Abstract
Background
HCMV hyperimmunoglobulin-preparations (HIG) contain high concentrations of HCMV-specific IgG. The reduced maternofetal-HCMV-transmission rate of IgG may be due to HCMV-specific neutralizing antibodies against the HCMV pentameric complex (PC). In contrast to HIG, standard intravenous immunoglobulin (IVIG) may have more neutralization (NT) capacity than HIG due to higher IgG subclass 3 levels (Planitzer et al., 2011).
Methods
We investigated the HCMV-specific NT-capacity of HIG Cytotect®, using a recombinant pentameric complex (gHgLUL128-131A) for specific antibody-depletion. We used a modified UL130-peptide (TANQNPSPPWSKLTYSKPH) based on original-sequence of Saccoccio et al. (Vaccine 29(15):2705–2711, 2011) (SWSTLTANQNPSPPWSKLTY) as neutralization target. Both UL130-peptides and the PC were bound via sixfold HisTag and anti-HisTag mAbs to magnetic beads to deplete HCMV-specific IgGs from HIG (Cytotect®). Modifying this depletion strategy, we analyzed the role of IgG subclass 3 in both HIG and IVIG.
Results
After CMV IgG-normalization of HIG and IVIG, we found a significant trend towards a decrease (16%) of neutralization-capacity for the UL130 TAN-peptide, but not for the original UL130 SWS-peptide. However, highly significant loss of NT-capacity could be only observed by PC depletion (42%). The IgG subclass 3 depletion revealed no significant reduction of NT-capacity in both HIG and IVIG.
Conclusion
Via specific antibody depletion, we could demonstrate that pentameric complex-specific antibodies are present in HIG and bind to the recombinant PC resulting in a highly significant reduction of NT-capacity compared to the UL130 TAN-and SWS-peptides. We could not confirm the functional role of IgG subclass 3 neutralizing antibodies in IgG-preparations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
HCMV is a ubiquitous virus that causes an incidence of congenital infection in the range of 0.2–2% of all live births. After a primary maternal infection during pregnancy maternal–fetal transmission rates increase from 9% in early or preconceptional pregnancy to 65% in the third trimester. Maternal HCMV primary infection during pregnancy is asymptomatic in about 80% of cases. HCMV may cause several neuronal disorders resulting in long-term sequelae that include hearing loss and mental retardation [1]. Effective vaccines to prevent HCMV primary infection and maternofetal transmission are unavailable. A promising vaccine candidate for glycoprotein B failed in a phase II study to induce high titers of neutralizing antibodies [2].
Glycoprotein B is a fusion protein that mediates with gH/gL-complexes the viral entry process into cells [3,4,5,6]. Using a murine cytomegalovirus animal model (MCMV), two viral gH/gL entry complexes (gH/gL/gO and gH/gL/MCK-2) have been identified. While gH/gL/gO of MCMV is essential for initial infection in host organs, the subsequent spread within tissues such as the salivary gland is provided by both entry complexes gH/gL/gO and gH/gL/MCK-2 [7]. In humans, the trimer complex gH/gL/gO is responsible for viral entry into fibroblasts [8, 9] and there is an alternative gH/gL complex, formed by gH/gL/pUL(128,130,131A). This pentameric complex promotes viral entry into epithelial, endothelial, dendritic, and monocytic cells [10,11,12,13] and is involved in maternal–fetal transmission of HCMV [14].
During natural infection, antibodies binding to the HCMV pUL128–131 glycoproteins are generally potent neutralizers [15]. Therefore, the pentameric complex is a major target for neutralizing antibody responses and vaccine development [16]. However, the pleiotropic humoral immune response during early gestation after a primary maternal infection induces antibodies to HCMV gB as well as to the PC. A monoclonal antibody against the glycoprotein B inhibited the infection of placenta-related trophoblast progenitor cells (TBPCs), but two monoclonal antibodies against the PC did not [17]. TBPCs possess no PC-related receptor in contrast to epithelial or endothelial cells. A delay of maternal antibodies to PC is associated with fetal HCMV-transmission during primary infection [18].
HIG for treatment of HCMV primary infected pregnant women shows a trend towards reduction of HCMV transmission to the fetus and reduced disease at birth [19,20,21,22]. However, the HIG treatment of HCMV primary infected pregnant women is not generally recommended outside of clinical trials, according to the current consensus recommendation [23].
The aim of this in vitro study was to demonstrate that potent neutralizing antibodies against the HCMV pentameric complex, especially against defined UL130 peptides are present in HIG preparations and may potentially play an important role in prevention of maternofetal HCMV transmission [24]. Recently, we characterized the IgG subclass distribution of HCMV hyperimmunoglobulin preparations Cytotect® and Cytogam®, as well as the IgG subclass distribution in standard immunoglobulins Kiovig®, Octagam® and Gammunex® [25]. We could demonstrate that IgG 1 is predominantly present with about 50–70% of all IgG subclasses in HIG and IVIG. Interestingly, IgG subclass 3 and 4 were found in remarkably low concentrations (< 2%). IgG subclass 3 antibodies were suggested to be mostly efficient in neutralization of HCMV in immunoglobulin preparations [26], according to former data of the impact of IgG subclass antibodies [27]. We performed additional depletion experiments of the IgG subclass 3 from Cytotect® and Kiovig® to investigate their impact on HCMV-specific NT capacity.
