Abstract
The first section of the bone marrow workshop of the European Association of Haematopathology (EAHP) 2020 Virtual Meeting was dedicated to pediatric myeloid neoplasms. The section covered the whole spectrum of myeloid neoplasms, including myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPN), myelodysplastic/myeloproliferative neoplasms (MDS/MPN), and acute myeloid leukemia (AML). The workshop cases are hereby presented, preceded by an introduction on these overall rare diseases in this age group. Very rare entities such as primary myelofibrosis, pediatric MDS with fibrosis, and MDS/MPN with JMML-like features and t(4;17)(q12;q21); FIP1L1::RARA fusion, are described in more detail.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although less common in the pediatric age group, most myeloid neoplasms seen in adults can also occur in childhood where they may show differences from their adult counterparts. Some entities preferentially occur in childhood, such as several types of acute myeloid leukemia (AML) with specific recurrent genetic abnormalities, others exclusively in childhood such as juvenile myelomonocytic leukemia (JMML) and the provisional WHO entity refractory cytopenia of childhood (RCC). Furthermore, when dealing with children and young adults, one must be particularly aware of a possible underlying inherited or de novo germline mutation that might predispose to myeloid neoplasms.
In this paper, we present an overview of the neoplastic cases submitted to the EAHP 2020 bone marrow (BM) workshop on pediatric myeloid neoplasms. The cases were grouped into the following sections: myeloproliferative neoplasms (MPN), JMML and related diseases, myelodysplastic syndromes (MDS), and AML. Each section is preceded by an introduction, focusing on the specific characteristics in childhood, followed at the end by a summary highlighting the lessons learned from the workshop.
Myeloproliferative neoplasms
Chronic myeloid leukemia
Chronic myeloid leukemia (CML) is a BCR::ABL1-positive MPN, characterized by leukocytosis due to proliferation of mainly the granulocytic lineage. CML is rare in childhood, accounting for less than 10% of all CML cases and less than 3% of all pediatric leukemias. The median age at diagnosis in children is 11–12 years, with 60–77% occurring in males [1, 2].
The clinical presentation of CML in childhood is variable, with weakness and abdominal pain being the most common presenting symptoms, and some children being diagnosed incidentally [1, 2]. In comparison with adults, children tend to present with higher white blood cell (WBC) counts [3]. Splenomegaly is common, occurring in > 70%, whereby children tend to have a larger spleen size relative to body size than adults [2,3,4].
Pediatric CML frequently shows high to very high (> 1000 × 109/L) platelet counts, without an increased risk of thrombosis [5]. Mild bleeding signs, however, are observed in 12% of children with thrombocytosis, which does not correlate to elevated platelet counts, but is associated with reduced high molecular weight multimers of von Willebrand factor, indicating an acquired von Willebrand syndrome. The latter resolves after initiation of CML treatment [5].
More than 90% of patients present in chronic phase. The proportion of pediatric patients diagnosed with advanced-stage disease (accelerated phase or blast phase) is, however, higher than that of adult patients [4]. Furthermore, in both children and adults, a molecular response with BCR::ABL1 transcript levels of < 10% at 3 months after starting imatinib is associated with a better progression-free survival [3, 6], but a higher proportion of children fail to achieve this compared with adults (37% versus 24–28%) [3, 6].
CML at the pediatric age shows differences in genomic landscape compared with adult CML. In both children and adults, a hematopoietic stem cell has acquired the BCR::ABL1 fusion gene and breakpoints occur in the same major breakpoint cluster regions (M-BCR) in the BCR gene on chromosome 22, but in chronic-phase CML the breakpoint distribution in BCR has been shown to be different in children [7]. Children show more frequent breakpoints in Alu repeat regions, and unlike adults with CML who have enrichment of fusion sites in the centromeric region, children show enrichment in fusion sites within telomeres overlapping with an Alu repeat region, similar to what is seen in adult Philadelphia-positive acute lymphoblastic leukemia with M-BCR rearrangement [4]. Additionally, transcriptomic analysis has demonstrated differentially expressed genes and pathways in childhood CML when compared to CML in adulthood [8].
Current prognostic scores used for adult patients (including the EUTOS, Hasford, and Sokal scores) are not validated in children. An attempt at validating these scoring systems showed a high discordance rate, confirming they cannot be applied to our youngest patients [4]. The recently proposed EUTOS Long-Term Survival score, which looks at age, spleen size below the costal margin, peripheral blast count, and platelet count, has been evaluated in 350 children and showed good differentiation of progression-free survival [9].
Workshop cases
Four CML cases in chronic phase were submitted to the workshop (Table 1), of which three were girls (aged 17, 16, and 10 years) and one was a boy (3 years old). All showed the typical BM morphology of chronic-phase CML. Three presented with leukocytosis (WBC up to 521.1 × 109/L), but one (case 730, the 16-year-old girl) showed a normal WBC of 5.6 × 109/L and macrocytic anemia. Her karyotype {46,XX,t(9;22;1;6)(q34;q11.2;p12;q27), t(6;22)(p12;q12),der(9)t(5;9)(q13;q22)[10]/46,XX[2]} revealed a complex variant of the t(9;22) translocation, involving both chromosomes 9 and 22 as well as three other chromosomes (in addition to 9q34 and 22q11). FISH:BCR/ABL dual-color, dual-fusion probe was positive for t(9;22)(q34;q11.2) in 67.5% of cells with deletion on derivative chromosome 9. Standard and variant t(9;22) translocations in the current tyrosine kinase inhibitors era are thought to share a similar good prognosis.
In CML, mutations in the kinase domain of the BCR::ABL1 fusion gene may induce resistance to tyrosine kinase inhibitors, as was illustrated by case 744, containing multiple such mutations. On follow-up, this patient acquired an additional EVI1 rearrangement, indicating clonal evolution.
Case 505 had a cytogenetically cryptic BCR::ABL1 not detected by conventional karyotyping, but demonstrated by FISH and RT PCR, illustrating the need for additional investigation whenever the clinical and histological picture is suspicious for CML but conventional karyotyping is normal. Cryptic or masked BCR::ABL1 fusions occur in 2–10% of CML patients.
Myeloproliferative neoplasms, BCR-ABL1 negative
The classical BCR::ABL1-negative MPNs, which include essential thrombocythemia (ET), polycythemia vera (PV), and primary myelofibrosis (PMF), are rare in children, with global incidences for children and young adults estimated to be around 0.6/100,000 patients/year (range 0.004 to 0.9) for ET, 0.18/100,000 patients/year for PV, and 0.53/100,000 patients/year (range 0.003 to 1.5) for PMF [11].
