. Secondary endpoints included protection from otitis media and pneumonia. Almost 40,000 children were enrolled. By the time 40 cases of invasive pneumococcal disease had developed, 39 were in the control group. This resulted in an efficacy of 97.4% ( P <0.001; 95% CI 82.7%–99.9%) against disease caused by vaccine serotypes. In the intent-to-treat analysis the respective numbers of cases were 49 versus 3, the protection thus being 93.9% ( P <0.001; 95% CI 79.6% to 98.5%). Disease due to non-vaccine serotypes was found in six children in the study group and three in the control group. Clearly the vaccine was highly efficacious against invasive disease, and the study was interrupted for ethical reasons.
The only vaccine failure was caused by type 19F, the one serotype that may require a higher concentration of circulating antibody than other types [9]. Otherwise, a serum concentration between 0.15 µg/ml and 0.5 µg/ml seemed to predict long-term protection, and this concentration for all vaccine types was reached by 90% of vaccinees. For pneumonia, the results were not as impressive, partly because of difficulties in defining pneumonia. An elegant way to present the results was classifying “pneumonia” in four ways: pneumonia as justified by the (junior) doctor on call, pneumonia with X-ray evidence as interpreted by a non-radiologist, pneumonia with the radiograph interpreted by a radiologist, and pneumonia with at least a 2.5 cm (1 inch) alveolar consolidation on the X-ray film. With this categorisation, the efficacy of heptavalent conjugate in California was 11%, 12%, 35%, and 63%, respectively. Evidently, the more likely the pneumonia was aetiologically pneumococcal, the better the vaccine efficacy [9]. However, when the Californian data were analysed a further year after unblinding, when the oldest children were 3.5 years of age, the efficacy appeared to fall after 2 years of age, although the difference is not significant [10].
The recently reported South African study [33,35] of a 9-valent conjugate vaccine showed 83% efficacy (95% CI 39%–97%) in HIV-negative children for prevention of a first episode of invasive pneumococcal disease caused by a vaccine serotype, while it was 65% (95% CI 24%–86%) in HIV-positive children. In children without HIV, there was a 20% (95%CI 2%–35%) reduction in the incidence of first episodes of radiologically confirmed alveolar consolidation. There was also evidence of a 66% reduction in invasive pneumococcal disease caused by penicillin-resistant strains.
Acute otitis media
AOM is overwhelmingly the most common pneumococcal infection with 7 million cases per year in the United States. However, the conjugate vaccines have not fulfilled the expectations of many. In a Finnish study, AOM (confirmed by myringotomy and culture) was the primary endpoint of a randomised, double-blind controlled trial comprising almost 1,700 infants [23,31]. Four doses of a pneumococcal conjugate vaccine (PCV7 or Pn OMPC, a heptavalent conjugate covering the same seven serotypes as PCV 7 but using an outer membrane protein of meningococcus for conjugation) or hepatitis B vaccine were administered at ages 2, 4, 6, and 12 months. When the efficacy of PCV7 was assessed at age 2 years, the overall incidence of AOM (Table 2) was reduced only by 6% (95% CI included zero), culture-proven pneumococcal otitis by 34%, and vaccine-specific AOM by 57%. Pn OMPC reduced AOM due to vaccine serotypes by 56% but the overall rate of AOM was not different in intervention and control groups [31].
In contrast, the study using Prevenar in California [9,57] did not investigate bacteriologically proven AOM, but interesting findings were still observed (Table 2). The incidence of AOM (defined clinically and without myringotomy), declined by 6% - exactly as it did in Finland -, but doctor visits for AOM, frequent AOM, and the need for ventilatory tube placement were reduced by 8%, 9%, and 25%, respectively [57]. In terms of spontaneously draining ears, the serotype-specific effectiveness was 53%, similar to Finland. The Israeli data support this experience (Table 2); a nonavalent conjugate prevented 17% of AOM [15,17].