Methods
Reference pools
For calibration of HCMV-neutralization, we generated an HCMV-IgG positive/IgM negative serum pool of 100 healthy HCMV latently infected mothers at birth. The HCMV IgG/IgM serostatus was analyzed via five different assay systems CLIA® (DiaSorin), CMIA® (Abott), ECLIA® (Roche), ELISA Enzygnost® (Siemens), ELISA® (Medac). Only sera with concordant test results were included and used as positive control cohort of reactive HCMV-neutralizers.
Additionally, we used an HCMV-IgG negative/IgM negative serum pool of 100 healthy HCMV-seronegative women at birth. The test results in all five assay systems were concordant HCMV-IgG/IgM negative for the included sera. The negative pool forms the baseline of our NT assays with a neutralization capacity of 0%. Both serum pools represent two greatly comparable collectives of clinical serum samples of pregnant women at birth. The samples derived from the cCMV screening study in Tuebingen and were cryopreserved until use, approved by our local Ethics Committee at the University Hospital of Tuebingen; EK number 506/2015BO2 [24, 25].
Target cells
The neutralization assays were performed using human foreskin fibroblasts (HFF) form ATCC (LOT: 62339645); passage: 18–26 [DMEM (1X) Dubecco’s Modified Eagle Medium, Gibco®] and retinal pigment epithelial cell monolayers (ARPE-19 cells) from ATCC (LOT: 59814960); passage: 19–27 (DMEM F12 Medium, Gibco®). Cell culture was biweekly tested for mycoplasma contamination [25].
Virus strains
We used defined dilutions of cell-free culture supernatants; containing an HCMV-isolate from amniotic fluid (H2497-11) which was first isolated and propagated on HFF or directly isolated and propagated on ARPE-19 cells without any previous adaption to HFF. The quantity of infectious virions were determined, using tissue culture infectious dose 50% (TCID50) determination after virus passage 20 for HFF (6.4 TCID50/ml) and virus passage 21 for ARPE-19 cells after 18 h incubation, which reached a value of 5.2 TCID50/ml. A least, a serial passage number of 16 was necessary to obtain cell-free virus from cell culture supernatant [25].
Immunoglobulin preparations
Cytotect® was used as HIG preparation for PC antibody depletion (Biotest Pharma, charge: B797033|50 mg/ml), as well as the IVIG preparation Kiovig® as additional control (Baxter charge: LE12M265BC|100 mg/ml). Proteins, IgG subclass analysis and HCMV-specific IgG antibodies were characterized in a previous work [25].
UL130 peptide design
The modified UL130 peptide TANQNSPPWSKLTYSKPH (TAN) based on the original UL130 peptide from Saccoccio SWSTLTANQNPSPPWSKLTY (SWS) (Table 1), which induced neutralizing antibodies in a rabbit animal model showed a high antigenicity scale [28, 29]. Our modified UL130 TAN-peptide showed the highest “percentage of probability” (> 75%) for epitope similarity. The peptide synthesis was performed by Intavis Peptide Services, Reutlingen Germany with an additionally 6xfold HisTag on the respective C-terminus (TANQNSPPWSKLTYSKPH-HHHHHH) for magnetic bead anti-HisTag antibody labeling. The epitopes were designed with software for linear epitopes by the use of the sequence of the strain Merlin HCMV protein UL130, which was obtained from the “Uniprot Code”: P16772 (available online: http://www.uniprot.org/uniprot/P16772). These computer servers were used for the epitope prediction: “BepiPred” (http://www.cbs.dtu.dk/services/BepiPred/) [30] and “SVMTriP” (http://sysbio.unl.edu/SVMTriP) [29, 31]. The physical and chemical properties were calculated with the computer server “Bcepred” (http://crdd.osdd.net/raghava/bcepred/), which included hydrophobicity, flexibility and accessibility [32]. In addition, the three-dimensional structure of UL130 region was predicted theoretically, using the computer server “I-TASSER”: (https://zhanglab.ccmb.med.umich.edu/I-TASSER/) [33].
Recombinant HCMV pentameric complex
The investigated HCMV pentameric complex is a recombinant product, which was generated by The Native Antigen Company, Oxfordshire UK (Product Code: HCMV-PENT) and was used in a concentration of 0.01 mg /ml. This native-like HCMV pentameric complex is produced in human cells (HEK293) to ensure that all proteins are properly folded and possess their native glycosylation pattern. The presence of all five proteins in the purified complex was confirmed by mass spectrometry. According to the manufacturer, there is an additional sixfold HisTag linked to gH. The genetic background for the recombinant HCMV pentameric complex is the VR1814 strain.
HCMV antibody depletion strategy
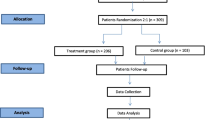
First, we analyzed HCMV-specific peptides, which are part of the HCMV pentameric UL130 region with an additional sixfold [HisTag] on the C-terminus (Fig. 1). In a second experiment, we used a recombinant pentameric complex with a linked sixfold [HisTag] on glycoprotein H. In both approaches, we used magnetic beads (Cell Signaling Technology, Danvers United States), which is coated via biotin-streptavidin bridge with protein G to attach monoclonal anti-HisTag-antibodies to the bead surface. After incubation for 24 h at 37 °C, the bead-fixed immune complex was mixed with serial diluted IgG preparations, followed by a second incubation for 24 h at 37 °C.
