Abstract
Escherichia coli O157:H7 with its traits such as intestinal colonization and fecal-oral route of transmission demands mucosal vaccine development. E. coli secreted protein B (EspB) is one of the key type III secretory system (TTSS) targets for mucosal candidate vaccine due to its indispensable role in the pathogenesis of E. coli O157:H7. However, mucosally administered recombinant proteins have low immunogenicity which could be overcome by the use of mucosal adjuvants. The quest for safe, potent mucosal adjuvant has recognized ΔG fragment of Zonula occludens toxin of Vibrio cholerae with such properties. ΔG enhances mucosal permeability via the paracellular route by altering epithelial tight junction structure in a reversible, ephemeral and non-toxic manner. Therefore, we tested whether recombinant ΔG intranasally co-administered with truncated EspB (EspB + ΔG) could serve as an effective mucosal adjuvant. Results showed that EspB + ΔG group induced higher systemic IgG and mucosal IgA than EspB alone. Moreover, EspB alone developed Th2 type response with IgG1/IgG2a ratio (1.64) and IL-4, IL-10 cytokines whereas that of EspB + ΔG group generated mixed Th1/Th2 type immune response evident from IgG1/IgG2a ratio (1.17) as well as IL-4, IL-10 and IFN-γ cytokine levels compared to control. Sera of EspB + ΔG group inhibited TTSS mediated haemolysis of murine RBCs more effectively compared to EspB, control group and sera of both EspB + ΔG, EspB group resulted in similar levels of efficacious reduction in E. coli O157:H7 adherence to Caco-2 cells compared to control. Moreover, vaccination with EspB + ΔG resulted in significant reduction in E. coli O157:H7 fecal shedding compared to EspB and control group in experimentally challenged streptomycin-treated mice. These results demonstrate mucosal adjuvanticity of ΔG co-administered with EspB in enhancing overall immunogenicity to reduce E. coli O157:H7 shedding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Escherichia coli O157:H7 is a common serotype of verocytotoxin-producing E. coli (VTEC) associated with the majority of human outbreaks and sporadic cases. E. coli O157:H7 infection is a grave public health concern due to its association with a fatal hemolytic uremic syndrome (HUS) in addition to diarrhoea, haemorrhagic colitis. Human infections are mainly acquired by contamination of food, water via direct or indirect contact with ruminant feces [1]. Therefore, vaccination of ruminants to limit colonization and shedding of E. coli O157:H7 are gaining significant attention. Recent studies on Type III secretory system protein-based vaccine have confirmed its positive effect in reducing fecal shedding in ruminants [2] and preventing human infection [3]. However, there are paradoxical views regarding the necessity of the mucosal immune response to confer protection against E. coli O157:H7. Some vaccine studies have reported it to be dispensable [4, 5] whereas other studies have shown enhanced protection in reducing fecal shedding in the presence of mucosal immune response [6, 7]. The latter results coincide with the report of induction of strong mucosal IgA response against Type III proteins following infection at the bovine terminal mucosa, which is the primary site of colonization for E. coli O157:H7 [8]. Despite its importance, studies attempting to achieve mucosal immunity with recombinant proteins are relatively scarce. Therefore, further studies on mucosal vaccine strategies employing recombinant proteins could progress the development of a potent vaccine against E. coli O157:H7.
Mucosal immunization is preferred to elicit mucosal immunity because parenteral immunization typically elicits poor mucosal immunity. But the poor immunogenicity of recombinant proteins applied to mucosal surfaces necessitates the use of mucosal adjuvants. However, the lack of safe and potent mucosal adjuvant with a precisely known mechanism of action seems to dampen the research on recombinant mucosal vaccine development. In this regard, Fasano et al. have identified a 45 kDa protein from Vibrio cholerae named Zonula occludens toxin (Zot), which is able to open epithelial tight junction in a reversible, non-toxic manner to increase paracellular transport of macromolecules [9,10,11]. Subsequently, its potential in mucosal antigen delivery via different routes [12] suggested it to be a promising candidate mucosal adjuvant. Further study has discerned a 12 kDa ΔG fragment of Zot capable of transiently increasing mucosal permeability [13]. This ΔG fragment has found its immense utility in the field of drug delivery [14], with no further research on its efficacy as a mucosal adjuvant. Another complication to achieve mucosal immunity using recombinant proteins arises in terms of immunization route. Recombinant proteins administered via oral route undergoes detrimental conditions like low gastric pH, digestive enzymes and bile salts resulting in its deactivation and degradation unless a suitable delivery vehicle is employed. On the other hand, intranasal administration is an alternative route for recombinant protein delivery because of its properties like lack of acidity, the dearth of abundantly secreted enzymes and small mucosal surface area [15].
A rational approach for eliciting mucosal immunity against E. coli O157:H7 would be to target a key TTSS multifunctional protein involved in initial stages of attaching and effacing (A/E) lesion formation which is crucial for efficient intestinal colonization. It is well known that the type III protein EspB acts as both translocon protein and translocated effector during the pathogenesis of E. coli O157:H7 [16]. As a translocon protein, EspB along with EspD of Type III machinery causes pore formation in the epithelial cell forming a conduit for the delivery of translocated proteins [17]. In fact, EspB is required for the translocation of Tir into the host cell which is responsible for intimate adherence [18]. Moreover, subsequent to its secretion into the host cell, EspB also functions as a multifaceted effector by interacting with various host proteins [16] to execute key events in the pathogenesis. The versatile role of EspB in pathogenesis and its strong immunogenicity [19] make it one of the prime targets to be co-administered with ΔG for candidate mucosal subunit vaccine development against E. coli O157:H7. Therefore, in the present work, we characterized the potentiality of ΔG active fragment of Zot co-administered with EspB via the intranasal route to elicit effective immune responses and its ability to prevent colonization, shedding of E. coli O157:H7 in mice.
Materials and methods
Media, bacterial strains, plasmids, cell line and mice
All media and supplements for bacterial culture were procured from Himedia laboratories, India. All the media, reagents, and chemicals related to cell culture were purchased from Sigma-Aldrich (India). pRSET A, B expression vectors and DH5α, BL21 (DE3) pLysS host strains were procured from Novagen, USA. The host strains were grown on Luria Bertani (LB) broth/agar and were supplemented with appropriate antibiotics such as ampicillin, chloramphenicol for cloning and expression studies. E. coli O157:H7 USDA 303 was a kind gift from Dr. Indrani Karunasagar, College of Fisheries, Mangalore and Vibrio cholerae O139 was obtained from National Institute of Cholera and Enteric Disease (NICED). These strains were grown on LB broth or agar without antibiotics. Caco-2 cell line was supplied by National Centre for Cell Science, Pune, India. Female BALB/c mice were provided by Central Animal Facility, Defence Food Research Laboratory, Mysuru, India. Mice were allowed access to food and water ad libitum. All animal experiments in this study were performed as per the guidelines of Institutional Animal Ethical Committee, DFRL, Mysuru with the approval of Committee For The Purpose of Control and Supervision of Experiments on Animals (CPCSEA), India (code- IAEC-2016/15).