Thrombotic events are less common in pediatric than in adult MPN, whereas adults have an increased risk of both arterial and venous thrombosis, children and adolescents with ET and PV predominantly have venous events (84.2%), and hemorrhagic episodes are rare (< 5%) [11]. Thromboses of the splanchnic territories are most frequent (75% of the venous events), with a large predominance of Budd-Chiari syndrome (62.5% of all venous events) [11]. It has been suggested that the presence of a driver mutation may confer an increased risk of thrombosis in children with MPN [10]. Progression towards myelofibrosis and transformation into AML is very rare in pediatric ET and PV [11].
Essential thrombocythemia
Pediatric ET must be differentiated from reactive thrombocytosis and from the non-clonal hereditary thrombocytosis caused by several different germline mutations in the genes for thrombopoietin, thrombopoietin receptor (MPL), JAK2, and gelsolin [12, 13]. Most of these germline mutations show an autosomal dominant pattern of inheritance [12]. Although the majority of these mutations is not or only rarely associated with thrombotic or hemorrhagic events, the JAK2 V617I, JAK2 T875N, and MPL S505N mutation do show an increased risk for vascular events [14,15,16]. Furthermore, the MPL S505N mutation is associated with splenomegaly and progression to BM fibrosis, significantly affecting life expectancy [15].
In a systematic review on pediatric MPN, 396 children with ET are reported, showing a mean age at diagnosis of 9.3 years [11]. In this study, about half of the patients were asymptomatic at diagnosis, with headache being the most frequent symptom, present in 27.5% of patients, and splenomegaly being the most frequent abnormal sign, occurring in 55% [11]. In this systematic review, A JAK2 V617F mutation was found in 31%, a CALR mutation in 10%, and a MPL mutation in 2% of patients [11], showing a much higher rate of triple negative disease (57%) than is reported in adults with ET (12%) [17].
Polycythemia vera
JAK2-negative PV cases must be differentiated from reactive polycythemia and from hereditary erythrocytosis. Hereditary erythrocytosis can be secondary due to, among others, mutations in genes in the oxygen sensing pathway, the erythropoietin (EPO) gene, or genes encoding high-affinity hemoglobins, and are associated with elevated or normal EPO levels [18]. In primary erythrocytosis, caused by mutations affecting erythroid progenitor cells, patients may, however, have low EPO levels, elevated hematocrit, and erythroid progenitors being hypersensitive to EPO, thereby mimicking PV [19]. Primary hereditary causes are very rare, the most common being mutations in the gene encoding the erythropoietin receptor (EPOR) [18, 19].
The mean age at diagnosis for pediatric PV is 11–12 years [11, 20]. Up to half of pediatric PV patients were reported to be asymptomatic at diagnosis, with headache being the most frequent symptom, reported in 30.5% to up to 100% of PV patients in some studies [11, 20, 21]. Thrombotic events occur in 15–25% of children, mainly in the form of Budd–Chiari syndrome [11, 20]. The presence of marked to severe leukocytosis (> 15 × 109/L) seems to be associated with both thrombotic and hemorrhagic complications [20]. In the largest study on PV, encompassing 75 children, splenomegaly was the most frequent abnormal sign, occurring in 15% of young PV patients [11]. A JAK2 V617F or JAK2 exon 12 mutation was demonstrated in this large study in only 37% and 2.5% of pediatric PV patients, respectively. The authors of this systematic review appropriately questioned whether these reported PV patients were properly diagnosed with PV and suggested that confirmation of this finding with a more recently diagnosed cohort could be helpful [11].
A recurring issue in MPN diagnosis is the separation of ET from PV particularly “masked” PV. As pediatric marrows already physiologically display high cellularity, determination of “hypercellularity” is difficult and the parameter of cellularity therefore usually is not contributory in separating ET from PV. Furthermore, lack of iron deposits is common in pediatric marrows and therefore this parameter does not discriminate PV from ET. To rule out PV, it is important referring to age-adjusted values (see, e.g., Nathan and Oski’s Hematology of Infancy and Childhood) for hemoglobin (Hb) and hematocrit (Hct) [22], particularly in patients less than 10 years old. A very low EPO level favors PV over ET. However, a normal EPO value does not rule out PV [20].
Primary myelofibrosis
Pediatric PMF is very rare. The two largest studies on pediatric PMF are one from the Texas Children’s Hospital, USA, describing 19 children, and one from China, describing 14 children with PMF [23, 24]. Median age at onset is very different between the two studies: 14 months (range 0–17 years) and 13.5 years (range 2–18 years) [23, 24]. Boys were affected slightly more than girls [23, 24]. Almost all patients had anemia, more than 85% showed thrombocytopenia, and 37–64% displayed neutropenia [23, 24]. The frequency of splenomegaly and hepatomegaly ranged between the studies from 21 to 63% for splenomegaly and 0 to 53% for hepatomegaly, with the lowest rates in the Chinese study [23, 24]. In the study from Texas, the amount of fibrosis varied, being MF1 (5 patients), MF2 (12 patients), or MF3 (2 patients). Megakaryocytic changes were described in this study as nuclear hypolobulation, separation of nuclear lobes, and the presence of micromegakaryocytes [23], rather than the presence of hyperchromatic, bulbous or “cloud-like”-shaped nuclei typically described in adult cases of PMF. JAK2 V617F and MPL W151L were tested in 17 and 6 children, respectively, but no mutations were found. Five cases had spontaneous resolution, but as no mutations were found, a reactive process in these cases cannot be ruled out. Although none showed acute leukemic transformation, 8 children died, half of them after hematopoietic stem cell transplantation (SCT) [23]. In the study from China, patients had either MF2 (3 patients) or MF3 (11 patients), and a CALR type 2 mutation was detected in 50% of patients [24]. Mutations of JAK2 V617F or MPL W515K/L were absent. In this study, none of the patients had spontaneous remission and six patients (43%) transformed to AML [24].
Workshop cases
Essential thrombocythemia
Of the 11 pediatric BCR::ABL1-negative MPN cases submitted to the workshop, 4 were classified by the panel as ET (Table 2). BM morphology was in all cases similar to that of adult ET with enlarged, hyperlobulated megakaryocytes (Fig. 1). Case 722 describes a 17-year-old male presenting with micturition problems and gastrointestinal bleeding. He was found to have thrombocytosis of 800–900 × 109/L and was diagnosed with a triple negative ET. The second ET case (case 408) describes an 11-year-old girl with pruritus, thrombocytosis of 1500 × 109/L and a CALR exon 9 mutation. The third ET case (case 153) describes a 17-year-old girl with chest pain, neck pain, and tingling of the arms for 2 weeks. She was found to have thrombocytosis of 1022 × 109/L and a MPL W515K mutation. The fourth ET case (case 564) was that of a 15-year-old girl who presented with headache. She had a 10-year history of thrombocytosis, most recently of 1100 × 109/L. A JAK2 V617F mutation was detected.
