Abstract
The use of adjuvant radiotherapy is controversial for atypical meningiomas undergoing gross total resection. It has recently been proposed that meningiomas may be classified into four molecular groups (MG): immunogenic (MG1), benign NF2-wildtype (MG2), hypermetabolic (MG3), and proliferative (MG4). The two latter have the worst prognosis, and it has been suggested that they can be identified using ACADL and MCM2 immunostainings. We studied 55 primary atypical meningiomas, treated with gross total resection and no adjuvant therapies, to assess whether ACADL and MCM2 immuno-expression may identify patients at higher recurrence risk, thus requiring adjuvant treatments. Twelve cases resulted ACADL-/MCM2-, 9 ACADL + /MCM2-, 17 ACADL + /MCM2 + , and 17 ACADL-/MCM2 + . MCM2 + meningiomas displayed more frequent atypical features (prominent nucleoli, small cells with high nuclear-to-cytoplasmic ratio) and CDKN2A hemizygous deletion (HeDe) (P = 0.011). The immunoexpression of ACADL and/or MCM2 was significantly associated with higher mitotic index, 1p and 18q deletions, increased recurrence rate (P = 0.0006), and shorter recurrence-free survival (RFS) (P = 0.032). At multivariate analysis, carried out including ACADL/MCM2 immuno-expression, mitotic index, and CDKN2A HeDe as covariates, this latter resulted a significant and independent prognosticator of shorter RFS (P = 0.0003).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meningiomas account for approximately 40% of all primary tumors in the central nervous system [1]. According to the World Health Organization (WHO), they are classified into 15 histological subtypes and three grades of malignancy [2]. The three-tiered grading system of meningiomas (CNS WHO grade) is mainly based on histopathological features [3]; however, CDKN2A/B homozygous deletion and TERT promoter (pTERT) mutation have been recently added as diagnostic criteria for CNS WHO grade 3 meningiomas because of their negative prognostic significance [2]. Owing to its significant correlation with disease recurrence, the CNS WHO grade of meningiomas is included in the flowcharts guiding the post-surgical treatment of these tumors. Indeed, wait and observation is indicated for patients with grade 1 meningiomas, whereas radiotherapy is indicated for patients with grade 3 meningiomas [4]. Patients with subtotal or partial resection of grade 2 meningiomas are invariably treated with adjuvant radiotherapy, whereas the post-surgical treatment of grade 2 meningiomas that underwent gross total resection is still controversial, and either radiotherapy or observation is suggested [4].
CNS WHO grade 2 meningiomas include three histological subtypes: (i) chordoid; (ii) clear cell; and (iii) atypical [2]. This latter is by far the most frequent and its diagnosis relates on the following histological features: (i) presence of 4–19 mitoses in an area of 1.6 mm2; and/or (ii) brain invasion; and/or (iii) at least three minor criteria among spontaneous necrosis, pattern-less architecture (sheeting), small cells with high nuclear/cytoplasmic ratio, prominent nucleoli, and hypercellularity [2]. Atypical meningiomas have a 5-year recurrence rate of approximately 50% [5]. The wide range of histological diagnostic criteria likely accounts for their heterogeneous clinical outcome. Therefore, additional factors able to stratify atypical meningiomas based on their recurrence risk would be useful to distinguish high-risk patients who could benefit from adjuvant therapy and to spare low-risk patients from adverse effects.
Recently, several studies have demonstrated that epigenetic and cytogenetic features may predict the recurrence-free survival (RFS) in patients with meningiomas [6,7,8]. However, these molecular assays may not be accessible to all centers because of their high costs and long turn-around time. Using a discovery cohort of 121 meningiomas (59 grade 1, 43 grade 2, and 19 grade 3) and a validation cohort of 80 meningiomas (23 grade 1, 55 grade 2, and 2 grade 3), a recent study distinguished four consensus molecular groups by the combination of DNA somatic copy-number aberrations, DNA somatic point mutations, DNA methylation, and messenger RNA abundance [9]. Each molecular group had distinctive features: immunogenic (MG1), benign NF2-wildtype (MG2), hypermetabolic (MG3), and proliferative (MG4) [9]. Stratification by molecular groups correlated with RFS, independently of the extent of resection, CNS WHO grade or radiotherapy, and predicted recurrence risk more accurately than CNS WHO grade and the previously described methylation-based classifications [10]. In detail, MG3 and MG4 were associated with the shortest RFS, whereas meningiomas in the MG1 group had the longest RFS [9]. Proteomic characterization showed that the different molecular groups were enriched in different proteins, namely, MG1 in S100A, MG2 in SCGN, MG3 in ACADL, and MG4 in MCM2; a subgroup analysis of 44 cases suggested that the molecular group could be predicted using immunostainings for these proteins [9]. However, the correlation between the immuno-expression of these proteins and the clinical-pathological features or recurrence probability of meningiomas remains to be analyzed.