Cloning, expression and purification procedures
The primers used for amplifying ΔG, espb genes included ΔG-F (5′CGCGGATCCGTTTTGTATTGGTCGGCTT-3′); ΔG-R (5′ CCGCTCGAGAAATATACTATTTAGTCCTTTTTT-3′) and espb-F (5′-CCGCTCGAGGCTTTGGTTGGCGGGAT-3′); espb-R (5′ CCCAAGCTTCCCAGCTAAGCGACCCG-3′). After PCR amplification from their respective genomic DNA, amplicons with the incorporated restriction sites were digested with their appropriate restriction enzymes (Fermentas, India). Following digestion, the BamHI/XhoI digested ΔG amplicon, XhoI/HindIII digested espb amplicon was ligated into BamHI/XhoI site of pRSET B, XhoI/HindIII site of pRSET A vector resulting in pRSET B-ΔG and pRSET A-espb, respectively. pRSET B-ΔG, pRSET A-espb plasmids were first transformed into DH5α followed by confirmation of these recombinant plasmid containing clones using a T7 universal primer-based PCR as well as sequencing as described previously [20]. The extracted recombinant plasmids were transformed into BL21 (DE3) pLysS and positive colonies were selected on LB agar with ampicillin (100 µg/mL) and chloramphenicol (34 µg/mL). Then the BL21 (DE3) pLysS harbouring the constructed vectors were inoculated in LB broth supplemented with suitable antibiotics and grown until the optical density of the medium at 600 nm was approximately 0.6. Then recombinant protein production was induced with 0.5 mM isopropyl-β-D-thiogalactopyranoside (Sigma, India) with further incubation in a shaker incubator for 5 h at 37 °C. After IPTG induction, both induced, uninduced cells were lysed and the protein expression was analysed by 12% SDS–PAGE stained with Coomassie brilliant blue (Bio-Rad, India). Colonies with the optimal expression level of recombinant ΔG, EspB proteins were induced in 500 mL LB broth and these recombinant proteins were purified from inclusion bodies solubilized using the denaturing buffer containing 8M urea, 20 mM sodium phosphate and 500 mM sodium chloride. Purification was performed with Ni2+-NTA slurry (Qiagen, Hilden, Germany) according to the manufacturer’s protocol employing denaturing buffers of varying pH for binding (8.0), wash (6.3) and elution (5.4). During wash step, 50 column volume of PBS containing 0.1% Triton X-114 (Sigma, India) followed by 20 column volume of wash buffer without detergent at 4 °C was used to remove endotoxin from recombinant protein preparation as described previously [21]. Dialysis in decreasing gradient of urea (6M, 4M, 2M, 0.5M) followed by final dialysis in PBS (pH-7.4) at 4 °C was done to refold the purified recombinant proteins and their endotoxin levels were analysed by Limulus amebocyte lysate (LAL) assay based E-TOXATE Kit (Sigma, India). The expression, purity of recombinant His-tagged proteins was assessed by 12% SDS–PAGE stained with Coomassie brilliant blue (Bio-Rad, India). The expressed protein was authenticated by Western blotting using mouse monoclonal anti-histidine antibodies and polyclonal goat anti-mouse HRP conjugated secondary antibodies (Sigma, India) followed by development with Diaminobenzidene tetrahydrochloride (Sigma, India) along with 30% H2O2 in phosphate buffered saline.
Immunization schedule
Three groups of 9 female BALB/c mice aged 6 week (central animal facility, DFRL) were intranasally immunized with 30 µg of purified EspB (n = 9) or 30 µg of purified EspB co-administered with 10 µg of purified ΔG (n = 9) or sterile PBS as a control in overall 20 µL volume on day 0, 7, 21 and 35. Blood and fecal samples were collected one week after the final immunization. The serum samples were used for the estimation of antibody titer, IgG1, IgG2a and IgA isotypes and the fecal samples were used for determination of IgA levels.
ELISA for assessment of antigen specific antibody responses
EspB specific serum IgG response was analysed using indirect ELISA as described previously [22]. IgG1, IgG2a titers were assayed in serially diluted sera obtained 1 week after the 35th day of immunization from all immunized groups by mouse isotyping kit (Sigma, Bangalore, India) as per manufacturer’s instructions. IgG and IgA isotyping assay were done similar to the ELISA for total serum IgG estimation with the only difference in the use of goat anti-mouse isotype specific monoclonal antibodies (1:1000 diluted in PBS) and polyvalent rabbit anti-goat HRP conjugate (Sigma, India). The absorbance was analysed using ELISA reader (TECAN Infinite® M200 PRO, Switzerland). IgG and IgA titers were calculated based on endpoint dilution method as the last dilution of the sample having a mean O.D. two times greater than the naive sample. Fecal IgA extraction was done as described by [23].
Splenocyte proliferation assay and Cytokine ELISA
The spleen was aseptically removed from control and immunized mice (n = 3) on the 7th day after final booster. The splenocytes were homogenized by gently rupturing the spleen on a wire mesh using rubber plunger of the 5 mL syringe followed by flushing with sterile Dulbecco’s Modified Eagle’s medium (DMEM) into centrifuge tube on ice. Cells were centrifuged and were adjusted to 1 × 106 cells/mL in DMEM with 10% (v/v) fetal bovine serum (FBS), 50 U/mL penicillin, 50 µg/mL of streptomycin and 0.2% NaHCO3. Wells were seeded with 100 µL of 1 × 106 cells in 96 well tissue culture microtiter plate and were re-triggered with 10 µg/mL of EspB or 10 µg/mL of Concanavalin A (Con A, Sigma, India) for 72 h. After incubation, the cell culture supernatant was collected for cytokine estimation and the cells were processed for lymphocyte proliferation based on the MTT assay as described elsewhere [24]. The level of cytokines in lymphocyte culture supernatant was quantified by mouse cytokine ELISA kit (Mabtech, Nacka, Sweden) specific for IL-4, IL-10 and IFN-γ as per manufacturer’s instructions.