None of the four ET patients experienced thrombotic events. Three out of four cases showed mild splenomegaly (range 13.1–15.2 cm), which is consistent with previous reports that children with ET often show splenomegaly [11]. Only case 153 showed fibrosis (MF1).
Based on our workshop case submissions, it seems that the percentage of triple negative ET cases may be lower than what was reported in some studies [11], but not in others [25]. The observed variability may reflect whether reactive or constitutional etiologies were carefully excluded.
Polycythemia vera
Three pediatric PV cases were submitted to the workshop. In all three cases, a JAK2 V617F mutation was detected (Table 2).
The first case (case 602) describes a 7-year-old girl with a 3-year history of chronic headaches, epigastric abdominal pain, and constipation. She also had a 3-year history of persistent leukocytosis (WBC now 16.4 × 109/L) with neutrophilia (neutrophils 72%) and thrombocytosis (826 × 109/L), with recently additional erythrocytosis (Hb 17.2 g/dL; Hct 51.1%). EPO levels were low. She had splenomegaly and her JAK2 V617F mutation allelic burden was 5%. She had no thrombotic events. The BM biopsy showed a hypercellular marrow (cellularity 90%) with panmyelosis. Megakaryocytes were increased and showed pleomorphic features with occasional loose clusters.
The second PV case (case 496) describes a 19-year-old boy who was diagnosed at the age of 2 (year 1995) with carnitine deficiency. Concurrent blood abnormalities led to a clinical diagnosis of PV. A BM biopsy performed in 1997 showed increased pleomorphic megakaryocytes, consistent with the diagnosis PV (Fig. 2). Complete blood counts 1 year later showed polycythemia according to the local age adjusted reference values (Hb 14.4 g/dL, elevated Hct) as well as thrombocytosis (1000 × 109/L), undetectable EPO levels, and elevated LDH (613 U/L). In 2004, at the age of 10, his blood values deteriorated and he developed splenomegaly (16.1 cm). Pegylated interferon treatment was started at this point, on which he showed hematologic response and decrease in spleen size. In 2012, a JAK2 V617V mutation had been demonstrated. Unfortunately, he developed chronic portal vein thrombosis (in 2014) and pulmonary embolisms (in 2015). Whether or not his carnitine deficiency played a role in his thrombotic events remains undetermined.
The third PV case (case 700) describes a 9-year-old girl who presented with a large bruise on her left calf in association with weight loss and fatigue. No thrombotic events were reported. She was found to have splenomegaly (6 cm below the costal margin). Laboratory investigation revealed erythrocytosis (Hb 15.1 g/dl, Hct 57.4%, RBC 7.8 × 1012/L, MCV 73.9 fL) and leukocytosis (42.8 × 109/L), but normal platelet count (157 × 109/L). Peripheral blood (PB) smear showed 4% blasts. The BM aspirate had 14% blast by cytology; 13% myeloblasts were detected by flow cytometry. Ancillary studies demonstrated a JAK2 V617F mutation (variant allele frequency (VAF): 61%), as well as a JAK2 R867Q mutation (VAF: 5%), RUNX1 R204Q mutation (VAF: 45%), and IKZF1 loss. The BM biopsy showed hypercellular marrow (> 90% cellularity) with increased trilineage hematopoiesis and focally increased blasts (Fig. 3a). Megakaryocytes were pleomorphic with a predominance of smaller forms noticed (Fig. 3b). MF1 fibrosis was present. Based on the increased Hb and Hct (and of RBC), the presence of a low MCV, the high frequency of JAK2 mutation, and the increase of blasts, a diagnosis of PV presenting in accelerated phase was made. She underwent cytoreduction with ruxolitinib followed by a matched unrelated donor SCT.
Bone marrow biopsy of a 9-year-old girl with polycythemia vera in accelerated phase (case 700). The HE stain (a) shows increased left shifted granulopoiesis and erythropoiesis, the latter showing megaloblastoid changes, associated with increased megakaryopoiesis characterized by the presence of a mixture of large and small dysplastic forms as highlighted in the CD61 stain (b). Her peripheral blood smear showed 4% blasts and her BM aspirate contained 14% blast by cytology and 13% myeloblasts by flow cytometry
As all the three submitted PV cases were JAK2 positive, it seems that, similar to ET, the percentage of triple negative PV pediatric cases might be lower than previously published by others [11]. This is supported by a yet unpublished study from Weill Cornell Medical Center in which all children diagnosed with PV demonstrated a JAK2 mutation, as was presented at the virtual EAHP 2020 meeting by Dr. Kucine.
Primary myelofibrosis
Three cases of PMF were submitted to the workshop, two of which presenting in the prefibrotic stage (pre-PMF) (Table 2).
The first case (case 678) is that of a 5-year-old boy with a history of frequent upper respiratory infections, significant dental caries, and self-limited bloody stools. He was found to have thrombocytosis (range 889–1147 × 109/L), mild normocytic anemia (10.5 g/dL), and neutrophilic leukocytosis (WBC 11–23 × 109/L, 95% neutrophils). LDH was high. There was no splenomegaly. A CALR type 1 mutation was demonstrated. The first BM biopsy showed normocellular to focally hypercellular (> 90%) marrow with increased granulopoiesis and megakaryopoiesis, and decreased maturing erythropoiesis. The megakaryocytes showed cytological atypia with cloud-like/bulbous and often hyperchromatic nuclei with large tight clusters (Fig. 4a), similar to PMF seen in adults. This initial biopsy showed only mild fibrosis (MF1) consistent with pre-PMF (Fig. 4b), but a follow-up biopsy demonstrated progression to overt myelofibrosis (PMF-MF2) (Fig. 4c, d).