In this study, we investigated whether the immuno-expression of ACADL and MCM2, used as surrogates of molecular groups MGM3 and MGM4, is associated with reduced RFS or with clinical, pathological and genetic features in a cohort of 55 atypical meningiomas treated with surgery and no radiotherapy.
Materials and methods
Cases
Fifty-five primary atypical meningiomas surgically resected from adult patients (age ≥ 18 years) between 2003 and 2018 were included in this study. The inclusion criteria were as follows: (1) atypical meningioma subtype according to WHO 2021 criteria [2]; (2) complete surgical resection (corresponding to Simpson grades 1–3 [11]); (3) no history of neurofibromatosis; (4) available information on RFS; (5) at least 24 months of follow-up for non-recurring tumors; and (6) availability of paraffin blocks.
Ethical issues
This study was approved by Comitato Etico per la Sperimentazione Clinica delle province di Verona e Rovigo (protocol n. 40,400, 2019/07/19).
Histological revision
We reviewed the histological slides of all cases to assess the number of mitoses per 1.6 mm2, brain invasion, hypercellularity, prominent nucleoli, small cells with a high nuclear-to-cytoplasmic ratio, spontaneous necrosis, and sheeting, as previously described [5, 12, 13].
Clinical data
Information on tumor localization, extent of surgical resection, and RFS was retrieved from the clinical records and operatory registries.
Meningiomas were subdivided into three groups according to their localization: (1) meningiomas of the convexity; (2) parasagittal/tentorium; and (3) skull base.
Immunohistochemistry
All cases were immunostained using antibodies against MCM2 (clone 1E7, dilution 1:200, Cell Signaling Technology) and ACADL (polyclonal, dilution 1: 200, Sigma).
In each case, we assessed the percentage of neoplastic cells that were positive for MCM2 and ACADL. Cases were classified as positive when > 5% of stained cells were observed.
Then, meningiomas were subdivided into three groups according to MCM2 and ACADL positivity: (i) immunohistochemical group1 (IHC-G1), including cases negative for both ACADL and MCM2 (corresponding to MG1 and MG2); (ii) IHC-G2, composed of cases positive for only ACADL (corresponding to MG3); and (iii) IHC-G3, comprising cases positive for MCM2 and either positive or negative for ACAL (corresponding to MG4).
CDKN2A copy number variations
CDKN2A copy number variations were assessed using NGS (see below) in 15 meningiomas (cases 12–26) and FISH and LSI CDKN2A/CEP 9 probes (Vysis/Abbott, Molecular Europe, Wiesbaden, Germany) in 40. In detail, slides were examined using an Olympus BX61 fluorescence microscope equipped with a 100 × oil immersion objective and a triple band pass filter for simultaneous detection of Spectrum Orange, Spectrum Green, and DAPI signals. We counted 200 non-overlapping nuclei containing a minimum of 2 reference probe (CEP 9 probe) signals. CDKN2A homozygous deletion was defined as the presence of two green signals (control probe on chromosome 9 centromeres) and no orange signals (reference probe on CDKN2A locus) in at least 30% of cells.
Next generation sequencing
In 15 meningiomas (cases 12–26), mutations and CNV in 409 genes (including CDKN2A/B) were previously analyzed using the Oncomine Tumor Mutational Load (TML) assay (Thermo Fisher), which covers 1.65 Mb of genomic space [8].