Haemolysis inhibition assay
The ability of immunized mice sera to inhibit EspB mediated haemolytic activity of E. coli strain was assessed as described by [25] with minor modifications. Briefly, EPEC ATCC 43887 was grown at 37 °C overnight without shaking followed by 1:100 dilution in DMEM without phenol red. Then, 2 mL of this suspension was mixed with pooled sera (complement inactivated at 56 °C for 30 min) from each group into 6 well plates and incubated for 1 h at 5% CO2 incubator. To this mixture, 2 mL of 5% RBC-DMEM solution was added followed by further incubation for 4 h at 37 °C (5% CO2) in 6 well plates. After incubation, the suspension was gently removed from the plates and cells were pelleted at 12,000×g for 1 min. The presence of released haemoglobin was calculated from the supernatants by measuring the OD at 543 nm (A543) in the plate reader (TECAN Infinite® M200 PRO, Switzerland). DH5α strain, which does not encode TTSS, was used as a negative control. Only EPEC ATCC 43887 with same incubation conditions except for the addition of sera served as a positive control. Haemolytic activity was presented as relative haemolysis percentage (percentage haemolysis caused by only EPEC ATCC 43887 with same incubation conditions—percentage haemolysis of each treatment). The experiment was performed thrice in triplicates for each group.
Assessment of antibody mediated inhibition of E. coli O157:H7 adherence to Caco-2 cells
The assay to determine the ability of anti-EspB antibodies to inhibit E. coli O157:H7 adherence was performed as described by [26] with minor modifications. In brief, Caco-2 cells were grown to confluence in Dulbecco’s Modified Eagle’s medium (DMEM) with 10% FBS, 50 units/mL penicillin, and 50 µg/mL streptomycin in 75 mL flask (Greiner). The cells were maintained at 37 °C in 5% CO2. Prior to the experiment, Caco-2 cells were seeded to each well of a 12-well tissue culture plate containing DMEM + 10% FBS without antibiotics and grown to a confluent monolayer with 7 × 105 cells per well. E. coli O157:H7 inoculum grown overnight on BHI agar at 37 °C was picked with a sterile inoculation loop and were gently re-suspended in sterile PBS. Hundred microliters of E. coli O157:H7 were incubated on a shaker set at 50 rpm for 1 h at room temperature with 20 µL serum of each immunization group including sham group. After incubation, these mixtures were made up to 300 µL volume with sterile PBS and were seeded to each well comprising Caco-2 cells in 700 µL cell culture media. After an additional incubation for 1 h at room temperature, cells were washed thrice with PBS to remove non-adherent bacteria followed by mechanical agitation using vigorous pipetting with PBS to dislodge cells with adherent bacteria. The plating of serial 10 fold dilutions of the suspension on the LB agar was done and CFU (colony forming unit) of adherent bacteria from each group was counted. Each experiment was repeated twice in triplicates.
E. coli O157:H7 challenge studies
Two weeks after the last immunization, six immunized mice per group were orally challenged with 100 µL of 1010E. coli O157:H7 suspension after their overnight fasting. Moreover, mice were given drinking water containing streptomycin sulphate (5 mg/mL) 1 day prior to challenge. The animals were accommodated individually and allowed to consume food and water ad libitum. The fecal samples from each mouse were collected at 2 days interval for the period of 2 weeks from the 14th day after last immunization and fecal shedding was investigated as described previously [27].
Statistical analysis
All statistical analyses were performed using GraphPad Prism 5.0 version. All the experiments were performed in triplicate unless otherwise stated. One way ANOVA with Tukey’s post hoc test was used to analyse antibody titer, antibody isotype titer, cytokine and haemolysis, adherence inhibition assay data. All their values were presented as mean value ± standard deviation (SD). Significance (P) value summary: ns; not significant, *P < 0.05, **P < 0.01, ***P < 0.001. One way repeated measures ANOVA with Bonferroni’s post-test was used to analyse the fecal shedding data among three different immunization groups. Fecal shedding data was presented as Log10 CFU of E. coli O157:H7 from individual mice in each immunized group.
Results
Cloning, expression and purification of recombinant ΔG, EspB
PCR amplified genes ΔG (333 bp) encoding amino acid region of 287–398 of zot, amino acid region of 98–312 of espb (643 bp) were directionally cloned in-frame into pRSET B and pRSET A plasmid, respectively (Fig. 1a). Recombinant clones harbouring these plasmids were confirmed by PCR using a T7 universal primer and proper reading frame of inserts was confirmed by sequencing. Recombinant plasmids pRSET B-ΔG, pRSET A-espb were then transformed into E. coli BL21 (DE3) pLysS for protein expression. The recombinant protein expression with predominant bands at 18 kDa for ΔG, 28 kDa for EspB was detected on the SDS–PAGE gel stained with Coomassie blue (Fig. 1b). The recombinant proteins purified using nickel affinity chromatography under denaturing conditions yielded a single protein band at 18 kDa for ΔG, 28 kDa for EspB, respectively (Fig. 1c). The endotoxin levels in the purified proteins were below 0.1 EU/mL (data not shown) which is the detection limit of Limulus amebocyte lysate (LAL) E-Toxate reaction kit (Sigma, India). Western blot with the anti-His antibodies displayed immunoreactivity to recombinant ΔG, EspB (Fig. 1d).