Bone marrow biopsies of a 5-year-old boy with primary myelofibrosis (PMF) with a CALR type 1 mutation (case 678), presenting in the prefibrotic stage and showing progression to the fibrotic stage. The first biopsy (a) shows tight clusters of markedly atypical megakaryocytes, including hypolobulated cloud-like and hyperchromatic forms, consistent with PMF. The reticulin stain (b) shows only mild fibrosis, MF1, consistent with the prefibrotic stage. A follow-up biopsy (c) shows hypercellular marrow with increased granulopoiesis, decreased erythropoiesis, tight clusters of atypical, hyperchromatic megakaryocytes and dilated sinusses (arrow). The reticulin stain (d) shows moderate fibrosis, MF2, consistent with progression to fibrotic stage PMF
The second PMF case (case 627) describes a 13-year-old girl presenting with headache and ear pain. Laboratory investigation revealed marked thrombocytosis (2000 × 109/L) and elevated LDH (340 U/L), but normal Hb and WBC. Splenomegaly (17 cm) was detected. No thrombosis was apparent. On treatment with hydroxyurea, platelet counts dropped. When hydroxyurea was stopped, platelet counts increased and neutrophilic leukocytosis developed (12 × 109/L with 85% neutrophils). The BM biopsy showed a hypercellular marrow characterized by a marked megakaryocytic proliferation with large forms displaying hypolobulated, cloud-like shaped hyperchromatic nuclei as well as some forms with hyperlobulated nuclei (Fig. 5a). Loose as well as tight clusters of megakaryocytes were present. There was no fibrosis (Fig. 5b) and no increase in blasts. The features in the marrow were consistent with pre-PMF. Molecular studies showed no driver mutation or any other mutation in the 45 genes NGS panel. On follow-up, the patient developed jugular and subclavian thrombosis, on which she was started on heparin, vitamin K antagonists, and pegylated interferon. Later, she underwent hematopoietic SCT from a tissue-matched donor with good outcome.
Two cases of pediatric primary myelofibrosis (PMF). a, b Bone marrow biopsy of a 13-year-old girl with a triple negative prefibrotic PMF (case 217) showing hypercellular marrow with tight clusters of atypical megakaryocytes (a HE) and no fibrosis (b reticulin). c, d Bone marrow biopsy a 17-year-old girl with a MPL positive PMF (case 182) showing hypercellular marrow with tight clusters of atypical megakaryocytes (c HE) and moderate fibrosis, MF2 (d reticulin), consistent with PMF, fibrotic stage
The third PMF case (case 182) describes a 17-year-old girl presenting with severe headaches. Five years earlier, she had similar symptoms and cerebral venous sinus thrombosis. Anti-cardiolipin IgG was elevated at the time and she was diagnosed with anti-phospholipid syndrome, which was treated with warfarin and aspirin. Repeated imaging revealed again venous sinus thrombosis, but also splenomegaly. Laboratory investigation showed leukocytosis (12.0 × 109/L), thrombocytosis (816 × 109/L), and elevated LDH (1216 U/L). Hb and EPO levels were normal. There was no leucoerythroblastic picture in the blood. The BM biopsy showed hypercellular marrow with increased granulopoiesis and megakaryopoiesis, and adequate erythropoiesis. The megakaryocytes were often large with bulbous nuclei and tight clustering, consistent with PMF (Fig. 5c). Patchy but overall moderate fibrosis (MF2) was present (Fig. 5d), consistent with fibrotic stage PMF. A MPL mutation with in-frame insertion was demonstrated (VAF: 15%).
All three submitted cases showed the typical histopathological features of PMF as seen in adults, suggesting that morphological criteria for PMF as described in the revised 2016 WHO classification might also be applicable for children.
MPN, unclassifiable
One pediatric MPN case (case 679) could not be further classified by the panel (Table 2). It describes a 15-year-old boy with a history of migraine, presenting with lower back and penile pain, and intermittent chest pain for the past several days. He was found to have thrombocytosis of 1834 × 109/L and leukocytosis of 34.3 × 109/L, and mild splenomegaly (18.8 cm). There was no anemia and the PB smear showed adequate normocytic/normochromic red blood cells. No MPN driver mutation or other mutation was demonstrable. The BM was slightly hypercellular with a megakaryocytic proliferation with enlarged, slightly clustered megakaryocytes, consistent with an MPN. There was no fibrosis. Based on BM morphology and marked leukocytosis, the panel felt that this case of triple negative MPN most likely represented pre-PMF (rather than ET).
Juvenile myelomonocytic leukemia and related diseases
Juvenile myelomonocytic leukemia
JMML is characterized by a proliferation of the granulocytic and monocytic lineages and develops at the age of 0 to 14 years, with a median age of 1.3–2 years, 95% occurring under the age of 5 [26,27,28]. Boys are affected about twice as frequent as girls [26, 27]. Most patients present with constitutional symptoms or signs of infections due to cytopenias and leukemic infiltration into organs [27]. Besides splenomegaly, hepatomegaly is almost always present and lymphadenopathy is common [27]. A skin rash is present in about one-third of cases [27, 28]. Hemoglobin F (HbF) is often elevated for age [28]. The PB values and PB cytology are the most important for diagnosis. BM findings alone are not diagnostic.
The majority (~ 85%) of JMML cases has a driver mutation in one of the genes of the canonical RAS pathway, most frequently in PTPN11, NRAS, KRAS, NF1, or CBL [26, 29, 30]. PTPN11, NRAS, KRAS, and CBL mutations can be either germline or somatic, whereas NF1 mutations are always germline [31,32,33,34]. The germline mutations generally occur as part of a broader syndrome (see RASopathies below), which carry an increased risk for developing JMML [31, 35].
A second, often subclonal, mutation occurs in less than half of JMML cases; this mutation can occur in another RAS pathway gene or in SETBP1, JAK3, SH3BP1, SH2B3, or components of the polycomb repressive complex 2, including EZH2 and ASXL1 [29, 30, 36]. Monosomy 7/del(7q) is the most common cytogenetic abnormality, present in 25–33% of cases [26,27,28].
The clinical course of JMML is generally aggressive, but mild forms or transient JMML-like myeloproliferations can occur, e.g., in the setting of a RASopathy or in the form of a RAS-associated autoimmune leukoproliferative disorder (RALD) as is discussed below.
RASopathies
Part of the JMML cases occur in the setting of a RASopathy. The RASopathies form a group of autosomal dominant neurodevelopmental dysmorphic syndromes caused by a germline mutation in genes that encode components of the RAS/MAPK pathway, which are detected in approximately 70–75% of patients [31]. They are associated with autoimmunity; 14% has a clinical diagnosis of an autoimmune disease and in 52% of patients, autoimmune antibodies can be demonstrated [37, 38]. The two most common RASopathies, Noonan syndrome and neurofibromatosis type 1, as well as CBL syndrome, one of the more rare Rasopathies also known as “Noonan-syndrome-like disorder with or without juvenile myelomonocytic leukemia,” predispose to JMML [32].