A recent study from the Netherlands casts further light on the impact in older otitis-prone children. Children aged between 1 and 7 years with a history of at least two episodes of AOM in the previous year were randomised to PCV7 followed 6 months later by a 23-valent pneumococcal polysaccharide vaccine, or to sequential hepatitis vaccines. They were followed for 18 months. No reduction in the overall rate of AOM was observed, although nasopharyngeal carriage of vaccine serotype strains was less frequently observed in recipients of pneumococcal vaccines and there was a compensatory increase in carriage of non-vaccine serotypes [62]. There was a difference in the numbers of episodes of AOM in the 6 months after children were given either conjugate pneumococcal or hepatitis vaccine but before boosting with polysaccharide pneumococcal (or hepatitis) vaccine (170 versus 195 respectively) compared with the numbers after boosting (275 in the polysaccharide pneumococcal vaccine group versus 200 in the control group, P =0.0001). This suggests initial benefit from use of PCV7 that is lost after receipt of polysaccharide pneumococcal vaccine. It is plausible that the boosted protection against PCV7 serotypes increased the likelihood of acquiring colonisation and mucosal disease due to other bacteria [50].
Combining all efficacy data accumulated on AOM so far, conjugate vaccines seem surprisingly not to differ much from polysaccharides (Table 1), except in the youngest age groups (those most prone to otitis). Direct effects are modest, and prevention of otitis on its own is not an indication for this vaccine [2,3]. On the other hand, AOM is so common that even a tiny clinical reduction in the disease episodes would potentially have impressive overall impact.
Nasopharyngeal carriage and herd immunity
Indirect effects of vaccination have been observed, especially in Israel, Finland and the United States. Like previously with Hib conjugate vaccines [47,60], pneumococcal conjugates reduce nasopharyngeal carriage. This is particularly the case for colonisation with anti-microbial-resistant pneumococci [18]. A herd immunity effect is likely, e.g. vaccination of day-care centre attendees has been shown to reduce carriage of pathogenic pneumococci by younger siblings [25]. With less transmission, one can infer a lower risk of invasive disease. There is evidence from the United States that use of PCV7 in children may be preventing disease in adults, especially those of an age likely to have young children [64] Of concern, however, is (the observation [45] now confirmed [23]) that conjugate vaccine may lead to replacement of the vaccine serotypes by other serotypes. So far it is unclear if this potential change in nasopharyngeal flora has clinical consequences.
Given, however, that one conjugate (Pn OMPC) produced no overall decline in the incidence of AOM, there is concern that the overall efficacy against blood-culture negative pneumonia (another “mucosal” form of disease) may decline over time. No significant increase in invasive disease due to non-vaccine serotypes has been observed to date among children in the Californian study, but, worryingly, the herd benefit in US adults does not include HIV-positive women in whom the rate of invasive pneumococcal disease is static, a fall in vaccine-serotype disease being equalled by a rise in non-vaccine serotype disease (“Invasive pneumococcal disease in HIV-AIDS: Has introduction of 7-valent pneumococcal conjugate vaccine reduced HIV-related disease burden in the US?” Schuchat A, Flannery B, Heffernan R et al. 4th International Symposium on Pneumococcal Diseases, Helsinki, May 9–13, 2004). Also relevant is the finding that reduced carriage may decrease the use of antimicrobials in children. In Israel [17], the reduction was 53% or 20% depending on whether acute lower respiratory infections or AOM, respectively, were looked at. The experience in California is similarly encouraging and coincides with this observation.
The cost issue
The current information strongly favours the view that vaccine serotype-specific serious infections can be prevented with pneumococcal conjugates, even in infants, the major risk group. However, meningitis and other life-threatening manifestations are rare in industrialised countries, in contrast with developing countries where the burden is large [49, 56,59]. For this reason, pneumococcal conjugates have an enormous potential, especially in the less privileged world. Sadly even Hib conjugates, for which abundant data demonstrate their efficacy, are not much used there [3] - because of their high cost. The cruel reality of cost applies also to pneumococcal conjugates, but to an even greater extent. The current United States list price is $57 per dose, or $228 for all four doses. “Any medical cost savings that are associated with the vaccine are unlikely to be high enough to offset the cost of the vaccine at its current price” [51]. Even in the United States, a full course costs more than the other paediatric vaccines combined [39]. Such pricing is entirely unrealistic in most countries of the world. The decision in Australia to implement PCV7 first in the aboriginal population (who are at high risk through deprivation) is laudable [61].