Cloning, expression and purification of recombinant proteins ΔG, EspB. a Agarose gel showing PCR amplification of ΔG, EspB. Lane L indicates 100 bp ladder, Lane 1; ΔG PCR product, Lane 2; EspB PCR product. Arrow marks indicate the size of the corresponding PCR products. b 12% SDS–PAGE stained with Coomassie brilliant blue displaying expression of recombinant proteins. Lane M; unstained protein marker, Lane 1; cell lysate of IPTG induced pRSET B-ΔG containing BL21(DE3) pLysS, Lane 2; un-induced BL21(DE3) pLysS cell lysate, Lane 3; IPTG induced pRSET A-espb containing BL21(DE3) pLysS cell lysate. Arrow marks indicate the size of the expressed recombinant proteins. c Coomassie brilliant blue stained 12% SDS–PAGE showing purification of expressed recombinant proteins. Lane M; unstained protein marker, Lane 1; purified EspB recombinant protein, Lane 2; purified ΔG recombinant protein. d Western blot using mouse anti-histidine monoclonal antibodies and polyclonal goat anti-mouse HRP conjugated secondary antibodies developed with Diaminobenzidine tetrahydrochloride along with 30% H2O2 to analyse expressed recombinant proteins. Lane M; pre-stained protein marker, Lane 1; purified ΔG recombinant protein, Lane 2; purified EspB recombinant protein. Arrow marks indicate immune-reactivity of purified ΔG, EspB at ~ 18 kDa and ~ 28 kDa, respectively
Intranasal co-administration of recombinant ΔG, EspB enhances EspB-specific IgG and IgA responses in serum and feces
In order to evaluate the potentiality of ΔG as a mucosal adjuvant, groups of mice were intranasally immunized with EspB or EspB + ΔG. 1 week after third booster dose, EspB-specific antibody responses were evaluated in serum and fecal samples. The log2 endpoint titer in sera of EspB + ΔG group peaked to 15.40 ± 0.49 (p < 0.001) as against sera of EspB group 13.29 ± 0.44 (p < 0.001) compared to control (Fig. 2a). Analysis of antibody isotype showed that the IgG1/IgG2a ratio of EspB group was 1.64 whereas that of EspB + ΔG group was 1.15 (Fig. 2b). This implies that co-administration of ΔG with EspB tend to skew the response to mixed Th1/Th2 type immune response. EspB intranasally co-administered with ΔG elicited significant EspB-specific IgA in both serum (Fig. 2c) and feces (Fig. 2d) (p < 0.001) whereas that of EspB alone elicited significant EspB-specific IgA only in serum (p < 0.001) but not in feces compared to control. Serum and fecal IgA levels of EspB + ΔG group were considerably high compared to EspB alone group (p < 0.001).
Analysis of anti-EspB antibodies induced by intranasal administration of recombinant proteins EspB and EspB + ΔG in serum and feces of immunized mice collected 1 week after the last booster (42 days). a EspB specific serum IgG titers determined by ELISA. b EspB specific antibody isotype analysis of IgG1, IgG2a and their ratios. c Anti-EspB-serum IgA titer elicited by EspB, EspB + ΔG immunized groups. d EspB specific fecal IgA titer was analysed in all the immunized groups. IgG and IgA titers were calculated based on endpoint dilution method as the last dilution of the sample having a mean O.D. two times greater than the naive sample. Data are representative of one of three independent experiments expressed as mean ± SD of all mice in each group and analysed using one way ANOVA with Tukey’s test (*p < 0.05, **p < 0.01, ***p < 0.001)
Cell mediated immune response and IL-4, IL-10 and IFN-γ production
Significant increase in proliferation index (P.I.) was observed in EspB + ΔG (3.842 ± 0.319) (p < 0.001) and EspB (2.752 ± 0.324) (p < 0.001) immunized mice splenocytes compared to control mice splenocytes (0.686 ± 0.303) after re-triggering with 10 µg/mL of EspB. Moreover, P.I. of EspB + ΔG group splenocytes was also significantly high compared to EspB group splenocytes (p < 0.05) (Fig. 3a). Furthermore, evaluation of cytokine levels revealed that EspB + ΔG immunized mice induced significantly high levels of IL-4 (367 pg/mL), IL-10 (309 pg/mL) whereas EspB immunized mice yielded 208 pg/mL, 235 pg/mL for IL-4 and IL-10, respectively (p < 0.001) compared to control group (Fig. 3b, c). However, IFN-γ levels enhanced significantly in EspB + ΔG group (290 pg/mL) (p < 0.001) while that of EspB (89 pg/mL) showed no significant increase compared to control (Fig. 3d).
Evaluation of potential of ΔG to enhance EspB-induced lymphocyte proliferation and EspB-specific cytokine production from in vitro cultured immunized mice splenocytes. a Splenocytes of control, EspB and EspB + ΔG were grown in vitro and re-induced with EspB (10 µg/mL) for 72 h and proliferation index was calculated based on MTT assay. Data are presented as mean proliferation index ± SD analysed by one way ANOVA with Tukey’s test. Cytokine sandwich ELISA to estimate the b IL-4, c IL-10 and d IFN-γ levels from the supernatant of immunized mice splenocytes removed at 72 h after stimulation with recombinant EspB. Data are representative of one of the three independent experiments done in triplicates. *p < 0.05, **p < 0.01, ***p < 0.001 represents significant difference as compared to sham group
Effect of antibody on haemolysis
The neutralizing capacity of immunized mice sera to inhibit haemolysis was assessed as a function of EPEC induced haemolysis in 5% mice RBC-DMEM suspension. The percentage of haemolysis was measured by determining absorbance (543 nm) of RBC supernatant incubated at 37 °C for 4 h which was previously incubated with EPEC for 1 h (with/without sera). The percentage was expressed relative to that of a control containing only EPEC without sera. The pooled sera from EspB + ΔG immunized group and EspB alone immunized group inhibited the lysis of erythrocytes by 77% and 61%, respectively (Fig. 4). The percentage inhibition of haemolysis was significantly high for EspB + ΔG (p < 0.001) as well as EspB (p < 0.001) compared to control. Moreover, the percentage inhibition of haemolysis was significantly high for EspB + ΔG compared to EspB group (p < 0.001).
Haemolysis inhibition assay. Anti-haemolytic property of antibodies in sera of EspB, EspB + ΔG and control group. Results were interpreted as % of haemolysis inhibition caused by sera of immunized groups relative to that of a control containing only EPEC without sera considered to be 100%. Data are represented as mean ± SD of three independent experiments (*p < 0.05, **p < 0.01, ***p < 0.001)
Effect of antibody on bacterial adherence to Caco-2 cells
Results of the percentage of adherent bacteria revealed that E. coli O157:H7 cells pre-treated with sera of EspB + ΔG, EspB showed significant inhibition of adherence to Caco-2 cells, respectively, compared to control group sera (p < 0.001). However, there was no considerable difference between adherence inhibition mediated by sera of EspB and EspB + ΔG group (Table 1).
Protection conferred by EspB, EspB + ΔG on E. coli O157:H7 challenge
After an oral challenge with 1010 CFU of E. coli O157:H7, fecal shedding was monitored in control and immunized mice for a period of 14 days. The fecal shedding of these bacteria in EspB + ΔG immunized mice steadily decreased and ceased completely after 10 days compared to EspB as well as control group (p < 0.001) which was shedding these bacteria even on the last day of the observation period (14 days). Moreover, EspB group shed low levels (2 log10 CFU) of E. coli O157:H7 on the last day of observation period but it was 4.5 log units lesser compared to control group which was shedding 6.5 log10 CFU (p < 0.01) (Fig. 5).
