Abstract
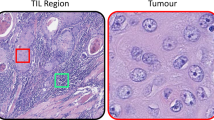
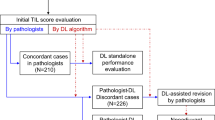
Stromal tumour infiltrating lymphocytes (sTIL) in haematoxylin and eosin (H&E) stained sections has been linked to better outcomes and better responses to neoadjuvant therapy in triple-negative and HER2-positive breast cancer (TNBC and HER2 +). However, the infiltrate includes different cell populations that have specific roles in the tumour immune microenvironment. Various studies have found high concordance between sTIL visual quantification and computational assessment, but specific data on the individual prognostic impact of plasma cells or lymphocytes within sTIL on patient prognosis is still unknown. In this study, we validated a deep-learning breast cancer sTIL scoring model (smsTIL) based on the segmentation of tumour cells, benign ductal cells, lymphocytes, plasma cells, necrosis, and ‘other’ cells in whole slide images (WSI). Focusing on HER2 + and TNBC patient samples, we assessed the concordance between sTIL visual scoring and the smsTIL in 130 WSI. Furthermore, we analysed 175 WSI to correlate smsTIL with clinical data and patient outcomes. We found a high correlation between sTIL values scored visually and semi-automatically (R = 0.76; P = 2.2e-16). Patients with higher smsTIL had better overall survival (OS) in TNBC (P = 0.0021). In the TNBC cohort, smsTIL was as an independent prognostic factor for OS. As part of this work, we introduce a new segmentation dataset of H&E-stained WSI.





Similar content being viewed by others

Data availability
Data on anonymized tiles and ground truth segmentations of breast cancer whole slide image sections have been deposited into the open-source database Zenodo (10.5281/zenodo.7775365).
References
Hammerl D, Smid M, Timmermans AM, Sleijfer S, Martens JWM, Debets R (2018) Breast cancer genomics and immuno-oncological markers to guide immune therapies. Semin Cancer Biol 52:178–188. https://doi.org/10.1016/J.SEMCANCER.2017.11.003
Denkert C et al (2018) Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol 19(1):40–50. https://doi.org/10.1016/S1470-2045(17)30904-X
Loi S et al (2013) Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02–98. J Clin Oncol 31(7):860–867. https://doi.org/10.1200/JCO.2011.41.0902
Salgado R et al (2015) The evaluation of tumor-infiltrating lymphocytes (TILS) in breast cancer: recommendations by an International TILS Working Group 2014. Ann Oncol 26(2):259–271. https://doi.org/10.1093/annonc/mdu450. (Oxford University Press)
Mohaiminul Islam M, Huang S, Ajwad R, Chi C, Wang Y, Hu P (2020) An integrative deep learning framework for classifying molecular subtypes of breast cancer. Comput Struct Biotechnol J 18:2185–2199. https://doi.org/10.1016/j.csbj.2020.08.005
Bychkov D et al (2021) Deep learning identifies morphological features in breast cancer predictive of cancer ERBB2 status and trastuzumab treatment efficacy. Sci Rep 11(1). https://doi.org/10.1038/s41598-021-83102-6
Beck AH et al (2011) Systematic analysis of breast cancer morphology uncovers stromal features associated with survival. Sci Transl Med 3(108):108–113. https://doi.org/10.1126/scitranslmed.3002564
Sarah Dudgeon AN, Wen S, Gallas BD A Pathologist-Annotated Dataset for Validating Artificial Intelligence: A Project Description and Pilot Study Title A Pathologist-Annotated Dataset for Validating Artificial Intelligence: A Project Description and Pilot Study Affiliations of Authors. iRhythm Technologies Inc
Saltz J et al (2018) Spatial organization and molecular correlation of tumor-infiltrating lymphocytes using deep learning on pathology images. Cell Rep 23(1):181-193.e7. https://doi.org/10.1016/j.celrep.2018.03.086
Thagaard J et al (2021) Automated quantification of stil density with h&e-based digital image analysis has prognostic potential in triple-negative breast cancers. Cancers (Basel) 13(12). https://doi.org/10.3390/cancers13123050
Bai Y et al (2021) An open-source, automated tumor-infiltrating lymphocyte algorithm for prognosis in triple-negative breast cancer. Clin Cancer Res 27(20):5557–5565. https://doi.org/10.1158/1078-0432.CCR-21-0325
Olkhanud PB et al (2011) Tumor-evoked regulatory B cells promote breast cancer metastasis by converting resting CD4+ T cells to T-regulatory cells. Cancer Res 71(10):3505–3515. https://doi.org/10.1158/0008-5472.CAN-10-4316
Tower H, Ruppert M, Britt K (2019) The immune microenvironment of breast cancer progression. Cancers (Basel) 11(9):1–15. https://doi.org/10.3390/cancers11091375
Ali HR et al (2014) Association between CD8+ T-cell infiltration and breast cancer survival in 12 439 patients. Ann Oncol 25(8):1536–1543. https://doi.org/10.1093/annonc/mdu191
Wang K, Shen T, Siegal GP, Wei S (2017) The CD4/CD8 ratio of tumor-infiltrating lymphocytes at the tumor-host interface has prognostic value in triple-negative breast cancer. Hum Pathol 69:110–117. https://doi.org/10.1016/j.humpath.2017.09.012
Garaud S et al (2019) Tumor-infiltrating B cells signal functional humoral immune responses in breast cancer. JCI Insight 4(18). https://doi.org/10.1172/jci.insight.129641