A cost-effectiveness projection done in the United States suggests that the impact of PCV7 on otitis media accounts for 60% of the cost-savings expected by a programme of vaccination against pneumococcal disease [39]. This saving may be lost if the results shown with Pn OMPC in Finland are borne out in practice. The more certain benefit is in prevention of invasive disease. Interestingly, in Germany, the 7-valent vaccine would probably prevent no more than 52% of invasive cases in children [38]. The planned 9- and 11-valent vaccines would perhaps increase the effectiveness to 62% and 71%, respectively.
Conclusion
Pneumococcal conjugates have opened a new (but expensive) path to the prevention of serious childhood infections. Although the routine vaccination schedule is becoming more congested [48], it is likely that this conjugate vaccine will be implemented in affluent countries (as in the United States). This inclusion will be facilitated by the development of combination vaccines, e.g. with meningococcus C conjugate. However, those who really need the vaccine are again likely to be the last to receive it.
Abbreviations
- AOM :
-
acute otitis media
- PCV7 :
-
Prevenar, a heptavalent pneumococcal conjugate vaccine where saccharides of serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F are individually covalently linked to a carrier consisting of a non-toxic mutant variant of diphtheria toxin, CRM197
- Hib :
-
Haemophilus influenzae type b
References
Åhman H, Käyhty H, Tamminen P, Vuorela A, Malinoski F, Eskola J (1996) Pentavalent pneumococcal oligosaccharide conjugate vaccine PncCRM is well tolerated and able to induce an antibody response in infants. Pediatr Infect Dis 15: 134–139
American Academy of Pediatrics (2000) Red book: report of the Committee on Infectious Diseases. American Academy of Pediatrics, Elk Grove Village, pp 458–460
American Academy of Pediatrics Committee on Infectious Diseases (2000) Policy Statement: recommendations for the prevention of pneumococcal infections, including the use of pneumococcal conjugate vaccine (Prevnar), pneumococcal polysaccharide vaccine, and antibiotic prophylaxis. Pediatrics 106: 362–326
A pneumococcal conjugate vaccine for infants and children (2000) Med Lett Drugs Ther 42: 25–27
Austrian R (1975) Random gleanings from a life with the pneumococcus. J Infect Dis 131: 474–484
Austrian R, Douglas RM, Schiffman G et al (1976) Prevention of pneumococcal pneumonia by vaccination. Trans Assoc Am Physicians 89: 184–194
Avery OT, Goebel WF (1929) Chemo-immunological studies on conjugated carbohydrate-proteins. II Immunological specificity of synthetic sugar-protein antigens. J Exp Med 50: 533–550
Bell EA (2000) Prevnar: the new conjugate pneumococcal vaccine. Infect Dis Child 13: 27–29
Black S, Shinefiled H, Fireman B et al (2000) Efficacy, safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Pediatr Infect Dis 19: 187–195
Black SB, Shinefield H, Fireman B, et al (2002) Efficacy against pneumonia of heptavalent conjugate pneumococcal vaccine (Wyeth Lederle) in 37,868 infants and children: expanded data analysis including duration of protection (abstract). 3rd International Symposium on Pneumococci and Pneumococcal Diseases (ISPPD), Anchorage, AL, May 5th–8th
Bolan G, Broome CV, Facklam RR, Plikayti s BD, Fraser DW, Schlech WF III (1986) Pneumococcal vaccine efficacy in selected populations in the United States. Ann Intern Med 104: 1–6
Butler JC, Breiman RF, Campbell JF, Lipman HB, Broome CV, Facklam RR (1993) Pneumococcal polysaccharide vaccine efficacy. An evaluation of current recommendations. JAMA 270: 1826–1831