Fecal shedding assay for assessing protection conferred against E. coli O157:H7 post challenge. Sham group and thrice immunized mice groups (EspB, EspB + ΔG) were given 1 day streptomycin treatment and were fed with 100 µL of 1010E. coli O157:H7 2 weeks after last immunization. Data are represented in the form of grouped scatter plot as Log10 CFU of E. coli O157:H7 of 6 individual mice in each group. Significant differences among different immunization groups were analysed using one way repeated measures ANOVA using Bonferroni’s post-test assuming *p < 0.05, **p < 0.01, ***p < 0.001 significant levels
Discussion
The meta-data analysis of published literature on vaccines against E. coli O157:H7 have revealed that Type III protein-based vaccines significantly reduced its fecal shedding in ruminants [28]. Despite the central role of EspB among Type III proteins in E. coli O157:H7 colonization, very few vaccine studies targeting this molecule are reported [29,30,31]. In particular, mucosal vaccine strategies employing EspB are still scant. A recent study by Ahmed et al. [32] has used L. Lactis as a delivery vehicle for oral immunization of EspB. However, issues related to weak expression levels, inability to measure exact in vivo antigen dose [33] raises the concern of its varying efficacy as an oral vaccine delivery vehicle. On the other hand, recombinant proteins targeting TTSS have shown considerable success as a candidate vaccine against E. coli O157:H7. Moreover, the safety and efficacy of ΔG in terms of mucosal drug delivery [14] is well established, which could, in turn, be extended for mucosal antigen delivery. Considering these lacunas and possibilities, the present study characterized the efficacy of active fragment of Zot (ΔG) co-administered with EspB via the intranasal route to generate the mucosal immune response and its ability to reduce colonization, shedding of E. coli O157:H7 in mice.
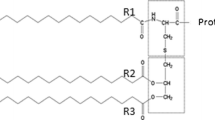
Recombinant ΔG, EspB was rationally constructed by selecting amino acid regions of these proteins involved in crucial functions. Recombinant truncated EspB contained amino acid region 98–312 of native EspB. The amino acid 99–118 of EspB is responsible for RBC haemolysis as well as actin accumulation below the bacterial attachment site, amino acid 118–190 is required for interaction with EspA and residues 217–312 is necessary for bacterial adherence [34]. In addition to this, the latest work on EspB from EPEC has shown that it selectively induce cell death in immune cells which could be an immune evasion strategy and the C-terminal 39 amino acid is probably responsible for this function [35]. However, it remains to be elucidated whether the EspB from E. coli O157:H7 possess this trait, as functional dissimilarity between one or more LEE-encoded effector proteins has been previously suggested between EPEC and EHEC [36]. In the case of recombinant ΔG, amino acid 287–398 of carboxyl-terminal region of Zot of Vibrio cholerae responsible for tight junction disassembly [13] was selected.
In our study, co-administration of ΔG with EspB resulted in robust systemic, mucosal and cellular immune responses. In terms of systemic immune response, IgG antibody titer was significantly high in mice intranasally immunized with EspB + ΔG compared to EspB alone. Antibody isotyping data showed high titers of both IgG1, IgG2a antibody isotype in EspB + ΔG group signifying probable mixed Th1/Th2 type response. These results were consistent with the previous report of a similar increase in IgG1, IgG2a levels when Zot (parent molecule of ΔG) was co-administered with tetanus toxoid [12]. In case of EspB alone group, the predominance of IgG1 over IgG2a as implied from the high value of IgG1/IgG2a ratio indicates a possible Th2 type immune response. A significant increase in serum, fecal IgA in EspB + ΔG group as compared to EspB alone group illustrated effective mucosal immune response. This could be attributed to the inherent nature of ΔG to modulate epithelial tight junction permeability [13] to efficiently deliver EspB to underlying lymphoid follicles containing M cells which are involved in antigen uptake and subsequent mucosal immune response. Though not precisely elucidated, the mucosal IgA response in EspB + ΔG group might be due to the probable involvement of plasmacytoid dendritic cells (pDCs) found in the nasal epithelium. The pDCs had been shown to induce IgA production by expressing B cell activating factor (BAFF), a proliferation-inducing ligand (April) in a T cell-independent pathway [37]. Furthermore, the fecal IgA observed in the present study with intranasal immunization of EspB + ΔG also coincides with the recent work showing that lung CD103 + DCs can imprint α4β7 and CCR9 gut-homing receptors and induce T cell migration to the gut where they impart mucosal immune protection [38].
The contribution of cell-mediated immunity was also assessed using the measurement of cytokine levels elicited in the immunized groups. Intranasal vaccination of EspB co-administered with ΔG generated high levels of both Th1 type (IFN-γ), Th2 type (IL-4, IL-10) cytokines. The observed cytokine patterns of EspB + ΔG group correlates with its antibody isotypes implying mixed Th1/Th2 type immune response. On the other hand, intranasal vaccination of EspB alone elicited high levels of Th2 type cytokines (IL-4, IL-10) without any significant increase in Th1 type cytokine (IFN-γ) indicating a solely Th2 type immune response. This was also reflected by the predominance of IgG1 over IgG2a isotype in the EspB alone group. Despite the fact that Th2 type cytokines (IL-4, IL-10) were highest in EspB + ΔG group, the comparable increase in Th1 type cytokine (IFN-γ) in this group emphasizes skewing towards mixed Th1/Th2 type immune response. However, high levels of IL-4, IL-10 especially IL-4 as compared to IFN-γ in EspB + ΔG group coincides with observed mucosal IgA response, as Th2 type cytokines are shown to be involved in mucosal immune response induction [39]. In addition, IFN-γ has been shown to enhance the transport of dimeric IgA through induction of polymeric immunoglobulin receptor [40] which could be the reason for the effective fecal IgA response observed in EspB + ΔG group and absence of the same in EspB alone group. Taken together, these results emphasize the ability of ΔG to increase overall systemic, mucosal, and cellular immune response to recombinant EspB. However, further investigations are required to understand the mechanisms underlying the observed cellular responses and its link to mucosal immunity. Moreover, a recent study by Baumann et al. [35] on different cell lines have shown that the secreted EspB from EPEC enters the cells autonomously suggesting that it might qualify as a novel cell-penetrating effector protein. Given that the Clustal Omega alignment between EspB of EPEC and E. coli O157:H7 has shown to form a closely related phylogenetic clade, it is possible to speculate that the EspB from E. coli O157:H7 could also possess the cell penetrating property. This, in turn, raises the question whether the EspB, EspB + ΔG intranasally administered in the present study possess the autonomous cell penetrating property in an in vivo system and definitely needs to be addressed further. Considering the fact that the delivery efficacy of an autonomous cell penetrating effector proteins are far less compared to T3SS-mediated delivery as reported previously [41], further characterization of EspB in an in vivo system is required to prove it to be a novel cell-penetrating effector protein.