HCMV pentameric depletion scheme: two UL130-peptides and a recombinant pentameric complex were bound via sixfold HisTag to magnetic beads, which were coated with biotin-streptavidin bridge and protein G to attach anti-HisTag monoclonal antibodies. This peptide-magnetic bead complex was used to deplete epitope-specific antibodies from polyclonal sera and IgG preparations via a 6 Tube magnetic separation rack. The depleted supernatant was used for in vitro NT assay experiments
Using a 6 Tube magnetic separation rack, bound HCMV-specific immune complexes were depleted and supernatant were transferred into new tubes. The magnetic beads, anti-HisTag-monoclonal antibodies as well as the 6-tube magnetic separation rack were derived from Cell Signaling Technology (Danvers, USA).
For the IgG subclass 3 depletion in immunoglobulin preparations, we modified the given antibody depletion strategy (Fig. 1), which is shown in Fig. 2. We linked anti-human IgG 3 mAb (Product code: 5247-9850, Clone: 5G12, Mouse-anti-human; BioRad laboratories, USA) to magnetic beads, to deplete IgG subclass 3 antibodies from Cytotect® and Kiovig®.
Long term cell-free HCMV plaque reduction assay (HCMV-PRA)
The dilution of cell-free virus supernatant (H2497-11) was adjusted to generate approximately 100 HCMV plaques per well in 96-well micotiter-plates after 5d incubation in the HCMV-IgG negative control.
The test was performed as described recently [25]. Briefly, serial sample dilutions (1:50, 1:500, 1:1000, 1:5000, and 1:10000) were used to define the NT50 values of the investigated IgG preparations. Serum dilutions were pre-incubated with cell-free HCMV H2497-11 (250× TCID50/ml) at 37 °C for 1 h and were inoculated to microtiter-plates containing initially 20000 target cells/well (ARPE-19 or HFF cells), including negative and positive controls. For neutralization testing, the dilution of cell-free virus supernatant was adjusted to form about (n = 100) HCMV plaques/well in 96-well micotiter-plates after 5d of virus-cell culture incubation in the HCMV-IgG negative control.
The IgG-preparations were used in two different dilution patterns—first, we used the HCMV IgG-concentration of the original stock IgG preparations (stock-HCMV-IgG-PRA) and secondly, we normalized the HCMV IgG-concentration of the IgG-preparations to the HCMV IgG level of the serum positive pool of 100 latently infected mothers at birth (normalized HCMV-IgG-PRA) [25]. We calculated the semi-quantitative neutralization capacity (%) to generate a calculation base, which leads to elimination of test-dependent microtiter-plate-factor. The IgG seronegative pool represents an infection rate of 100% or rather a neutralization capacity of 0%. Complement inactivation was performed at 56 °C for 30 min prior to neutralization assays.
In the absence of a WHO HCMV IgG unit standard, we used the HCMV PEI standard (110 U/ml, ELISA: Enzygnost® Anti-HCMV/IgG Siemens Healthcare Diagnostics) from 1996 to calibrate our NT assays [25].
Statistical analysis
All compiled data were measured in threefold replica, calibrating mean and standard deviation for further statistical analysis. We compared the percentage of neutralization capacity to reflect the variation of viral plaque numbers in each individual microtiter-plate (plate-factor). For PROBIT analysis and p value determination the statistic programs PASW Statistics version 18 (SPSSInc® Company) and JMP version 18 (SAS® Company) were used. The Wilcoxon signed-rank test was used to compare quantitative measured values between defined groups.
Results
On the computer-based server analysis of the UL130 peptide (TAN), we predicted five antigenic regions (Suppl. Mat. Fig. 1A, B). Both servers showed concordance and high scores between positions W29 and H51. The properties of hydrophilicity, flexibility, and accessibility had a considerable score value (Suppl. Mat. Fig. 1C), whereas the tridimensional structure obtained by crystallography (code: 5VOB on the Protein Data Bank, available online: https://www.rcsb.org/pdb/explore/explore.do?structureId=5VOB) was similar with our theoretical prediction (Suppl. Mat. Fig. 2).
In the first plaque reduction assay (PRA), undiluted HCMV-IgG stock solutions of the investigated IgG-preparations Cytotect® and Kiovig® were analyzed for their impact on specific NT-capacity reduction using the UL130 TAN-peptide with ARPE-19 target cells (Fig. 3a). Cytotect® showed the highest NT-capacity, followed by Kiovig®, while the HCMV-IgG + pool had the lowest level of NT-capacity. The HCMV-specific IgG reduction effect using Cytotect® showed with (16%; p = 0.12) the highest difference of NT reduction at a dilution of 1:5000 or 29.44 mPEI U/ml HCMV IgG resulting from the difference between the native samples (75%) and depleted samples (59%).