Integrated molecular grading
The integrated molecular grading system proposed by Driver et al. [6] was applied to fifteen meningiomas analyzed by NGS. This is a grading system combining genetic alterations and mitotic index. In detail, one point is assigned to the presence of each genetic alteration among 1p, 3p, 4p/q, 6p/q, 10p/q, 14q, 18p/q and 19p/q deletion, and CDKN2A/B homozygous or heterozygous deletion; one point is assigned to mitotic index of 4–19 mitoses/1.6 mm2, whereas two points are assigned to mitotic index of ≥ 20 mitoses/1.6 mm2 [6]. Meningiomas with 0–1 point are classified as integrated grade 1, meningiomas with 2–3 points as integrated grade 2, and meningiomas with ≥ 4 points as integrated grade 3 [6].
Statistical analyses
We used the Chi-squared test to analyze the correlations between the immunohistochemical group and the various clinico-pathological parameters (age and sex of the patients, localization, brain invasion, sheeting, hypercellularity, prominent nucleoli, spontaneous necrosis, small cells with high nuclear/cytoplasmic ratio of the tumors) or genetic features (i.e., gene mutations or CNV, chromosomal gains or losses). The Kruskal–Wallis test was used to assess whether the mitotic index differed according to the immunohistochemical group.
Finally, RFS was assessed using the Kaplan–Meier method, with the date of primary surgery as the entry data and length of survival to the detection of a recurrent tumor as the end point. The Mantel-Cox log-rank test was applied to assess the strength of association between mitotic index, brain invasion, immunohistochemical group, CDKN2A/B copy number, and RFS.
A probability (P) value less than 0.05 was considered significant. Statistical analysis was performed using the MedCalc 12.1.4.0 statistical software (MedCalc Software, Mariakerke, Belgium).
Results
Clinical features
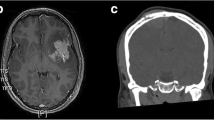
This study included 55 meningiomas that were surgically resected in 30 male and 25 female patients (mean age: 60 ± 13 years), with extent of surgical resection corresponding to Simpson grade 1 in 33 cases, grade 2 in 14 cases, and grade 3 in 8 (Fig. 1). Twenty-one meningiomas were located at the brain convexity, 20 were parasagittal/tentorial, and 14 were at the skull base.
Thirty-seven patients had tumor recurrence during follow-up, with an RFS length ranging between 4 and 151 months (median, 41 months). The follow-up time ranged from 32 to 105 months (median, 52 months) in patients without disease recurrence.
Histopathological features, TERT promoter mutation, and CDKN2A copy number variations
Histologically, meningiomas were classified as atypical because of the following: (i) a mitotic index ≥ 4/1.6 mm2, in 35 cases; (ii) presence of brain invasion, in the absence of a high mitotic index, in 17 cases; and (iii) presence of only minor atypical criteria, in 3 cases (Fig. 1). In accordance with the inclusion criteria, none had CDKN2A homozygous deletion or TERT promoter mutations.
Fifteen cases had CDKN2A heterozygous deletion (HeDe) (Fig. 1).
Mitotic index was higher in meningiomas IHC-G2 (ACADL +) and IHC-G3 (MCM2 +)
Twelve meningiomas were classified as IHC-G1 (MCM2-/ACADL-) (Fig. 1).
All cases positive for ACADL and/or MCM2 had ≥ 20% stained cells, whereas none showed a percentage of stained cells between 5 and 20%.
Nine tumors with ACADL positivity in 20–60% of cells and lacking MCM2 immunostaining were IHC-G2 (MCM2-/ACADL +) (Fig. 2). Finally, 34 meningiomas, showing MCM2 immunostaining in 20–90% cells, were IHC-G3 (MCM2 +) (Fig. 3); 17 of these cases had concurrent ACADL immunostaining in 10–80% tumor cells.
Tumors IHC-G3 (MCM2 +) were more frequently characterized by prominent nucleoli (77% vs 64% in IHC-G2 and 33% in IHC-G1) (P = 0.0449) and by small cells with high nuclear/cytoplasmic ratio (66% vs. 42% and 11%) (P = 0.0129) (Table 1). Atypical meningiomas IHC-G2 and IHC-G3 had a significantly higher mitotic index than IHC-G1 (P = 0.029).
1p and 18q deletion were more frequent in meningiomas IHC-G2 (ACADL +) and IHC-G3 (MCM2 +)
NGS analysis was carried out on 15 atypical meningiomas, including 4 IHCG1, 3 IHCG2, and 8 HCG3. Six cases had NF2 mutations (1/4 IHC-G1, 2/3 IHC-G2, and 3/8 ICH-G3) and two harbored AKT1 E17K mutation (1 IHC-G1 and in 1 IHC-G3) (Fig. 1).