The neutralizing property of sera from immunized groups was assessed by its ability to inhibit haemolysis of murine RBCs and adherence of bacteria to Caco-2 cells. Compared to control, EspB + ΔG group sera exhibited the highest percentage inhibition of haemolysis followed by EspB which correlates with high anti-EspB titers observed in the former group. The haemolysis inhibition property of antibodies could be due to binding, neutralization of the region of EspB responsible for haemolysis as previously reported [25, 31]. EspB, EspB + ΔG group sera showed significantly higher percentage inhibition of E. coli O157:H7 to Caco-2 cells compared to control. However, there was no significant difference in the adherence inhibition capacity between EspB and EspB + ΔG group. It is not surprising that there was no corresponding increase in neutralising property with an increase in anti-EspB antibodies in EspB + ΔG group since factors other than EspB has already been shown to be involved in adherence [42]. The data from fecal shedding assay following E. coli O157:H7 challenge showed that EspB + ΔG group shed a significantly low number of bacteria in the feces and for less duration compared to control group which shed bacteria throughout the observation period. EspB group also shed comparatively low levels of bacteria in the feces than control but were still shedding the bacteria even on the 14th day. The reduction in fecal shedding observed in the present study with EspB was consistent with previous studies wherein immunization of calves with intimin and EspB has been shown to reduce E. coli O157:H7 shedding [30, 43]. Efficient mucosal IgA response observed in EspB + ΔG group could be the reason for enhanced protection conferred by this group as it is shown previously [44] to reduce bacterial load in the cecum. There are also reports which suggest that IgA is not absolutely necessary for preventing E. coli O157:H7 colonization [27, 45]. This could be due to the receptor-mediated transcytosis of IgG across the epithelial barrier [46] to confer protection against E. coli O157:H7 colonization. But studies involving delivery of antigens to the mucosal surface along with mucosal adjuvants to elicit immune response have almost always been accompanied by IgA production and has shown better protection compared to those immunized via parenteral route [31, 47]. Therefore, it is possible to speculate that IgA, though not mandatory, plays a crucial role through its properties such as abundance, competitive inhibition of pathogen binding and immune exclusion [48] in conferring protection against the gastrointestinal pathogen such as E. coli O157:H7. There has been a substantial increase in non-O157 Shiga toxin-producing Escherichia coli (STEC) infection in the past decade [49] and among them the “Big Six” non-O157 EHEC strains have been described by the CDC as the cause of 71% of non-O157 EHEC disease [50]. Therefore, it is highly desirable that the candidate vaccine could provide sufficient cross-protection across the wide array of non-O157 STEC strains. In this regard, several T3SS proteins have shown high sequence homology and the antibodies raised against them have shown cross-reactivity among different EHEC serotypes [19]. Similarly, Clustal Omega analysis of EspB shows high percentage identity among E. coli O157:H7 and the “Big Six” non-O157 EHEC strains. Though not characterized in the present study, the high sequence homology observed among these strains suggests that the probable cross-protection could be obtained using EspB used in the present study. However, it has been previously suggested that cautious interpretation should be made as antibody cross-reactivity as such may not correspond to cross-protection [51]. Further studies are required to substantiate the cross-protective potential of EspB used in the present study against non-O157 strains. Taken together, the results suggest the effective mucosal adjuvanticity of ΔG in eliciting systemic, mucosal and cellular immune response when co-administered with EspB via the intranasal route to confer protection against E. coli O157:H7 shedding. In future studies, our group will attempt to fuse ΔG with multi-epitope vaccines targeting major TTSS proteins to confer enhanced protection against E. coli O157:H7 colonization.
Conclusion
In conclusion, our results demonstrated that ΔG active fragment of Zot, when co-administered with EspB via intranasal route, elicited effective systemic, mucosal and cellular immune response against EspB. Immunization with EspB alone induced an efficient immune response at only systemic level whereas that of EspB + ΔG enhanced it at both systemic and mucosal level which is vital for combating gastrointestinal pathogen like E. coli O157:H7. Sera from EspB + ΔG group displayed more effective haemolysis neutralizing properties compared to EspB alone immunized group, but the adherence inhibition properties of both the groups were almost similar. Moreover, mice immunized with EspB + ΔG could effectively reduce fecal shedding of E. coli O157:H7 in experimentally infected mice compared to mice immunized with EspB alone. Therefore, ΔG could find its potential application in multivalent mucosal vaccine formulation for enhanced protection against E. coli O157:H7. Besides, it also emphasizes the mucosal adjuvant potential of ΔG when co-administered with protein antigens delivered via intranasal route.