a1 TAN-peptide antibody depletion was used in PRA with normalized HCMV IgG concentrations to show the impact on NT-capacity (%) on ARPE-19 target cells; a2 NT50 PROBIT analysis of the PRA using TAN-peptide antibody depletion with normalized HCMV IgG concentration. b1 SWS-peptide antibody depletion was used in a PRA with normalized HCMV IgG concentration to reveal the impact on NT-capacity (%) on ARPE-19 target cells; b2 NT50 PROBIT analysis of the PRA using SWS-peptide antibody depletion with normalized HCMV IgG concentration
a1 PRA was performed using a recombinant pentameric complex to deplete PC-specific antibodies from IgG-preparations without CMV IgG predilution on ARPE-19 target cells; a2 NT50 PROBIT analysis of the PRA on ARPE-19 target cells using PC-specific antibody depletion with stock HCMV IgG concentration. b1 PRA was performed to deplete PC-specific antibodies from IgG-preparations with stock HCMV IgG concentration on fibroblasts as target cells; b2 NT50 PROBIT analysis of the PRA on fibroblasts as target cells (PRA) using PC-specific antibody depletion without HCMV IgG predilution
For Kiovig®, the highest reduction effect (15%; p = 0.11) was found at dilution 1:5000 or 8.24 mPEI U/ml HCMV IgG and the HCMV IgG + pool revealed the greatest difference (11%; p = 0.11) at 1:1000 corresponding to 42.62 mPEI U/ml HCMV IgG. The NT50 values for the investigated IgG preparations and the HCMV-IgG + pool are shown in Fig. 3b via PROBIT analysis. The NT50-values decreased in all HCMV IgG samples after IgG depletion. However, the HCMV-IgG-specific depletion effects showed only non-significant trends towards decrease of NT-capacity in all tested samples. For proof of principle, we found no significant reduction-effects on NT-capacity using human foreskin fibroblasts as target cells (p = 0.78 HCMV-IgG + pool; p = 0.65 Cytotect®; p = 0.69 Kiviog®) (data not shown).
In a second step, following HCMV IgG normalization of stock solutions of the IgG-preparations, we analyzed in a PRA the impact on NT-capacity using both UL130 peptides (TAN) (Fig. 4a1) and (SWS) (Fig. 4b1) against ARPE-19 cells. In both experiments the IgG preparations (Cytotect®, Kiovig®) and the HCMV IgG + reference pool showed similar NT-capacities to HCMV IgG concentrations of the latently infected mothers.
Interestingly, both Cytotect® (p = 0.01) and Kiovig® (p = 0.02) showed a significant difference between the native and depleted sample using the TAN-peptide. Furthermore, comparing the NT-capacity reduction effects of our modified TAN-peptide (TANQNPSPPWSKLTYSKP) with that of Saccoccio et al. [28] (SWSTLTANQNPSPPWSKLTY) [28], we could detect similar contribution of both peptides in HCMV antibody binding and NT-capacity. The reduction effects were about 15% at the maximum in both UL130 peptide depletion tests. The PROBIT analysis confirmed our result and showed similar decreases of NT50 values comparing the depleted and the native samples of the TAN- and SWS-peptide (Fig. 4a2, b2).
For the pentameric complex, we investigated the specific antibody depletion using ARPE-19 cells with normalized CMV IgG concentration of the different IgG preparations (Fig. 5a1). The total number of HCMV plaques in the reference HCMV-IgG-negative pool was n = 83 (mean ± 2). The effect of HCMV IgG depletion of Cytotect® showed a significant difference (42%) of NT reduction at a dilution of 1:5000 or 29.44 mPEI U/ml HCMV IgG resulting from difference between the native (57%) and depleted samples (15%) (p < 0.05; 0.01).
The HCMV IgG + pool showed the highest reduction effect of NT-capacity (30%) and a significant difference (p < 0.05; 0.03) at dilution 1:1000 or 42.62 mPEI U/ml HCMV IgG between the native and depleted samples. NT50-values (Fig. 5a2), revealed a significant HCMV-specific antibody depletion effect of the recombinant PC. Interestingly, the ECLIA assay system was not able to detect any difference of HCMV-specific IgG-antibody binding between native and depleted samples of Cytotect® at a dilution of 1:5000 or 29.44 mPEI U/ml HCMV IgG and the HCMV-IgG + pool at a dilution of 1:1000, respectively, 42.62 mPEI U/ml HCMV IgG (Table 2). For a control, we also investigated the decrease of NT-capacity after PC depletion using fibroblasts as target cells (Fig. 5b1). Comparing the reduction of NT-capacity effects, Cytotect® and the HCMV-IgG + pool showed no significant differences in human foreskin fibroblasts (p > 0,05; 0.68/0.87) (Fig. 5b2). In Fig. 6, the results for the IgG subclass 3 depletion are given for ARPE-19 cells (Fig. 6a1, a2) and for HFF (Fig. 6a1, a2). Comparing NT50-values, we could not observe any significant difference (p > 0.05) in NT-capacity before and after IgG 3 depletion for Cytotect® and Kiovig®, as well as for our HCMV-IgG + reference pool of latently infected mothers.
a1 IgG preparations Cytotect® and Kiovig® were used in stock HCMV IgG concentrations in a PRA after depletion of IgG subclass 3 antibodies, performed on ARPE-19 cells. b1 NT50 PROBIT analysis of the PRA on ARPE-19 cells, using IgG subclass 3 antibodies for depletion of pAbs from Cytotect® and Kiovig®. b1 After depletion of IgG subclass 3 antibodies, Cytotect® and Kiovig® were used in a PRA on HFF. b2 NT50 PROBIT analysis of the PRA on HFF, using Cytotect® and Kiovig®, which were pervious depleted with IgG subclass 3 antibodies
Discussion
HCMV-specific hyperimmunoglobulin preparations such as Cytotect® are pooled sera of healthy donors with high HCMV-specific IgG concentrations. We found that HIG preparations contain higher concentrations of HCMV neutralizing antibodies than standard IgG preparations as observed using plaque reduction NT assays with epithelial target cells. We also observed that HIGs contain lower concentration of total IgG, but higher concentrations of HCMV-specific IgG than standard IgG preparations using the Roche ECLIA HCMV IgG test system. We also analyzed the IgG subclass distribution in immunoglobulin preparations with very low concentrations of IgG 3 and IgG 4 [25]. A former study postulated, that IgG subclass 3 would have main impact on CMV neutralization in HIG and IVIG preparations which would result in higher functional HCMV neutralization titers for Kiovig® than for Cytotect® [26]. Therefore, we depleted subclass 3 IgG in modification to PC depletion from both immunoglobulin preparations. We demonstrated that IgG 3 subclass depletion did not result in any significant reduction of the functional NT capacity for both IgG preparations and the target cell types of fibroblast and epithelial cells. Importantly, in contrast to the IgG subclass 3 levels, the different HCMV-specific IgG concentrations in HIGs and IVIGs stock solutions were not considered in context of their resulting NT capacity [26].