The deletion of 1p (P = 0.0239), 10q, 14q, or 18q (P = 0.0125) was exclusive to ICH-G2 and ICH-G3 (Fig. 1).
CDKN2A hemizygous deletion was more frequent in atypical meningiomas IHC-G3 (MCM2 +)
CDKN2A HeDe was present in 14 meningiomas ICH-G3, in one meningioma IHC-G2 and absent in all meningiomas IHC-G1 (P = 0.0462).
Integrated molecular grade correlates with MCM2 and ACADL immunostaining
All four meningiomas lacking MCM2 and ACADL immunostaining (IHC-G1) were classified as integrated grade 1; all three meningiomas in IHC-G2 (ACADL + /MCM2-) were classified as integrated grade 3, whereas 5/8 tumors in IHC-G3 (MCM2 +) were classified as integrated grade 2 or 3 (P = 0.0166).
Immunostaining for ACADL or MCM2 was significantly associated with tumor recurrence and shorter RFS
Three of 12 (25%) meningiomas IHC-G1, 9/9 (100%) IHC-G2, and 25/34 (74%) IHC-G3 recurred (P = 0.0006) (Table 1). RFS was significantly shorter in patients with meningiomas IHC-G2 or IHC-G3 (hazard ratio, 2.3; 95% confidence interval, 1–5.1; P = 0.032) (Fig. 4) or having mitotic index ≥ 4/1.6 mm2 (hazard ratio, 2.8; 95% confidence interval, 1.4–5.5; P = 0.0026) or harboring CDKN2A HeDe (hazard ratio, 5; 95% confidence interval, 2.1–12.1; P = 0.0003) (Fig. 4).
Kaplan–Meier curves showing RFS of 55 patients with atypical meningioma according to IHC group and CDKN2A copy number variation. A The RFS of patients with atypical meningioma IHC group 2 (ACADL + /MCM2-) and IHC group 3 (MCM2 +) was significantly shorter than that of patients with atypical meningiomas IHC group 1 (ACADL-/MCM2-). B The RFS of patients with atypical meningioma harboring CDKN2A hemizygous deletion (HeDe) was significantly shorter than that of patients with atypical meningiomas having disomic CDKN2A
Multivariate analysis (Cox regression model) was used to determine the independent effect of the IHC group, high mitotic index (≥ 4/1.6 mmq) and CDKN2A HeDe on RFS. A low mitotic index (< 4/1.6 mm2) was independently associated with longer RFS (hazard ratio, 0.3; 95% confidence interval, 0.1–0.7; P = 0.0082), and CDKN2A HeDe was independently associated with shorter RFS (hazard ratio, 3.3; 95% confidence interval, 1.5–6.9; P = 0.0015), whereas IHC group had no independent effect on patients RFS.
Discussion
The treatment of patients with atypical meningiomas after gross total resection is largely debated, owing to controversial results in studies investigating the benefit of adjuvant radiotherapy in ameliorating their RFS. Controversial findings may be due to the biological heterogeneity of atypical meningiomas, which include indolent and aggressive tumors.
Nassiri et al. recently suggested that meningiomas could be classified into molecular groups, which may reflect their biological and clinical aggressiveness better than WHO histological subtypes [9]. In their cohort of 121 tumors, molecular groups were prognostically relevant even in the subgroup of 43 meningiomas classified as grade 2 according to the 2016 WHO criteria [3], with MG3 and MG4 cases having the shortest RFS (P = 0.037) [9]. MG3 and MG4 may be recognized using immunohistochemistry against ACADL and MCM2 [9], but whether these immunostainings may be useful to identify meningiomas with a higher recurrence risk has not been investigated.
In this study, we analyzed for the first time whether ACADL and MCM2 immunostainings, used as surrogates to determine molecular groups MG3 and MG4, could predict the recurrence risk of atypical meningiomas and to identify cases which could benefit from adjuvant treatments in clinical practice. In a cohort of 55 primary meningiomas, classified atypical according to the 2021 WHO criteria, and that underwent complete surgical resection and no adjuvant radiotherapy, immunostaining for MCM2 or ACADL in ≥ 20% tumor cells was significantly associated with recurrence and with shorter RFS, without any significant difference between tumors showing only ACADL immunostaining (corresponding to MG3) or both ACADL and MCM2 positivity (equating to MG4). These findings suggest that in routine practice atypical meningiomas can be stratified according to recurrence risk using MCM2 and ACADL immunostainings.