References
Karmali MA, Gannon V, Sargeant JM (2010) Verocytotoxin-producing Escherichia coli (VTEC). Vet Microbiol 140:360–370
Varela NP, Dick P, Wilson J (2013) Assessing the existing information on the efficacy of bovine vaccination against Escherichia coli o157: H7—a systematic review and meta-analysis. Zoonoses Public Health 60:253–268
Matthews L, Reeve R, Gally DL et al (2013) Predicting the public health benefit of vaccinating cattle against Escherichia coli O157. Proc Natl Acad Sci USA 110:16265–16270. https://doi.org/10.1073/pnas.1304978110
Potter AA, Klashinsky S, Li Y et al (2004) Decreased shedding of Escherichia coli O157:H7 by cattle following vaccination with type III secreted proteins. Vaccine 22:362–369. https://doi.org/10.1016/j.vaccine.2003.08.007
McNeilly TN, Mitchell MC, Rosser T et al (2010) Immunization of cattle with a combination of purified intimin-531, EspA and Tir significantly reduces shedding of Escherichia coli O157:H7 following oral challenge. Vaccine 28:1422–1428. https://doi.org/10.1016/j.vaccine.2009.10.076
Lin R, Zhu B, Zhang Y et al (2017) Intranasal immunization with novel EspA-Tir-M fusion protein induces protective immunity against enterohemorrhagic Escherichia coli O157:H7 challenge in mice. Microb Pathog 105:19–24. https://doi.org/10.1016/j.micpath.2017.01.062
Wan C, Zhou Y, Yu Y et al (2011) B-cell epitope KT-12 of enterohemorrhagic Escherichia coli O157:H7: a novel peptide vaccine candidate. Microbiol Immunol 55:247–253. https://doi.org/10.1111/j.1348-0421.2011.00316.x
Nart P, Holden N, McAteer SP et al (2008) Mucosal antibody responses of colonized cattle to Escherichia coli O157-secreted proteins, flagellin, outer membrane proteins and lipopolysaccharide. FEMS Immunol Med Microbiol 52:59–68. https://doi.org/10.1111/j.1574-695X.2007.00341.x
Fasano A, Baudry B, Pumplin DW et al (1991) Vibrio cholerae produces a second enterotoxin, which affects intestinal tight junctions. Proc Natl Acad Sci USA 88:5242–5246. https://doi.org/10.1073/pnas.88.12.5242
Fasano A, Uzzau S (1997) Modulation of intestinal tight junctions by zonula occludens toxin permits enteral administration of insulin and other macromolecules in an animal model. J Clin Invest 99:1158–1164. https://doi.org/10.1172/JCI119271
Fasano A, Fiorentini C, Donelli G et al (1995) Zonula occludens toxin modulates tight junctions through protein kinase C-dependent actin reorganization, in vitro. J Clin Invest 96:710–720. https://doi.org/10.1172/JCI118114
Marinaro M, Fasano A, De Magistris MT (2003) Zonula occludens toxin acts as an adjuvant through different mucosal routes and induces protective immune responses. Infect Immun 71:1897–1902. https://doi.org/10.1128/IAI.71.4.1897-1902.2003
Di Pierro M, Lu R, Uzzau S et al (2001) Zonula occludens toxin structure-function analysis. Identification of the fragment biologically active on tight junctions and of the zonulin receptor binding domain. J Biol Chem 276:19160–19165. https://doi.org/10.1074/jbc.M009674200
Salama NN, Fasano A, Thakar M, Eddington ND (2005) The impact of ∆G on the oral bioavailability of low bioavailable therapeutic agents. J Pharmacol Exp Ther 312:199–205. https://doi.org/10.1124/jpet.104.073205
Pavot V, Rochereau N, Genin C et al (2012) New insights in mucosal vaccine development. Vaccine 30:142–154. https://doi.org/10.1016/j.vaccine.2011.11.003
Hamada D, Hamaguchi M, Suzuki KN et al (2010) Cytoskeleton-modulating effectors of enteropathogenic and enterohemorrhagic Escherichia coli: a case for EspB as an intrinsically less-ordered effector. FEBS J 277:2409–2415. https://doi.org/10.1111/j.1742-4658.2010.07655.x
Frankel G, Phillips AD, Rosenshine I et al (1998) Enteropathogenic and enterohaemorrhagic Escherichia coli: more subversive elements. Mol Microbiol 30:911–921. https://doi.org/10.1046/j.1365-2958.1998.01144.x
Kenny B, Finlay BB (1995) Protein secretion by enteropathogenic Escherichia coli is essential for transducing signals to epithelial cells. Proc Natl Acad Sci USA 92:7991–7995
Asper DJ, Karmali MA, Townsend H et al (2011) Serological response of Shiga toxin-producing Escherichia coli type III secreted proteins in sera from vaccinated rabbits, naturally infected cattle, and humans. Clin Vaccine Immunol 18:1052–1057. https://doi.org/10.1128/CVI.00068-11
Reddy PK, Ramlal S, Sripathy MH, Batra H (2012) A simple and universal ligation mediated fusion of genes based on hetero-staggered PCR for generating immunodominant chimeric proteins. Gene 509:104–109. https://doi.org/10.1016/j.gene.2012.08.011
Reichelt P, Schwarz C, Donzeau M (2006) Single step protocol to purify recombinant proteins with low endotoxin contents. Protein Expr Purif 46:483–488. https://doi.org/10.1016/j.pep.2005.09.027
Tadepalli G, Konduru B, Murali HS, Batra HV (2017) Intraperitoneal administration of a novel chimeric immunogen (rOP) elicits IFN-γ and IL-12p70 protective immune response in BALB/c mice against virulent Brucella. Immunol Lett 192:79–87. https://doi.org/10.1016/j.imlet.2017.10.013
Amani J, Mousavi SL, Rafati S, Salmanian AH (2011) Immunogenicity of a plant-derived edible chimeric EspA, Intimin and Tir of Escherichia coli O157:H7 in mice. Plant Sci 180:620–627. https://doi.org/10.1016/j.plantsci.2011.01.004
Reddy PN, Paul S, Sripathy MH, Batra HV (2015) Evaluation of recombinant SEA-TSST fusion toxoid for protection against superantigen induced toxicity in mouse model. Toxicon 103:106–113. https://doi.org/10.1016/j.toxicon.2015.06.008
Martorelli L, Garbaccio S, Vilte DA et al (2017) Immune response in calves vaccinated with type three secretion system antigens and shiga toxin 2b subunit of Escherichia coli O157:H7. PLoS One 12:e0169422. https://doi.org/10.1371/journal.pone.0169422
Ruan X, Sack DA, Zhang W (2015) Genetic fusions of a CFA/I/II/IV MEFA (multiepitope fusion antigen) and a toxoid fusion of heat-stable toxin (STa) and heat-labile toxin (LT) of enterotoxigenic Escherichia coli (ETEC) retain broad anti-CFA and antitoxin antigenicity. PLoS One 10:e0121623. https://doi.org/10.1371/journal.pone.0121623
Amani J, Salmanian AH, Rafati S, Mousavi SL (2010) Immunogenic properties of chimeric protein from espA, eae and tir genes of Escherichia coli O157:H7. Vaccine 28:6923–6929. https://doi.org/10.1016/j.vaccine.2010.07.061
Snedeker KG, Campbell M, Sargeant JM (2012) A systematic review of vaccinations to reduce the shedding of Escherichia coli O157 in the faeces of domestic ruminants. Zoonoses Public Health 59:126–138. https://doi.org/10.1111/j.1863-2378.2011.01426.x