Furthermore, in all depletion experiments of UL130 peptides, PC, and IgG 3, we observed that the HIG Cytotect® has a higher NT-capacity than the IVIG Kiovig® using stock concentrations, which confirmed data of our former study analyzing selected IVIG and HIG preparations [25]. Our characterization of the NT-capacity of HIGs and standard IgG preparations, calibrated with HCMV IgG PEI units/ml was also confirmed [34, 35]. Like Wang et al. [35], we observed that the HIG preparations of PEI CMV standard, Cytotect® and Cytogam® have similar biochemical compositions with respect to total protein, albumin, IgG class and subclass distributions. Furthermore, CMV-specific IgG antibodies were two- to threefold higher in HIGs than in standard IgG preparations like Kiovig® with high NT-capacity in vitro [25].
Based on these findings, we wanted to evaluate the HCMV antibody binding and NT-capacity against HCMV pentameric complex, especially against defined epitopes of the UL130 region. We used a peptide design the region W29-H51 of the UL130 peptide, which is given in (Suppl. Mat. Fig. 1A, B). The high antigenicity for this region was described and showed optimal physical and chemical properties as well (Fig. 1c). In an analysis of protein modelling, T46 was reported as part of our TAN peptide to be involved in the complex stabilization of the UL130 [36]. We also observed structural similarities between our tridimensional predicted model and a model that used crystallographic analysis [36].
In the PRAs, we confirmed HCMV-specific antibodies against PC and TAN/SWS-peptides in both HIG and IVIG by magnetic bead peptide depletion and their individual specific contribution on virus neutralization in vitro against ARPE-19 target cells. Using stock solutions of HIG and IVIG, we found significant reduction of NT capacity only by depletion of PC-specific antibodies, while UL130 peptide specific antibody depletion via TAN- and SWS-peptides showed a non-significant trend forward reduction of NT capacity.
In contrast, no PC-dependent antibody depletion effect was found using human foreskin fibroblasts. This observation confirmed former data, that HCMV uses another mechanism of viral entry into fibroblasts than into epithelial cells [3,4,5,6,7,8,9,10,11,12,13]. This result also confirmed the variations in NT-capacity of IgG preparations using different target cells [37]. Ryckman described the UL128-UL130A region is mainly responsible for viral entry into epithelial and endothelial cells as part of pentameric complex and confirmed former findings of Wang and Adler, which revealed the requirement of the pentameric complex for epithelial and endothelial cell tropism [9, 12, 15]. In this context, the UL128-131 genes are also essential for viral growth in endothelial cells, followed by viral transfer to leukocytes [10]. The depletion of gH/gL-specific antibodies using another hyperimmunoglobulin preparation (Cytogam® from CSL Behring) induced hardly any decrease of NT-capacity compared to PC depletion [38]. Therefore, the UL128-131 region of the pentameric complex seems to be mainly responsible for virus neutralization and not the gH/gL fragment alone [38]. The results of our UL130 TAN/SWS peptide depletion experiments support this hypothesis. Interestingly, we observed a substantial amount of NT reduction via polyclonal antibodies present in the HIG preparation (Cytotect®) using the UL130 TAN and SWS peptides (16%), compared to the NT reduction via polyclonal HIG-antibodies directed against the full-length pentameric complex with 42%. However, it might be due to the fact that gH/gL dimers might fail to effectively reduce the in vitro NT-capacity [38] because of an unphysiological conformation, compared to a complete PC (gH/gL-UL128-131A). Macagno et al., 2010 showed that neutralizing mAbs need a co-expressing of at least two genes of the UL128 locus (UL128/UL130 and UL128/UL131A). This fact could explain the non-significant reduction of NT-capacity, using single UL130-specific peptides like TAN and SWS in our work. But it has to be considered, that Magcagno investigated four neutralizing mABs, which may not recognize all present epitopes for effective neutralization. This might be the source for a still observed NT reduction of 16% using the polyclonal IgG preparation Cytotect®.
Our results of the antibody depletion from IgG preparations, using the UL130 TAN peptide are confirmatory and revealed additional defined expressed epitopes of this gene region in modification to Saccocio et al. [28]. Gerna et al. [45] investigated components of the pentameric complex, especially the UL128-UL131A region in context of anti-HCMV therapeutic antibodies and potential HCMV-vaccines [40]. In a further study, domain-specific antibodies against the UL128-UL131A region were identified [41]. We could not detect any difference of HCMV-specific antibodies between native and depleted samples using the ECLIA HCMV IgG® test system (Table 2). We suggest, that the ECLIA assay using recombinant mixture of HCMV-specific antigens, does not bind a substantial amount of polyclonal pentameric complex-specific antibodies which are present in HIG preparations. However, PC-specific antibodies seem to be crucial for HCMV neutralization in epithelial and endothelial cells. This correlates with our observation that HCMV-specific antibody binding and corresponding NT-capacity may differ, since women with high ECLIA values (> 500 U/ml), may have very low in vitro neutralization titers and vice versa (data not shown).