Noonan syndrome is the most common RASopathy and characterized by distinctive facial dysmorphisms, congenital heart defects and cardiomyopathy, reduced postnatal growth, and variable cognitive deficits [39]. A germline PTPN11 mutation is present in 40–50% of patients [40]. The remainder of the germline mutations occur in more than 10 other genes of the RAS/MAKP signaling pathway. A bona fide JMML is seen in 3% of children with PTPN11 mutated Noonan syndrome, often with an excess of blasts and very severe neonatal manifestations, half of patients dying in the first month of life [41]. JMML has occasionally been described in KRAS mutated Noonan syndrome [42]. A transient JMML-like myeloproliferative disorder is seen in 2.5–10% in infants with Noonan syndrome, almost invariably harboring a germline PTPN11 mutation [41, 43, 44].
Approximately 10–14% of JMML cases occur in children with neurofibromatosis type 1 [27], containing a germline mutation in the NF1 gene encoding for neurofibromin [45]. Children with neurofibromatosis type 1 and JMML tend to be older and show a more aggressive form of the disease [27].
The percentage of germline CBL mutations detected in JMML patients varies up to 17% in the largest studies [26, 46,47,48,49]. Most of these patients show constitutional anomalies consistent with CBL syndrome, which include Noonan-like features (developmental delay, congenital heart defects, and craniofacial anomalies), neurologic deficits, and pigmented skin lesions [34, 48, 50, 51]. CBL syndrome carries an increased risk for JMML. Whereas the few recently described cases of JMML with a somatic CBL mutations were refractory to chemotherapy [34], the clinical course of JMML with a germline CBL mutation is heterogeneous with some cases showing spontaneous regression and others behaving aggressively [34, 50, 51].
Workshop cases
Several challenging cases of JMML and related disorders were submitted to the workshop (Table 3).
JMML and RASopathies
Case 521 describes a 3-year-old girl with fever, showing typical JMML-associated features including leukocytosis, monocytosis, anemia, thrombocytopenia, splenomegaly, and elevated HbF (56.5%). The presence of a germline RRAS2 (pQ72L) mutation, a gene in the RAS/MAKP pathway, further confirmed the diagnosis of JMML. She had no clinical characteristics of a RASopathy. RRAS2 is one of the less frequently mutated genes in JMML and up to now has not been associated with Noonan syndrome, the most common RASopathy [52]. In addition, this patient had a somatic JAK3 (p.R657Q) mutation. JAK3 mutations in JMML are always secondary and found in distinct subclones, present in 2.8–12% of cases [29, 30]. JAK3 mutations are associated with mutated PTPN11 or RAS [29, 30], and associated with poor prognosis and progression of disease [30].
Case 279 describes a 5-year-old boy with a borderline-low leukocyte counts (WBC 5.1 × 109/L), monocytosis (1.07 × 109/L), severe anemia, thrombocytopenia, rare (~ 1%) circulating blasts, splenomegaly, and a somatic PTPN11 mutation. Although WBCs were low, there was absolute monocytosis, so that the diagnostic criteria for JMML were still met.
Case 492 describes a 5-month-old boy with AML with myelodysplasia-related changes (AML-MRC) who presented with decreased feeding and upper respiratory infections. He had leukocytosis, monocytosis, anemia, thrombocytopenia, and marginally elevated HbF (21.7%) as well as 19% circulating blasts. In addition, he was shown to have splenomegaly. BM showed trilinear dysplasia and 25–30% blasts. Monosomy 7 and an NF1 mutation (VAF: 75%) were documented. The peripheral blood findings (leukocytosis and monocytosis), the elevated HbF, and the presence of splenomegaly in association with NF1 mutation and monosomy 7 suggested the possibility of an underlying JMML that evolved to AML-MRC.
Case 344 describes a 4-year-old boy who underwent allogeneic SCT for JMML, who presented with acute leukemia 5 months thereafter. Flow cytometry of the BM revealed a mixed population of myeloid blasts (~ 30%) and progenitor B cells (~ 30%), raising the possibility of mixed phenotype acute leukemia (MPAL). FISH study detected a deletion 7q in 96% of cells. In the differential diagnosis, AML-MRC ex JMML is considered because of the 7q deletion, but the possibility of a therapy-related myeloid neoplasm is also possible despite the short time interval. Without further molecular data to assess whether the AML and JMML were clonally related, this differential diagnosis could not be resolved.
RAS-associated autoimmune leukoproliferative disorder
Case 473 describes a now 34-year-old woman with a history of pancytopenia since age 2. At the age of 5, she underwent splenectomy because of massive splenomegaly. She also had a history of rheumatoid arthritis and possible autoimmune lymphoproliferative syndrome (ALPS). At age 34, she presented to the hospital with diffuse lymphadenopathy as well as diffusely hypermetabolic BM uptake on PET-CT. CBC showed leukocytosis (21.4 × 109/l) with monocytosis (12%). Hb and platelet counts were within normal range. Due to these findings, BM and lymph node biopsies were performed. The BM biopsy and smears showed a hypercellular (90%) marrow with myeloid predominant trilineage hematopoiesis and increased monocytes. There was mild dysplasia within granulocytes and megakaryocytes. Plasma cells were slightly increased with occasional large forms. The lymph node biopsy showed a picture consistent with Rosai-Dorfman disease. In lymph node and BM, the same KRAS G13C mutation was detected.
The indolent course of the disease in the above case is most compatible with the entity called RAS associated autoimmune leukoproliferative disorder (RALD). Whereas JMML with KRAS or NRAS mutations generally run an aggressive course, RALD shows an indolent clinical behavior and long-term survival in absence of therapy [53]. As in the case described, RALD has many clinical and laboratory features overlapping with JMML, typically presenting with persistent absolute or relative monocytosis, massive splenomegaly, and lymphadenopathy, and is associated with autoimmunity [54, 55].
HbF can be increased for age [55]. Patients often present in childhood, frequently within the first year of life [55]. Almost all RALD patients meet the diagnostic criteria for JMML, but the accumulation of additional genetic abnormalities in JMML cells seems to contribute to the malignant phenotype in the latter [55]. RALD also shares many features with ALPS, including lymphadenopathy, massive splenomegaly, increased circulating B cells, hypergammaglobulinemia, and autoimmune cytopenia, but germline or somatic mutations in FAS, FASL, or CASP10 characteristic for ALPS are absent in RALD. In addition, the CD4-/CD8-double-negative T cell receptor αβ T cells typical for ALPS, are present at normal levels or only marginally elevated in the peripheral blood and absent in lymph nodes. As there are no molecular data on the possible ALPS of case 473 described above, it might well be that what was previously taken for ALPS might retrospectively already have been RALD given the many clinical similarities of these two entities. RALD with an associated Rosai-Dorfman disease has been previously described in a 15-year-old boy with the same KRAS G13C mutation as in the submitted case [56].