Capeding MR, Sombrro LT, Lucero MG, Saniel MC (1994) Serotype distribution and antimicrobial resistance of invasive Streptococcus pneumoniae isolates in Filipino children. J Infect Dis 169: 479–480
Chan CY, Molrine DC, George S et al (1996) Pneumococcal conjugate vaccine primes for antibody responses to polysaccharide pneumococcal vaccine after treatment of Hodgkins disease. J Infect Dis 173: 256–258
Dagan R, Fraser D (2000) Conjugate pneumococcal vaccine and antibiotic-resistant Streptococcus pneumoniae: herd immunity and reduction of otitis morbidity. Pediatr Infect Dis J 19: S79–S88
Dagan R, Englehard D, Piccard E and the Israeli Pediatric Bacteremia and Meningitis Group (1992) Epidemiology of invasive childhood pneumococcal infections in Israel. JAMA 268: 3328–3333
Dagan R, Sikuler-Cohen M, Givon-Lavi N et al (2000) A 9-valent pneumococcal CRM197 vaccine has a major impact on morbidity and antibiotic use in daycare centers. Pediatric Academic Societies and American Academy of Pediatrics Meeting, Boston, MA, May 2000
Dagan R, Givon-Lavi N, Porat N, Sikuler-Cohen M, Fraser D (2000) Immunisation of toddlers attending day care centers with a 9-valent conjugate pneumococcal vaccine (PncCRM9) reduces transmission of Streptococcus pneumoniae and antibiotic resistant S. pneumoniae to their young siblings (abstract). 40th Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC), Toronto, Sept 17th–20th
Davies JAV (1937) The response of infants to inoculation with type I pneumococcus carbohydrate. J Immunol 33: 1–7
Douglas RM, Miles HB (1984) Vaccination against Streptococcus pneumoniae in children: lack of demonstrable benefit in young Australian children. J Infect Dis 149: 861–869
Echániz-Aviles G, Velazquez-Meza ME, Carnalla-Barajas MN et al (1998) Predominance of the multi-resistant 23F international clone of Streptococcus pneumoniae among isolates from Mexico. Microb Drug Resist 4: 241–246
Eskola J, Takala AK, Kela E, Pekkanen E, Kalliokoski R, Leinonen M (1992) Epidemiology of invasive pneumococcal infections in children in Finland. JAMA 268: 3323–3327
Eskola J, Kilpi T, Palmu A (2001) Efficacy of a pneumococcal conjugate vaccine against acute otitis media in infants and children. N Engl J Med 344: 403–409
Francis T Jr, Tillett WS (1930) Cutaneous reactions in pneumonia: the development of antibodies following the intradermal injection of type-specific polysaccharide. J Exp Med 52: 573–585
Givon-Lavi N, Fraser D, Dagan R (2003) Vaccination of day-care center attendees reduces carriage of Streptococcus pneumoniae among their younger siblings. Pediatr Infect Dis J 22: 524–532
Hausdorff WP, Bryant J, Paradiso P, Siber G (2000) Which pneumococcal serogroups cause the most invasive disease: implications for conjugate vaccine formulation and use, part I. Clin Infect Dis 30: 100–121
Heidelberger M, Avery OT (1923) The soluble specific substance of pneumococcus. J Exp Med 38: 73–79
Heidelberger M, Dilapi MM, Siegel MYM (1950) Persistence of antibody in human subjects injected with pneumococcal polysaccharides. J Immunol 65: 535–541
Karma P, Pukander J, Sipilä M et al (1985) Prevention of otitis media in children by pneumococcal vaccination. Am J Otolaryngol 6: 173–184
Käyhty H, Peltola H, Eskola J, et al (1989) Immunogenicity of Haemophilus influenzae oligosaccharide-protein and polysaccharide-protein conjugate vaccination of children at 4, 6, and 14 months of age. Pediatrics 84: 995–999