Yekta MA, Goddeeris BM, Vanrompay D, Cox E (2011) Immunization of sheep with a combination of intiminγ, EspA and EspB decreases Escherichia coli O157:H7 shedding. Vet Immunol Immunopathol 140:42–46. https://doi.org/10.1016/j.vetimm.2010.11.010
Vilte DA, Larzábal M, Garbaccio S et al (2011) Reduced faecal shedding of Escherichia coli O157:H7 in cattle following systemic vaccination with γ-intimin C280 and EspB proteins. Vaccine 29:3962–3968. https://doi.org/10.1016/j.vaccine.2011.03.079
Cataldi A, Yevsa T, Vilte DA et al (2008) Efficient immune responses against Intimin and EspB of enterohaemorragic Escherichia coli after intranasal vaccination using the TLR2/6 agonist MALP-2 as adjuvant. Vaccine 26:5662–5667. https://doi.org/10.1016/j.vaccine.2008.07.027
Ahmed B, Loos M, Vanrompay D, Cox E (2014) Oral immunization with Lactococcus lactis-expressing EspB induces protective immune responses against Escherichia coli O157:H7 in a murine model of colonization. Vaccine 32:3909–3916. https://doi.org/10.1016/j.vaccine.2014.05.054
Lin R, Zhang Y, Long B et al (2017) Oral immunization with recombinant lactobacillus acidophilus expressing espA-Tir-M confers protection against enterohemorrhagic Escherichia coli O157:H7 challenge in mice. Front Microbiol 8:417. https://doi.org/10.3389/fmicb.2017.00417
Chiu H-J, Syu W-J (2005) Functional analysis of EspB from enterohaemorrhagic Escherichia coli. Microbiology 151:3277–3286. https://doi.org/10.1099/mic.0.28115-0
Baumann D, Salia H, Greune L et al (2018) Multitalented EspB of enteropathogenic Escherichia coli (EPEC) enters cells autonomously and induces programmed cell death in human monocytic THP-1 cells. Int J Med Microbiol 308:387–404. https://doi.org/10.1016/j.ijmm.2018.03.005
Viswanathan VK, Koutsouris A, Lukic S et al (2004) Comparative analysis of EspF from enteropathogenic and enterohemorrhagic Escherichia coli in alteration of epithelial barrier function. Infect Immun 72:3218–3227. https://doi.org/10.1128/IAI.72.6.3218-3227.2004
Tezuka H, Abe Y, Asano J et al (2011) Prominent role for plasmacytoid dendritic cells in mucosal T cell-independent IgA induction. Immunity 34:247–257. https://doi.org/10.1016/j.immuni.2011.02.002
Ruane D, Brane L, Reis BS et al (2013) Lung dendritic cells induce migration of protective T cells to the gastrointestinal tract. J Exp Med 210:1871–1888. https://doi.org/10.1084/jem.20122762
Yamamoto M, Vancott JL, Okahashi N et al (1996) The role of Th1 and Th2 cells for mucosal IgA responses. Ann N Y Acad Sci 778:64–71. https://doi.org/10.1111/j.1749-6632.1996.tb21115.x
Sollid LM, Kvale D, Brandtzaeg P et al (1987) Interferon-gamma enhances expression of secretory component, the epithelial receptor for polymeric immunoglobulins. J Immunol (Baltimore Md 1950) 138:4303–4306
Rüter C, Lubos ML, Norkowski S, Schmidt MA (2018) All in—Multiple parallel strategies for intracellular delivery by bacterial pathogens. Int J Med Microbiol. https://doi.org/10.1016/j.ijmm.2018.06.007
Etcheverría AI, Padola NL (2013) Shiga toxin-producing Escherichia coli: factors involved in virulence and cattle colonization. Virulence 4:366–372
Martorelli L, Garimano N, Fiorentino GA et al (2018) Efficacy of a recombinant Intimin, EspB and Shiga toxin 2B vaccine in calves experimentally challenged with Escherichia coli O157:H7. Vaccine 36:3949–3959
García-Angulo VA, Kalita A, Kalita M et al (2014) Comparative genomics and immunoinformatics approach for the identification of vaccine candidates for enterohemorrhagic Escherichia coli O157:H7. Infect Immun 82:2016–2026. https://doi.org/10.1128/IAI.01437-13
Babiuk S, Asper DJ, Rogan D et al (2008) Subcutaneous and intranasal immunization with type III secreted proteins can prevent colonization and shedding of Escherichia coli O157:H7 in mice. Microb Pathog 45:7–11. https://doi.org/10.1016/j.micpath.2008.01.005
Yoshida M, Claypool SM, Wagner JS et al (2004) Human neonatal Fc receptor mediates transport of IgG into luminal secretions for delivery of antigens to mucosal dendritic cells. Immunity 20:769–783. https://doi.org/10.1016/j.immuni.2004.05.007
Fan H, Wang L, Luo J, Long B (2012) Protection against Escherichia coli O157:H7 challenge by immunization of mice with purified Tir proteins. Mol Biol Rep 39:989–997. https://doi.org/10.1007/s11033-011-0824-0
Mantis NJ, Rol N, Corthésy B (2011) Secretory IgA’s complex roles in immunity and mucosal homeostasis in the gut. Mucosal Immunol 4:603–611. https://doi.org/10.1038/mi.2011.41
Gould LH, Mody RK, Ong KL et al (2013) Increased recognition of non-O157 shiga toxin–producing Escherichia coli infections in the United States during 2000–2010: epidemiologic features and comparison with E. coli O157 Infections. Foodborne Pathog Dis 10:453–460. https://doi.org/10.1089/fpd.2012.1401
Brooks JT, Sowers EG, Wells JG et al (2005) Non-O157 shiga toxin–producing Escherichia coli infections in the United States, 1983–2002. J Infect Dis 192:1422–1429. https://doi.org/10.1086/466536
McNeilly TN, Mitchell MC, Corbishley A et al (2015) Optimizing the protection of cattle against Escherichia coli O157:H7 colonization through immunization with different combinations of H7 Flagellin, Tir, Intimin-531 or EspA. PLoS One 10:e0128391. https://doi.org/10.1371/journal.pone.0128391
Funding
Aravind S is funded by Senior Research Fellowship from Defence Research and Development Organisation, India. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that no conflict of interest exists.
Ethical approval
For this type of study, formal consent is not required.
Statement on the welfare of animals
All procedures performed in studies involving animals were in accordance with the ethical standards of the institution as per the Institutional Animal Ethical Committee (IAEC code 15/2016), DFRL, Mysuru, Karnataka, India.
Data availability statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Rights and permissions
About this article
Cite this article
Shekar, A., Ramlal, S., Jeyabalaji, J.K. et al. Intranasal co-administration of recombinant active fragment of Zonula occludens toxin and truncated recombinant EspB triggers potent systemic, mucosal immune responses and reduces span of E. coli O157:H7 fecal shedding in BALB/c mice. Med Microbiol Immunol 208, 89–100 (2019). https://doi.org/10.1007/s00430-018-0559-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-018-0559-9