Mohammed ZMA, Going JJ, Edwards J, Mcmillan DC (2013) The relationship between lymphocyte subsets and clinico-pathological determinants of survival in patients with primary operable invasive ductal breast cancer. Br J Cancer 109(6):1676–1684. https://doi.org/10.1038/bjc.2013.493
Wei H, Fu P, Yao M, Chen Y, Du L (2016) Breast cancer stem cells phenotype and plasma cell-predominant breast cancer independently indicate poor survival. Undefined 212(4):294–301. https://doi.org/10.1016/J.PRP.2016.01.008
bin Seow DY et al (2020) Tertiary lymphoid structures and associated plasma cells play an important role in the biology of triple-negative breast cancers. Breast Cancer Res Treat 180(2):369–377. https://doi.org/10.1007/S10549-020-05548-Y
Kuroda H et al (2021) Prognostic value of tumor-infiltrating B lymphocytes and plasma cells in triple-negative breast cancer. Breast Cancer 28(4):904–914. https://doi.org/10.1007/s12282-021-01227-y
Yeong J et al (2018) High densities of tumor-associated plasma cells predict improved prognosis in triple negative breast cancer. Front Immunol 9(MAY). https://doi.org/10.3389/fimmu.2018.01209
Li JJ, Tsang JY, Tse GM (2021) Tumor microenvironment in breast cancer—Updates on therapeutic implications and pathologic assessment. Cancers 13(16). https://doi.org/10.3390/cancers13164233. (MDPI)
Moncusí A, Villanueva X, Noguera A, Bonilla M, Posso M, Macià F (2022) Informe 2022 del Registre de Tumors de l’Hospital del Mar (RTHMar), Barcelona. Barcelona: Parc de Salut MAR; 2022. Barcelonas
Allison KH et al (2020) Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol 38:1346–1366. https://doi.org/10.1200/JCO.19
Wolff AC et al (2018) Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline focused update. J Clin Oncol 36:2105–2122. https://doi.org/10.1200/JCO
Bankhead P et al (2017) QuPath: open source software for digital pathology image analysis. Sci Rep 7(1). https://doi.org/10.1038/s41598-017-17204-5
Graham S et al (2019) Hover-Net: Simultaneous segmentation and classification of nuclei in multi-tissue histology images. Med Image Anal 58:101563. https://doi.org/10.1016/J.MEDIA.2019.101563
Dang VuQ et al (2019) Methods for segmentation and classification of digital microscopy tissue images. Front Bioeng Biotechnol 7:53. https://doi.org/10.3389/fbioe.2019.00053
Hendry S et al (2017) Assessing tumor-infiltrating lymphocytes in solid tumors: a practical review for pathologists and proposal for a standardized method from the international immuno-oncology biomarkers working group: part 2: TILs in melanoma, gastrointestinal tract carcinomas, non-small cell lung carcinoma and mesothelioma, endometrial and ovarian carcinomas, squamous cell carcinoma of the head and neck, genitourinary carcinomas, and primary brain tumors. Adv Anat Pathol 24(6):311–335. https://doi.org/10.1097/PAP.0000000000000161. (Lippincott Williams and Wilkins)
AiErken NJ et al (2017) High PD-L1 expression is closely associated with tumor-infiltrating lymphocytes and leads to good clinical outcomes in Chinese triple negative breast cancer patients. Int J Biol Sci 13(9):1172–1179. https://doi.org/10.7150/ijbs.20868
Schoenfeld D (1981) The asymptotic properties of nonparametric tests for comparing survival distributions. Biometrika 68(1):316–319. https://doi.org/10.2307/2335833
Schoenfeld DA (1983) Sample-size formula for the proportional-hazards regression model. Biometrics 39(2):499–503. https://doi.org/10.2307/2531021
Jang N, Kwon HJ, Park MH, Kang SH, Bae YK (2018) Prognostic value of tumor-infiltrating lymphocyte density assessed using a standardized method based on molecular subtypes and adjuvant chemotherapy in invasive breast cancer. Ann Surg Oncol 25(4):937–946. https://doi.org/10.1245/s10434-017-6332-2
Acknowledgements
The authors would like to acknowledge Xavier Duran for his statistical guidance.
Funding
This research was funded by Rio Hortega post-residency grant, Instituto de Salud Carlos III CM20/00019 and supported by grants from Instituto de Salud Carlos III/FEDER (PT17/0015/0011) and the ‘Xarxa de Bancs de tumors’ sponsored by Pla Director d’Oncologia de Catalunya (XBTC).
Author information
Authors and Affiliations
Contributions
Conceptualization: MG, JG, LC and IV. Methodology: MG, JG, PS, JS, PG, JM, LC and IV. Formal analysis and investigation: MG, JG, LC and IV. Writing-original draft preparation: MG and JG. Writing-review and editing: LC, IV, BB, BL and JA. Funding acquisition: MG, LC and JA.
Corresponding author
Ethics declarations
This study was approved by the Ethics Commission of Hospital del Mar (2020/794537/I). Biological samples were obtained from ‘Parc de Salut MAR Biobank (MARBiobanc)’(Barcelona).
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonzàlez-Farré, M., Gibert, J., Santiago-Díaz, P. et al. Automated quantification of stromal tumour infiltrating lymphocytes is associated with prognosis in breast cancer. Virchows Arch 483, 655–663 (2023). https://doi.org/10.1007/s00428-023-03608-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-023-03608-4