Kilpi T, Ahman H, Jokinen J, Lankinen KS, Palmu A, Savolainen H, Gronholm M, Leinnonen M, Hovi T, Eskola J, Kayhty H, Bohidar N, Sadoff JC, Makela PH; Finnish Otitis Media Study Group (2003) Protective efficacy of a second pneumococcal conjugate vaccine against pneumococcal acute otitis media in infants and children: randomized, controlled trial of a 7-valent pneumococcal polysaccharide-meningococcal outer membrane protein complex conjugate vaccine in 1666 children. Clin Infect Dis 37:1155–1164
Klein O (1981) The epidemiology of pneumococcal disease in infants and children. Rev Infect Dis 3: 246–253
Klugman K (2002) Panel discussion: conjugate vaccine: efficacy against invasive disease and pneumonia and herd immunity. 3rd International Symposium on Pneumococci and Pneumococcal Diseases (ISPPD), Anchorage, AL, May 5th–8th
Klugman KP, Koornhof HJ (1988) Drug resistance pattern and serogroups or serotypes of pneumococcal isolates from cerebrospinal fluid or blood, 1979–1986. J Infect Dis 158: 956–964
Klugman KP, Madhi SA, Huebner RE et al (2003) A trial of a 9-valent pneumococcal conjugate vaccine in children with and those without HIV infection. N Engl J Med 349: 1341–1348
Koskela M (1986) Antibody response of young children to parenteral vaccination with pneumococcal capsular polysaccharides: a comparison between antibody levels in serum and middle ear effusion. Pediatr Infect Dis J 5: 431–434
Koskela M (1987) Serum antibodies to pneumococcal C-polysaccharide in children: response to acute pneumococcal otitis media or to vaccination. Pediatr Infect Dis J 6: 519–526
Kries R von, Siedler A, Schmitt HJ, Reinert RR (2000) Proportion of invasive pneumococcal infections in German children preventable by pneumococcal conjugate vaccines. Clin Infect Dis 31: 482–487
Lieu TA, Ray GT, Black SB et al (2000) Projected cost-effectiveness of pneumococcal conjugate vaccination of healthy infants and young children. JAMA 283: 1460–1468
MacLeod CM, Hodges RG, Heidelberger M, Bernhard WC (1945) Prevention of pneumococcal pneumonia by immunization with specific capsular polysaccharides J Exp Med 82: 445–465
Mäkelä PH, Sibakov M, Herva E et al (1980) Pneumococcal vaccine and otitis media. Lancet 2: 547–551
Mastro TD, Ghafoor A, Normani NK et al (1991) Antimicrobial resistance of pneumococci in children with acute lower respiratory tract infection in Pakistan. Lancet 337: 156–159
Musher DM, Luchi MJ, Watson DA, Hamilton R, Baughn RE (1990) Pneumococcal polysaccharide vaccine in young adults and older bronchitics: determination of IgG responses by ELISA and the effect of absorption of serum with non-type-specific cell wall polysaccharide. J Infect Dis 161: 728–735
Nielsen SV, Henrichsen J (1992) Capsular types of Streptococcus pneumoniae isolated from blood and CSF during 1982–1987. Clin Infect Dis 15: 794–798
Obaro S, Adegbola RA, Banya WA, Greenwood BM (1996) Carriage of pneumococcal after pneumococcal vaccination. Lancet 348: 272
Pasteur L (1881) Note sur la maladie nouvelle provoquée par la salive d’un enfant mort de la rage. Bull Acad Méd Paris 10: 944–1003
Peltola H (2000) Worldwide Haemophilus influenzae type b disease at the beginning of the 21st century: global analysis of the disease burden 25 years after the use of polysaccharide vaccine and a decade after the advent of conjugates. Clin Microbiol Rev 13: 302–317
Peltola H (2000) What would happen if we stopped vaccination? Lancet 356: s22
Peltola H (2001) Burden of meningitis and other severe bacterial infections of children in Africa: implications for prevention. Clin Infect Dis 31: 64–71
Peltola H, Schmitt J, Booy R (2003) Pneumococcal conjugate vaccine for acute otitis media–yes or no? Lancet 361: 2170–2171