In accordance with the reported frequent inactivation of tumor suppressor genes in MG4 and MG3 [9], atypical meningiomas with MCM2 or ACADL immunostaining had higher mitotic counts, reflecting a high proliferative activity. In addition, they had chromosomal instability and were enriched in multiple chromosomal deletions previously associated with a higher risk of meningioma recurrence [6, 8, 14,15,16,17]. This finding is in line with the high aneuploidy found in MG3 and MG4 meningiomas, which harbor frequent losses in chromosomes 22q, 1p, 6q, 14, and 18 [9], whereas these alterations are infrequent in meningiomas of other molecular groups.
Driver et al. recently proposed a three-tiered integrated molecular grading of meningiomas based on the presence of several chromosomal deletions (1p, 3p, 4p/q, 6p/q, 10p/q, 14q, 18p/q, and 19p/q), CDKN2A/B deletion, and mitotic count [6]. In 527 meningiomas, they demonstrated that the overall correlation between CNS WHO and molecular integrated grading was good; however, within CNS WHO grade 2 meningiomas, the concordance with integrated grades was of only 31%, reflecting the high molecular heterogeneity of these tumors [6]. Indeed, CNS WHO grade 2 meningiomas resolved into integrated grade 1 in one-third and into integrated grade 3 in another third [6]. Although integrated molecular grading outperformed CNS WHO grading in predicting recurrence and it nicely stratified CNS WHO grade 2 meningiomas for their recurrence risk [6], its application in routine practice is limited by the high costs. In this study, we applied the integrated molecular grading to 15 atypical meningiomas (CNS WHO grade 2) according to the 2021 WHO criteria. Owing to the higher frequency of chromosomal deletions in cases with MCM2 or ACADL immunostaining, the immunohistochemical group and integrated grade were significantly correlated. Indeed, all four cases classified as integrated grade 1 lacked MCM2 or ACADL immunostaining. Therefore, these findings suggest that MCM2 and/or ACADL immunostaining may be used to identify meningiomas with high chromosomal instability and consequently a high integrated grade.
In this study, we assessed CDKN2A copy number variations as a requisite to exclude CNS WHO grade 3 meningioma [2]. Fifteen tumors, all positive for MCM2 or ACADL, had CDKN2A HeDe. Although CDKN2A HeDe is not currently considered as a criterion for upgrading meningiomas to CNS WHO grade 3, it was recently suggested to predict shorter RFS in patients with meningiomas [18]. Indeed, in a heterogeneous cohort of 659 meningiomas, including primary and recurrent tumors, of all three CNS WHO grades, and with either total or subtotal surgical resection, CDKN2A/B HeDe was found in 15 cases in association with shorter progression-free survival [18]. Our findings, obtained in a cohort of only primary atypical meningiomas that underwent total resection, further support the negative prognostic significance of CDKN2A HeDe in meningiomas. Indeed, this was significantly associated with unfavorable IHC groups (MCM2 + and ACADL +) and with shorter RFS, independently of these latter.
In conclusion, this is the first study to show that immunostainings for MCM2 and ACADL may be useful for identifying atypical meningiomas characterized by higher genomic instability, CDKN2A HeDe, higher integrated molecular grade, recurrence risk, and shorter RFS. A limitation of this study was the number of cases, although it should be emphasized that we included only primary meningiomas that underwent gross total resection. Despite the correlation with pathological and genetic features reflecting higher biological aggressiveness, MCM2/ACADL immuno-expression was not an independent prognostic factor at the multivariate RFS analysis including mitotic index and CDKN2A HeDe.