MDS/MPN with JMML-like features and t(4;17)(q12;q21); FIP1L1::RARA fusion
Two cases (case 471 and case 472) with a FIP1L1::RARA fusion were submitted to the workshop. As they phenotypically resemble JMML but lack a RAS pathway mutation, they were classified by the panel as MDS/MPN with JMML‑like features.
Case 471 describes a 9-month-old boy presenting with fevers and recurrent otitis media. It has recently been published [57]. The PB showed anemia (Hb 8.8 g/dL), leukocytosis (45.9 × 109/L), monocytosis (14%), increased promyelocytes (16%) without Auer rods, and numerous maturing myelomonocytic cells. There was marked dysgranulopoiesis and the monocytes showed some abnormal features. HbF was mildly elevated. Marked splenomegaly was present. No bruising, other bleeding manifestations, or features of disseminated intravascular coagulation were noticed. The BM biopsy and aspirate showed normocellular marrow with increased myeloid to erythroid ratio, markedly increased and left-shifted myelopoiesis, decreased erythropoiesis, and dysmegakaryopoiesis (Fig. 6a). There was an expanded population of myelomonocytic cells (29%) and promyelocytes (44%) with occasional basophilic granules (Fig. 6b). No Auer rods were identified. Ancillary studies demonstrated an in-frame fusion between FIP1L1 exon 13 and RARA exon 3 resulting in a t(4;17)(q12;q21). In addition, a somatic alteration of MAP2K2 p.R231L (VAF: 24.4%) was detected, on which no functional data are available and which may alter RAS-RAF-MEK-ERK signaling. Germline testing detected an NF1 mutation, which could be a benign polymorphism. He achieved remission after treatment with ATRA and arsenic trioxide (ATO) combined with idarubicin which induced only a short-lived remission. SCT showed good outcome.
Myelodysplastic/myeloproliferative neoplasm, with JMML-like features and t(4;17)(q12;q21); FIP1L1::RARA fusion in a 9-month-old girl (case 471). The bone marrow biopsy (a) shows a markedly increased and left-shifted myelopoiesis, decreased erythropoiesis and dysmegakaryopoiesis. The bone marrow aspirate smear (b) demonstrates the expanded population of myelomonocytic cells and atypical promyelocytes with occasional basophilic granules, without Auer rods
The second case (case 472) describes a 16-month-old girl with a 1-month history of intermittent fevers, generalized malaise, and night sweats. Her PB showed marked leukocytosis (156.4 × 109/L) with neutrophilic left-shift, dysgranulopoiesis, atypical monocytes, and promyelocytes without Auer rods. She had no splenomegaly. The BM showed cellular marrow (> 90% cellularity) with marked and abnormal myelomonoytic hyperplasia and decreased erythropoiesis and megakaryopoiesis. Blasts were < 5%. Her karyotype was 46,XX,t(2;3)(q11.2;p21),t(4;17)(q12;q21),add(7)(p21),del(90(p21)[18]/46,XX[2]. A FIP1L1::RARA fusion was demonstrated as well as a bi-allelic deletion of CDKN2A/2B.
Myeloid neoplasms with a FIP1L1::RARA fusion have previously been described in two adults and a child [58,59,60]. They characteristically show an increase in promyelocytes. The two adult patients with FIP1L1::RARA fusion were diagnosed as acute promyelocytic leukemia (APL) [58, 60]. One of the cases was shown to be sensitive to all-trans retinoic acid (ATRA) [60]. Promyelocytes with Auer rods and disseminated intravascular coagulation, which are characteristic features of APL, were, however, lacking. The only previously described pediatric case with FIP1L1::RARA fusion showed a clinical picture most consistent with JMML [59].
Besides cases associated with FIP1L1::RARA, other JMML mimics include cases with rare rearrangements, like ALK and ROS1 or CCDC88C::FLT3 fusions [61]. Patients with suspected JMML who lack canonical RAS pathway mutations should have RNA-Seq performed to identify potentially targetable gene fusions (e.g., FLT3).
Myelodysplastic syndromes
Pediatric MDS is rare, with an incidence of 1.8–4 cases/million [62]. It can occur at any age, with a median age at diagnosis of 8.3 years [63]. In contrast to adults, in whom low-grade MDS usually presents only with anemia, low-grade MDS in childhood commonly presents also with thrombocytopenia and neutropenia [63]. In addition, the mutational landscape of MDS in children differs from that in adults; mutations in genes for epigenetic regulation (e.g., TET2, ASXL1, and DNMT3A) and RNA splicing (e.g., SF3B1 and U2AF1) are rare in pediatric primary MDS (2%), whereas mutations in genes from the RAS/MAPK pathway are common (45%) [64].
A relatively high percentage of pediatric MDS cases represent secondary MDS. This includes therapy-related myeloid neoplasms, MDS secondary to acquired aplastic anemia, and MDS secondary to inherited predisposition syndromes, including the inherited bone marrow failure syndromes Fanconi anemia, severe congenital neutropenia, dyskeratosis congenita, and Shwachman-Diamond syndrome.
Underlying inherited or de novo germline predisposing genetic aberrations are being recognized in an increasing amount of pediatric MDS cases. According to the revised 2016 WHO classification, myeloid neoplasms with germline predisposition can be classified in three groups: (1) Myeloid neoplasms with germline predisposition without a pre-existing disorder or organ dysfunction, (2) myeloid neoplasms with germline predisposition and pre-existing platelet disorders, and (3) myeloid neoplasm with germline predisposition and other organ dysfunction, which includes myeloid neoplasm with germline GATA2 mutation, myeloid neoplasms associated with bone marrow failure syndromes, myeloid neoplasms associated with telomere biology disorders, JMML associated with neurofibromatosis, Noonan syndrome or Noonan syndrome-like disorders, and myeloid neoplasms associated with Down syndrome [65]. Additional germline predisposing mutations are still being discovered, such as mutations in sterile alpha motif domain-containing protein 9 (SAMD9) and its paralogue, SAMD9-like (SAMD9L) [66, 67]. In patients with a hematologic malignancy, cultured skin fibroblasts are the preferred tissue for germline mutation testing.