Ray GT, Butler JC, Black SB, Shinefield HR, Fireman BH, Lieu TA (2002) Observed costs and health care use of children in a randomised controlled trial of pneumococcal conjugate vaccine. Pediatr Infect Dis J 21: 361–365
Riley ID, Everingham FA, Smith DE, Douglas RM (1981) Immunisation with a polyvalent pneumococcal vaccine: effect on respiratory mortality in children living in the New Guinea Highlands. Arch Dis Child 56: 354–357
Riley ID, Lehmann D, Alpers M P, Marshall DT de C, Gratten H, Smith D (1986) Pneumococcal vaccine prevents death from acute lower-respiratory-tract infections in Papua New Guinean children. Lancet 2: 877–881
Rosen C, Christensen P, Henrichsen J, Hovelius B, Prellner K (1984) Beneficial effect of pneumococcal vaccination on otitis media in children over two years old. Int J Pediatr Otorhinolaryngol 7: 239–246
Scott JAG, Hall AJ, Hannington A et al (1998) Serotype distribution and prevalence of resistance to benzylpenicillin in three representative populations of Streptococcus pneumoniae isolates from the coast of Kenya. Clin Infect Dis 27: 1442–1450
Shann F (1998) Pneumococcal vaccine: time for another controlled trial. Lancet 351: 1600–1601
Shinefield H (2000) Pneumococcal vaccine and ongoing lessons. Special symposium organized at the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy, (ICAAC), Toronto, Sept 17th
Shinefield HR, Black S, Ray P et al (1999) Safety and immunogenicity of heptavalent pneumococcal CRM197 conjugatevaccine in infants and toddlers. Pediatr Infect Dis 18: 757–763
Steinhoff MC (1993) Developing and deploying pneumococcal and haemophilus vaccines. Lancet 342: 630–631
Takala AK, Eskola J, Leinonen M et al (1991) Reduction of oropharyngeal carriage of Haemophilus influenzae type b (Hib) in children immunized with a Hib conjugate vaccine. J Infect Dis 164: 982–986
Trotman J, Hughes B, Mollison L (1995) Invasive pneumococcal disease in central Australia. Clin Infect Dis 20: 1553–1556
Veenhoven R, Bogaert D, Uiterwaal C et al (2003) Effect of conjugate pneumococcal vaccine followed by polysaccharide pneumococcal vaccine on recurrent acute otitis media: a randomised study. Lancet 36: 2189–2195
Verhaegen J, Glupczynski Y, Verbist L et al (1990) Capsular types and antibiotic sensitivity of pneumococci isolated from patients with serious infections in Belgium 1980 to 1988. Eur J Clin Microbiol Dis 9: 390–395
Whitney CG, Farley MM, Hadler J et al (2003) Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med 348: 1737–1746
Wright AE, Morgan W, Colbrook L, Dodgson RW (1914) Observations on prophylactic inoculation against pneumococcus infections, and on the results which have been achieved by it. Lancet I: 1–10, 87–95
Zangwill KM, Vadheim CM, Vannier AM, Hemenway LS, Greenberg DP, Ward JI (1996) Epidemiology of invasive pneumococcal disease in Southern California: implications for the design and conduct of a pneumococcal conjugate vaccine efficacy trial. J Infect Dis 174: 752–759
World Health Organisation (1999). Pneumococcal vaccines – WHO position paper. Wkly Epidemiol Rec 74: 177–184
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper is the product of a Summit of Independent European Vaccine Experts held in Tenerife, January 2003. The opinions expressed in this paper are independent of government and industry.
Rights and permissions
About this article
Cite this article
Peltola, H., Booy, R. & Schmitt, HJ. What can children gain from pneumococcal conjugate vaccines?. Eur J Pediatr 163, 509–516 (2004). https://doi.org/10.1007/s00431-004-1430-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-004-1430-0