Data availability
Data will be available upon request to corresponding author,
References
Ostrom QT, Price M, Neff C, Cioffi G, Waite KA, Kruchko C, Barnholtz-Sloan JS (2022) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2015–2019. Neuro Oncol 24:v1–v95. https://doi.org/10.1093/neuonc/noac202
Sahm F, Perry A, von Deimling A, Claus EB, Mawrin C, Brastianos PK, Santagata S (2021) Meningiomas. In: Brat D, J.,, Ellison DW, Figarella-Branger D, Hawkins C, Louis DN, Ng HK, Perry A, Pfister SM, Refeinberger G, Soffietti R, von Deimling A, Wesseling P (eds) WHO classification of tumours editorial board central nervous system tumours International Agency for Research on Cancer Lyon
Louis DN, Ohgaki H, Wisteler OD, Cavenee WK, Ellison DW, Figarella-Branger D, Perry A, Refeinberger G, von Deimling A (2016) WHO Classification of tumors of the central nervous system IARC Lyon
Goldbrunner R, Stavrinou P, Jenkinson MD, Sahm F, Mawrin C, Weber DC, Preusser M, Minniti G, Lund-Johansen M, Lefranc F, Houdart E, Sallabanda K, Le Rhun E, Nieuwenhuizen D, Tabatabai G, Soffietti R, Weller M (2021) EANO guideline on the diagnosis and management of meningiomas. Neuro Oncol 23:1821–1834. https://doi.org/10.1093/neuonc/noab150
Fioravanzo A, Caffo M, Di Bonaventura R, Gardiman MP, Ghimenton C, Ius T, Maffeis V, Martini M, Nicolato A, Pallini R, Pegolo E, Pinna G, Sala F, Skrap M, Volpin V, Barresi V (2020) A risk score based on 5 clinico-pathological variables predicts recurrence of atypical meningiomas. J Neuropathol Exp Neurol 79:500–507. https://doi.org/10.1093/jnen/nlaa018
Driver J, Hoffman SE, Tavakol S, Woodward E, Maury EA, Bhave V, Greenwald NF, Nassiri F, Aldape K, Zadeh G, Choudhury A, Vasudevan HN, Magill ST, Raleigh DR, Abedalthagafi M, Aizer AA, Alexander BM, Ligon KL, Reardon DA, Wen PY, Al-Mefty O, Ligon AH, Dubuc AM, Beroukhim R, Claus EB, Dunn IF, Santagata S, Linda Bi W (2022) A molecularly integrated grade for meningioma. Neuro Oncol 24:796–808. https://doi.org/10.1093/neuonc/noab213
Hielscher T, Sill M, Sievers P, Stichel D, Brandner S, Jones DTW, von Deimling A, Sahm F, Maas SLN (2022) Clinical implementation of integrated molecular-morphologic risk prediction for meningioma Brain Pathol e13132. https://doi.org/10.1111/bpa.13132
Barresi V, Simbolo M, Fioravanzo A, Piredda ML, Caffo M, Ghimenton C, Pinna G, Longhi M, Nicolato A, Scarpa A (2021) Molecular profiling of 22 primary atypical meningiomas shows the prognostic significance of 18q heterozygous loss and CDKN2A/B homozygous deletion on recurrence-free survival Cancers (Basel) 13. https://doi.org/10.3390/cancers13040903
Nassiri F, Liu J, Patil V, Mamatjan Y, Wang JZ, Hugh-White R, Macklin AM, Khan S, Singh O, Karimi S, Corona RI, Liu LY, Chen CY, Chakravarthy A, Wei Q, Mehani B, Suppiah S, Gao A, Workewych AM, Tabatabai G, Boutros PC, Bader GD, de Carvalho DD, Kislinger T, Aldape K, Zadeh G (2021) A clinically applicable integrative molecular classification of meningiomas. Nature 597:119–125. https://doi.org/10.1038/s41586-021-03850-3
Sahm F, Schrimpf D, Stichel D, Jones DTW, Hielscher T, Schefzyk S, Okonechnikov K, Koelsche C, Reuss DE, Capper D, Sturm D, Wirsching HG, Berghoff AS, Baumgarten P, Kratz A, Huang K, Wefers AK, Hovestadt V, Sill M, Ellis HP, Kurian KM, Okuducu AF, Jungk C, Drueschler K, Schick M, Bewerunge-Hudler M, Mawrin C, Seiz-Rosenhagen M, Ketter R, Simon M, Westphal M, Lamszus K, Becker A, Koch A, Schittenhelm J, Rushing EJ, Collins VP, Brehmer S, Chavez L, Platten M, Hanggi D, Unterberg A, Paulus W, Wick W, Pfister SM, Mittelbronn M, Preusser M, Herold-Mende C, Weller M, von Deimling A (2017) DNA methylation-based classification and grading system for meningioma: a multicentre, retrospective analysis. Lancet Oncol 18:682–694. https://doi.org/10.1016/S1470-2045(17)30155-9