The expression of the pentameric complex was described using a Chinese hamster ovary (CHO) system for future vaccine production [42]. The maternal–fetal transmission of HCMV through the placenta depends on known and unknown factors which involve a complex interaction of different cell types. We suggest that the divergent findings of Fouts and Zydek are part of the multistep maternofetal transmission process [14, 17]. More recently, neutralizing mAbs to one, or more components of the pUL128L blocked syncytium formation in highly infected ARPE-19 epithelial cells, whereas only a partial inhibitory effect occurred with mAbs against the trimer gH/gL/gO or against gB at comparable concentrations [40].
In the absence of an efficient vaccine, HIGs are the only relevant treatment option to manage HCMV primary infection in pregnant women in the first trimester, combined with an early hygiene-counseling of the women to prevent the HCMV infection following maternal–fetal transmission [43]. However, the administration of HIG is not recommended outside of clinical studies since the only available RCT study did not reach statistical significance in reduction of maternofetal transmission using a 4 week administration study design [19, 22]. In our in vitro investigations, we aim to elucidate the mode of action of these antibody preparations to develop an optimized HIG application scheme [24, 44].
In conclusion, the HCMV pentameric complex is a target for virus-specific antibody binding and neutralization that may lead to an effective HCMV vaccine [45]. Our in vitro experiments demonstrate that HIG and IVIG preparations contain PC-specific antibodies with high NT capacity, potentially able to prevent maternal–fetal HCMV transmission in early pregnancy [24].
References
Picone O, Vauloup-Fellous C, Cordier AG, Guitton S, Senat MV, Fuchs F, Ayoubi JM, Grangeot Keros L, Benachi A (2013) A series of 238 cytomegalovirus primary infections during pregnancy: description and outcome. Prenat Diagn 33(8):751–758
Pass RF (2009) Development and evidence for efficacy of HCMV glycoprotein B vaccine with MF59 adjuvant J. Clin Virol 46:73–76
Connolly SA, Jackson JO, Jardetzky TS, Longnecker R (2011) Fusing structure and function: a structural view of the herpesvirus entry machinery. Nat Rev Microbiol 9:369–381
Eisenberg RJ, Atanasiu D, Cairns TM, Gallagher JR, Krummenacher C et al (2012) Herpes virus fusion and entry: a story with many characters. Viruses 4:800–832
Ciferri C, Chandramouli S, Donnarumma D, Nikitin PA, Cianfrocco MA, Gerrein R, Feire AL, Barnett SW1, Lilja AE, Rappuoli R, Norais N, Settembre EC, Carfi A (2015) Structural and biochemical studies of HCMV gH/gL/gO and Pentamer reveal mutually exclusive cell entry complexes. Proc Natl Acad Sci USA 112(6):1767–1772
Stegmann C, Abdellatif ME, Laib Sampaio K, Walther P, Sinzger C (2016) Importance of highly conserved peptide sites of human cytomegalovirus gO for formation of the gH/gL/gO complex. J Virol. 91(1):e01339-16
Lemmermann NA, Krmpotic A, Podlech J, Brizic I, Prager A, Adler H, Karbach A, Wu Y, Jonjic S, Reddehase MJ, Adler B (2015) Non-redundant and redundant roles of cytomegalovirus gH/gL complexes in host organ entry and intra-tissue spread. PLoS Pathog 11(2):e1004640
Vanarsdall AL, Chase MC, Johnson DC (2011) Human cytomegalovirus glycoprotein gO complexes with gH/gL, promoting interference with viral entry into human fibroblasts but not entry into epithelial cells. J Virol 85:11638–11645
Adler B, Scrivano L, Ruzcics Z, Rupp B, Sinzger C, Koszinowski U (2006) Role of human cytomegalovirus UL131A in cell type-specific virus entry and release. J Gen Virol 87(Pt 9):2451–2460
Hahn G, Revello MG, Patrone M, Percivalle E, Campanini G, Sarasini A, Wagner M, Gallina A, Milanesi G, Koszinowski U, Baldanti F, Gerna G (2004) Human cytomegalovirus UL131-128 genes are indispensable for virus growth in endothelial cells and virus transfer to leukocytes. J Virol 78(18):10023–10033
Gerna G, Percivalle E, Lilleri D, Lozza L, Fornara C et al (2005) Dendritic-cell infection by human cytomegalovirus is restricted to strains carrying functional UL131–128 genes and mediates efficient viral antigen presentation to CD8+ T cells. J Gen Virol 86:275–284. PMID
Wang D, Shenk T (2005) Human cytomegalovirus virion protein complex required for epithelial and endothelial cell tropism. Proc Natl Acad Sci USA 102(50):18153–18158
Sinzger C, Eberhardt K, Cavignac Y, Weinstock C, Kessler T et al (2006) Macrophage cultures are susceptible to lytic productive infection by endothelial-cell-propagated human cytomegalovirus strains and present viral IE1 protein to CD4 + T cells despite late downregulation of MHC class II molecules. J Gen Virol 87:1853–1862