Together, GATA2 and SAMD9/SAMD9L syndromes currently form the most common predisposing conditions in pediatric MDS. In cases that originally were classified as primary pediatric MDS, 7% showed a GATA2 mutation and 8–17% a SAMD9/SAMD9L mutation [64, 68, 69]. They are particularly found in the setting of monosomy 7 [64, 68].
GATA2-related MDS typically shows BM hypocellularity with multilineage dysplasia [70,71,72]. Dysplastic megakaryocytes in GATA2 deficiency characteristically are both large and small with separated and peripheralized nuclear lobes, which may provide a morphologic clue to an underlying GATA2 deficiency [70,71,72]. In addition, increased reticulin fibrosis is much more frequent in GATA2 deficiency than in de novo MDS (46–73% versus 10%) [70,71,72]. Cytogenetic abnormalities are common in patients with GATA2 deficiency, most common being monosomy 7, der(1;7), or trisomy 8, whereas complex karyotypes are generally not seen [68, 73].
SAMD9/9L syndromes are autosomal dominant syndromes with variable penetrance. They cause a spectrum of multisystem disorders that carry a markedly increased risk of developing myeloid malignancies with monosomy 7 [74]. The median age at diagnosis of MDS in SAMD9/9L syndromes is 10 years (0.2–17.6), with the vast majority (90%) showing a hypocellular marrow with features similar to RCC [69]. MDS with excess blasts is seen in 10% of cases [69].
RCC is a provisional entity dealt with in the WHO MDS chapter [75]. It is defined by persistent cytopenia with < 5% blasts in the BM and < 2% blasts in the PB. Most patients with RCC (61–67%) have normal cytogenetics [76]. The vast majority (81%) shows decreased cellularity with a marrow which superficially resembles aplastic anemia. In contrast to aplastic anemia, RCC is reported to show left-shifted erythropoiesis arranged in large erythroid islands with an increased number of immature erythroblasts, particularly proerythroblasts [77]. Micromegakaryocytes are present in some cases [76, 77]. A similar RCC-like morphological picture can be seen in some hematological and non-hematological diseases, which must be excluded before a diagnosis of RCC can be made. Hematological disorders include the inherited BM failure syndromes, paroxysmal nocturnal haemoglobinuria (PNH), and hepatitis-associated aplastic anemia. Non-hematological disorders include infections, vitamin deficiencies, and metabolic disorders. A minority (19%) of RCC cases shows normo- or hypercellular marrow. Similar to hypocellular RCC, the BM in normo- and hypercellular RCC typically shows enlarged erythroid islands with impaired maturation, which is essential and an important clue to the diagnosis of RCC [76, 77].
Workshop cases
In total, 16 of the submitted cases were classified by the panel as MDS (Table 4).
Seven MDS cases had excess of blast (1 × MDS-EB1, 6 × MDS-EB2) and two of them were accompanied by fibrosis. One of the MDS-EB2 cases (case 677) was a 7-year-old boy with a t(3;5)(q25;q35); MLF1::NPM1, which is an aberration typically seen in younger pediatric patients with MDS or AML and is associated with an excellent response to SCT.
There were two cases of therapy-related MDS; one case of a 16-year-old boy with a history of Ewing sarcoma at the age of 15, and one case of a 14-year-old girl with a history of spinal neuroblastoma at the age of 2.
One of the submitted cases was classified as MDS with single lineage dysplasia and fibrosis (case 322) and six cases were classified as MDS, unclassifiable (MDS-U), based on the presence of single lineage dysplasia combined with pancytopenia (4 cases) or either single or multilineage dysplasia combined with 1% blasts in the PB (2 cases). Two of the MDS-U cases (case 723 and case 754) also showed fibrosis (MF2) and were therefore classified as MDS-U-F. Case 754 is illustrated in Fig. 7. In adults, MDS-U with 1% blasts has been described as a distinct subgroup of MDS-U with a poor prognosis [78]. Whether this also holds true for pediatric MDS-U remains to be determined.
Two pediatric cases of myelodysplastic syndrome (MDS) with fibrosis showing pronounced dysplasia, espcecially in the megakaryocytes. a, b Case 754 (MDS, unclassifiable, with fibrosis) shows moderate fibrosis, MF2 (a HE, b reticulin stain). c, d Case 322 (MDS with single lineaged dysplasia with fibrosis) shows severe fibrosis, MF3 (c HE, d reticulin stain)
In two of the MDS cases above (case 228 and case 723), the patients had a history of cytopenia, suggestive of an underlying germline condition: case 228 was a 10-year-old boy with MDS-U, known with congenital neutropenia, and case 723 was an 18-year-old young man with MDS-U-F with monosomy 7, who had a long history of neutropenia and thrombocytopenia. The latter patient received an allogeneic matched unrelated donor cord blood transplantation, 3 months after which he developed a donor cell MDS with again monosomy 7.
In one of the MDS-U cases (case 179), the 7-year-old boy had a de novo heterozygous mutation of RRAS and a concurrent del7/7q detected in his myeloid neoplasm. The presence of multiple phenotypic abnormalities, including scoliosis, craniosynostosis, and cardiac anomalies, as well as delayed milestones, was suggestive of an underlying RASopathy (i.e., Noonan syndrome), but the fact that his RAS mutation was not detected by whole exome sequencing (trio exome analysis) that was performed on normal tissue to detect germline mutations was in favor of a somatic mutation.
None of the cases was felt by the panel to fit the diagnosis of RCC; these cases were at least moderately cellular, not displaying the typical low cellularity of RCC reminiscent of AA. They also did not display markedly enlarged erythroid islands with impaired maturation, which is a key feature for the diagnosis of RCC, including the normo- and hypercellular RCC variants [76]. Rather, a predominance of granulopoiesis and a picture more consistent with MDS in adults was seen. One of the submitted cases came close to hypocellular RCC, but was eventually felt by the panel to represent aplastic anemia, partly due to its clinical picture with rapid onset cytopenia and the absence of cytogenetic aberrations.
Interestingly, as mentioned before, 5 of the 16 MDS cases showed marrow fibrosis (Fig. 7). The mean age in these fibrotic cases was 12.2 years (range 2–18 years), with a male:female ratio of 1:4. All of the workshop MDS-F cases showed chromosomal aberrations: 2 cases showed trisomy 8 (case 322 classified as MDS-SLD-F and case 754 classified as MDS-U-F), 1 case showed 3 copies of PML suggestive of trisomy 15 (case 329 classified as MDS-EB2-F), 1 case had monosomy 7 (case 723 classified as MDS-U-F), and the fifth case (case 682 classified as MDS-EB1-F) showed on interphase FISH a translocation of chromosome 11q with unknown fusion partner. In literature, fibrosis in pediatric MDS has been associated with germline GATA2 mutations [70,71,72], but unfortunately the information on GATA2 status was not available in many of submitted cases.