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 20:22–39. https://doi.org/10.1136/jnnp.20.1.22
Barresi V, Branca G, Granata F, Alafaci C, Caffo M, Tuccari G (2013) Embolized meningiomas: risk of overgrading and neo-angiogenesis. J Neurooncol 113:207–219. https://doi.org/10.1007/s11060-013-1117-3
Barresi V, Lionti S, Caliri S, Caffo M (2018) Histopathological features to define atypical meningioma: what does really matter for prognosis? Brain Tumor Pathol 35:168–180. https://doi.org/10.1007/s10014-018-0318-z
Aizer AA, Abedalthagafi M, Bi WL, Horvath MC, Arvold ND, Al-Mefty O, Lee EQ, Nayak L, Rinne ML, Norden AD, Reardon DA, Wen PY, Ligon KL, Ligon AH, Beroukhim R, Dunn IF, Santagata S, Alexander BM (2016) A prognostic cytogenetic scoring system to guide the adjuvant management of patients with atypical meningioma. Neuro Oncol 18:269–274. https://doi.org/10.1093/neuonc/nov177
Domingues PH, Sousa P, Otero A, Goncalves JM, Ruiz L, de Oliveira C, Lopes MC, Orfao A, Tabernero MD (2014) Proposal for a new risk stratification classification for meningioma based on patient age, WHO tumor grade, size, localization, and karyotype. Neuro Oncol 16:735–747. https://doi.org/10.1093/neuonc/not325
Olar A, Wani KM, Wilson CD, Zadeh G, DeMonte F, Jones DT, Pfister SM, Sulman EP, Aldape KD (2017) Global epigenetic profiling identifies methylation subgroups associated with recurrence-free survival in meningioma. Acta Neuropathol 133:431–444. https://doi.org/10.1007/s00401-017-1678-x
Patel AJ, Wan YW, Al-Ouran R, Revelli JP, Cardenas MF, Oneissi M, Xi L, Jalali A, Magnotti JF, Muzny DM, Doddapaneni H, Sebastian S, Heck KA, Goodman JC, Gopinath SP, Liu Z, Rao G, Plon SE, Yoshor D, Wheeler DA, Zoghbi HY, Klisch TJ (2019) Molecular profiling predicts meningioma recurrence and reveals loss of DREAM complex repression in aggressive tumors. Proc Natl Acad Sci U S A 116:21715–21726. https://doi.org/10.1073/pnas.1912858116
Khan AB, English CW, Chen WC, Athukuri P, Bayley JCt, Brandt VL, Shetty A, Hadley CC, Choudhury A, Lu HC, Harmanci AO, Harmanci AS, Magill ST, Raleigh DR, Klisch TJ, Patel AJ, (2023) Even heterozygous loss of CDKN2A/B greatly accelerates recurrence in aggressive meningioma. Acta Neuropathol. https://doi.org/10.1007/s00401-023-02543-7
Funding
Open access funding provided by Università degli Studi di Verona within the CRUI-CARE Agreement. This study is supported by FUR 2022, University of Verona, Italy, to VB.
Author information
Authors and Affiliations
Contributions
V.B.: conceptualization; original draft; revision of the histological slides; interpretation of the results; statistical analyses; funding acquisition; reviewing and editing. S.A: revision of histological slides; data collection; interpretation of the results; reviewing and editing. M.S.: molecular analysis; interpretation of the results. S.P.: fluorescent in situ hybridization; interpretation of the results. M.C.: interpretation of the results; reviewing and editing. A.S.: interpretation of the results; reviewing and editing.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Comitato Etico per la Sperimentazione Clinica delle province di Verona e Rovigo (protocol n. 40400, 2019/07/19).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barresi, V., Ammendola, S., Simbolo, M. et al. Atypical meningiomas with an immunohistochemical profile consistent with hypermetabolic or proliferative molecular groups show high mitotic index, chromosomal instability, and higher recurrence risk. Virchows Arch 483, 97–104 (2023). https://doi.org/10.1007/s00428-023-03537-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-023-03537-2