Fouts AE, Chan P, Stephan JP, Vandlen R, Feierbach B (2012) Antibodies against the gH/gL/UL128/UL130/UL131 complex comprise the majority of the anti-cytomegalovirus (anti-CMV) neutralizing antibody response in CMV hyperimmune globulin. J Virol 86(13):7444–7447
Ryckman BJ, Rainish BL, Chase MC, Borton JA, Nelson JA, Jarvis MA, Johnson DC (2008) Characterization of the human cytomegalovirus gH/gL/UL128-131 complex that mediates entry into epithelial and endothelial cells. J Virol 82(1):60–70
Ha S, Li F, Troutman MC, Freed DC, Tang A, Loughney JW, Wang D, Wang IM, Vlasak J, Nickle DC, Rustandi RR, Hamm M, DePhillips PA, Zhang N, McLellan JS, Zhu H, Adler SP, McVoy MA, An Z, Fu TM (2017) Neutralization of diverse human cytomegalovirus strains conferred by antibodies targeting viral gH/gL/pUL128-131 pentameric complex. J Virol 91(7):e02033-16. https://doi.org/10.1128/JVI.02033-16
Zydek M, Petitt M, Fang-Hoover J, Adler B, Kauvar LM, Pereira L, Tabata T (2014) HCMV infection of human trophoblast progenitor cells of the placenta is neutralized by a human monoclonal antibody to glycoprotein B and not by antibodies to the pentamer complex. Viruses 6(3):1346–1364
Lilleri D, Kabanova A, Revello MG, Percivalle E, Sarasini A et al (2013) Fetal human cytomegalovirus transmission correlates with delayed maternal antibodies to gH/gL/pUL128-130-131 complex during primary infection. PLoS One 8:e59863
Nigro G, Adler SP, La TR, Best AM (2005) Passive immunization during pregnancy for congenital cytomegalovirus infection. Engl J Med 353:1350–1362
Visentin S, Manara R, Milanese L, Da Roit A, Forner G, Salviato E, Citton V, Magno FM, Orzan E, Morando C, Cusinato R, Mengoli C, Palu G, Ermani M, Rinaldi R, Cosmi E, Gussetti N (2012) Early primary cytomegalovirus infection in pregnancy: maternal hyperimmunoglobulin therapy improves outcomes among infants at 1 year of age. Clin Infect Dis 55(4):497–503
Buxmann H, Stackelberg OM, Schlößer RL, Enders G, Gonser M, Meyer-Wittkopf M, Hamprecht K, Enders M (2012) Use of cytomegalovirus hyperimmunoglobulin for prevention of congenital cytomegalovirus disease: a retrospective analysis. J Perinat Med 40(4):439–446
Revello MG, Lazzarotto T, Guerra B, Spinillo A, Ferrazzi E, Kustermann A, Guaschino S, Vergani P, Todros T, Frusca T, Arossa A, Furione M, Rognoni V, Rizzo N, Gabrielli L, Klersy C, Gerna G, CHIP Study Group (2014) A randomized trial of hyperimmune globulin to prevent congenital. N Engl J Med 370(14):1316–1326
Rawlinson WD, Boppana SB, Fowler KB, Kimberlin DW, Lazzarotto T, Alain S, Daly K, Doutré S, Gibson L, Giles ML, Greenlee J, Hamilton ST, Harrison GJ, Hui L, Jones CA, Palasanthiran P, Schleiss MR, Shand MW, van Zuylen WJ (2017) Congenital cytomegalovirus infection in pregnancy and the neonate: consensus recommendations for prevention, diagnosis, and therapy. Lancet Infect Dis 17(6):e177–e188
Kagan KO, Enders M, Schampera MS, Baeumel E, Hoopmann M, Geipel A, Berg C, Goelz R, De Catte L, Wallwiener D, Brucker S, Adler SP, Jahn G, Hamprecht K (2018) Prevention of maternal-fetal transmission of CMV by hyperimmunoglobulin (HIG) administered after a primary maternal CMV infection in early gestation. Ultrasound Obstet Gynecol. https://doi.org/10.1002/uog.19164
Schampera MS, Schweinzer K, Abele H, Kagan KO, Klein R, Rettig I, Jahn G, Hamprecht K (2017) Comparison of cytomegalovirus (CMV)-specific neutralization capacity of hyperimmunoglobulin (HIG) versus standard intravenous immunoglobulin (IVIG) preparations: impact of CMV IgG normalization. J Clin Virol 90:40–45
Planitzer CB, Saemann MD, Gajek H, Farcet MR, Kreil TR (2011) Cytomegalovirus neutralization by hyperimmune and standard intravenous immunoglobulin preparations. Transplantation 92(3):267–270. https://doi.org/10.1097/TP.0b013e318224115e
Gupta CK, Leszczynski J, Gupta RK et al (1996) IgG subclass antibodies to human cytomegalovirus (CMV) in normal human plasma samples and immune globulins and their neutralizing activities. Biologicals 24:117
Saccoccio FM, Sauer AL, Cui X, Armstrong AE, Habib el-SE, Johnson DC, Ryckman BJ, Klingelhutz AJ, Adler SP, McVoy MA (2011) Peptides from cytomegalovirus UL130 and UL131 proteins induce high titer antibodies that block viral entry into mucosal epithelial cells. Vaccine 29(15):2705–2711
Yang X, Yu X (2009) An introduction to epitope prediction methods and software. Rev Med Virol 19(2):77–96
Jespersen MC, Peters B, Nielsen M, Marcatili P (2017) BepiPred-2.0: improving sequence-based B-cell epitope prediction using conformational epitopes. Nucleic Acids Res 45(W1):w24–w29
Yao B, Zhang L, Liang S, Zhang C (2012) SVMTriP: A method to predict antigenic epitopes using support vector machine to integrate tri-peptide similarity and propensity. PLoS One 7(9):e45152
Saha S, Raghava GPS (2004) BcePred: prediction of continuous B-cell epitopes in antigenic sequences using physico-chemical properties, vol 3239. ICARIS, LNCS, Springer, New York, pp 197–204
Zhang Y (2008) I-TASSER server for protein 3D structure prediction. BMC Bioinform 9(1):40
Germer M, Herbener P, Schüttrumpf J (2016) Functional properties of human cytomegalovirus hyperimmunoglobulin and standard immunoglobulin preparations. Ann Transpl 21:558–564
Wang X, Xu Y, Scott DE, Murata H, Struble EB (2017) Binding and neutralizing anti-cytomegalovirus activities in immune globulin products. Biologicals 50:35–41
Chandramouli S, Malito E, Nguyen T, Luisi K, Donnarumma D, Xing Y, Norais N, Yu D, Carfi A (2017) Structural basis for potent antibody-mediated neutralization of human cytomegalovirus. Sci Immunol 2(12):eaan1457
Cui X, Meza BP, Adler SP, McVoy MA (2008) Cytomegalovirus vaccines fail to induce epithelial entry neutralizing antibodies comparable to natural infection. Vaccine 26:5760–5766
Loughney JW, Rustandi RR, Wang D, Troutman MC, Dick LW Jr, Li G, Liu Z, Li F, Freed DC, Price CE, Hoang VM, Culp TD, DePhillips PA, Fu TM, Ha S (2015) Soluble human cytomegalovirus gH/gL/pUL128-131 pentameric complex, but not gH/gL, inhibits viral entry to epithelial cells and presents dominant native neutralizing epitopes. J Biol Chem 290(26):15985–15995
Macagno A, Bernasconi NL, Vanzetta F, Dander E, Sarasini A, Revello MG, Gerna G, Sallusto F, Lanzavecchia A (2010) Isolation of human monoclonal antibodies that potently neutralize human cytomegalovirus infection by targeting different epitopes on the gH/gL/UL128-131A complex. J Virol 84(2):1005–1013
Gerna G, Percivalle E, Perez L, Lanzavecchia A, Lilleri D (2016) Monoclonal antibodies to different components of the human cytomegalovirus (HCMV) pentamer gH/gL/pUL128L and trimer gH/gL/gO as well as antibodies elicited during primary HCMV Infection prevent epithelial cell syncytium formation. J Virol 90(14):6216–6223
Ha S, Li F, Troutman MC, Freed DC, Tang A, Loughney JW, Wang D, Wang I-Ming, Vlasak J, Nickle DC, Rustandi RR, Hamm M, DePhillips PA, Zhang N, McLellan JS, Zhu H, Adler SP, McVoy MA, Zhiqiang AN, Tong-Ming FU (2017) Neutralization of diverse human cytomegalovirus strains conferred by antibodies targeting viral gH/gL/pUL128-131 pentameric complex. J Virol 91(7):JVI-02033
Hofmann I, Wen Y, Ciferri C, Schulze A, Fühner V, Leong M, Gerber A, Gerrein R, Nandi A, Lilja AE, Carfi A, Laux H (2015) Expression of the human cytomegalovirus pentamer complex for vaccine use in a CHO system. Biotechnol Bioeng 112(12):2505–2515
Hamilton ST, van Zuylen W, Shand A, Scott GM, Naing Z, Hall B, Craig ME, Rawlinson WD (2014) Prevention of congenital cytomegalovirus complications by maternal and neonatal treatments: a systematic review. Rev Med Virol. (6):420–433
Hamprecht K, Kagan KO, Goelz R (2014) Comment on: a randomized trial of hyperimmune globulin to prevent congenital cytomegalovirus. N Engl J Med 370(26):2543
Gerna G, Revello MG, Baldanti F, Percivalle E, Lilleri D (2017) The pentameric complex of human Cytomegalovirus: cell tropism, virus dissemination, immune response and vaccine development. J Gen Virol 98(9):2215–2234
Acknowledgements
MS received a Grant from Biotest AG, Preclinical Research (Dr. M Germer). Cytotect® was provided from Biotest AG. We thank Wioleta Kapis for her excellent technical assistance and for providing sera from the Tuebingen congenital CMV study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
Maternal sera at birth were derived from the Tuebingen congenital CMV study, approved by our local Ethics Committee at the University Hospital of Tuebingen; EK number 506/2015BO2. Each mother enrolled in the cCMV study was informed about the study design and has given signed permission using her serum for CMV serology.
Electronic supplementary material
Below is the link to the electronic supplementary material.
430_2018_558_MOESM1_ESM.pptx
Supplemental Material Figure 1: Prediction of the epitopes through bioinformatics analysis by the use of two computer servers (A and B). The epitope was selected from position 33 to 51 with optimal physical chemical properties (C). Supplemental Material Figure 2: Structural similarities were observed, comparing our predicted 3D model and a previously reported crystalized model [36] (PPTX 434 KB)
Rights and permissions
About this article
Cite this article
Schampera, M.S., Arellano-Galindo, J., Kagan, K.O. et al. Role of pentamer complex-specific and IgG subclass 3 antibodies in HCMV hyperimmunoglobulin and standard intravenous IgG preparations. Med Microbiol Immunol 208, 69–80 (2019). https://doi.org/10.1007/s00430-018-0558-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-018-0558-x