Acute myeloid leukemia
Although all types of AML can occur at the pediatric age, some forms occur more often or even exclusively in childhood, and the genetic landscape of pediatric AML differs from that of adult AML [79]. Certain mutations that are common in adult AML, such as mutations in DNMT3A, TP53, and IDH1 or IDH2, are rare in pediatric AML [79]. Mutations in NRAS, KRAS, KIT, WT1, MYC, CBL, GATA2, SETD2, PTPN11, and FLT3 are more common in children, and sites of mutation often differ from those detected in adults [79]. In addition, chromosomal rearrangements are more prevalent in childhood, with highest frequencies being found in infancy, declining with age [79].
The most common pediatric AML belongs to the group of AML with recurrent genetic abnormalities (AML-RGA). They include t(9;21)(p21.3;p23.3); KMT2A::MLLT3 (20–22%), t(8;21)(q22;q22.1); RUNX1::RUNX1T1 (9–15%), and inv(16)(p13.1q22) or t(16;16)(p13.1;q22); CBFB::MYH11 (6–10%), of which t(8;21)(q22;q22.1); RUNX1::RUNX1T1 and the two with involvement of chromosome 16 are associated with a favorable prognosis [79,80,81]. In cases of AML with variant KMT2A rearrangement, the prognosis depends on the fusion gene partner; some show a favorable prognosis, e.g., t(1;11)(q21;q23), while others show an adverse prognosis, e.g., t(10;11)(p12;q23), t(10;11)(p11.2;q23), t(6;11)(q27;q23), and t(4;11)(q21;q23) [82]. In t(9;11)(p22;q23); KMT2A::MLLT3 (previously called MLL-AF9 and the most common KMT2A fusion in pediatric AML), prognosis appears to be related to morphology, as those with acute monoblastic features have a significantly better outcome than cases showing other cytochemical types, at least in one study [82].
In addition to KMT2A, RUNX1, and CBFB, there are many other rare chromosomal rearrangements that display a higher prevalence in pediatric than in adult AML. Some rearrangements preferentially occur at infancy, such as AML (megakaryoblastic) with t(1;22)(p13.3;q13.1); RBM15::MKL1, AML with t(7;12)(q36;p13); MNX1::ETV6, AML with t(8;16)(p11;p13); KAT6A::CREBBP (which can spontaneously remit in infancy, but has an intermediate prognosis in later childhood), and AML with inv(16)(p13.3q24.3); CBFA2R3::GLIS2 as reviewed by Quessada et al. [83]. Others typically present later in childhood (median age varying between 6.6 and 12.4 years), such as AML with t(10;11)(p12;q14); PICALM::MLLT10, AML with t(6;9)(p23;34.1); DEK::NUP214, AML with t(16;21)(p11;q22); FUS::ERG, AML with t(16;21)(q24;q22); RUNX1::CBFA2T3, AML with t(5;11); NUP98::NSD1, AML with t(6;11)(q27;q23.3); KMT2A::MLLT4, and AML with t(15;17)(q24.1;q21.2); PML::RARA [83]. Other rare cytogenetic AML subgroups have also been reported [83].
As already discussed above in the section on MDS, several inherited or de novo germline aberrations are known to predispose to the development myeloid neoplasms. One of the predisposition syndromes is Down syndrome (DS), which children have a markedly increased risk of developing AML in their first 5 years of life, especially acute megakaryoblastic leukemia (AMKL). MDS and AML in DS are biologically similar and are therefore grouped together under the diagnosis “myeloid leukemia associated with Down syndrome” [84]. Somatic mutations in GATA1 are an early event in the leukemogenesis and are characteristic for myeloid leukemia associated with DS [85, 86]. Approximately 10% of newborns with DS develop a preleukemic clone with somatic GATA1 mutation. This preleukemic clone, known as transient myeloproliferative disease (TMD) or transient abnormal myelopoiesis (TAM), may be morphological indistinguishable from Down-associated AMKL, but resolves spontaneously in 60% of cases at a mean of 58 days (range 2–194 days) [87]. About 20% subsequently develops leukemia, predominantly AMKL, and about 20% experience early death mainly due to liver failure [87].
Workshop cases
In total, 12 cases of pediatric AML were included in the workshop, covering a wide spectrum of AML subtypes (Table 5). Four cases were classified as AML-RGA, four as AML-MRC, and three as AML not otherwise specified (AML-NOS). In addition, there were two cases of myeloid sarcoma.
AML with recurrent genetic abnormalities
The first AML-RGA case (case 458) was a 7-month-old girl with AML (megakaryoblastic) with t(1;22)(p13.3;q13.1); RBM15::MKL1. This is a rare translocation occurring in infants and presenting as AMKL.
The second case (case 511) was a 3-year-old girl with AML with CBFA2T3::GLIS2, which is equivalent to inv(16)(p13.3;q24.3). This is a rare cryptic chromosomal translocation associated with treatment-refractory disease, occurring especially in infants, and presenting in 20% of cases as an AMKL. In this case, the blasts showed a so-called RAM phenotype (phenotype named after initials of the first patient in which this was described), consisting of bright CD56 expression, dim or negative CD45 and CD38 expression, and lack of HLA-DR expression. The RAM phenotype is mainly seen in infants and very young patients, and an independent risk factor in pediatric AML patients associated with extremely poor outcome [88].
The third case (case 583) was a 12-year-old boy with AML with mutated NPM1. The NPM1 mutation is one of the most common recurrent cytogenetic aberrations in AML, and, in contrast to the previous two cytogenetic aberrations, not specific for childhood. Its frequency is rare in AML in infants (2.5%), but it increases with age to up to 34% in adult AML [79]. In addition to the NPM1 mutation, the patient had several other mutations: RAD21 (VAF: 43%), KRAS (VAF: 27%), and two different PTPN11 mutations (VAF: 10% and 2%).
The fourth AML-RGA case (case 187) was a 10-year-old boy with AML with t(8;21)(q22;q22.1); RUNX1T1::RUNX1, which interestingly showed myelomastocytic differentiation with increased serum tryptase (29 μg/L) and two KIT mutations (c.1251_1266delins16 and c.2466 T > A (p.Asn822Lys)), which have not been described in systemic mastocytosis. In both the AML blasts and the mast cells, the t(8;21) could be detected, indicating they belong to the same clone.
AML with myelodysplasia related changes
Four of the submitted AML cases were classified by the panel as AML-MRC; one based on a previous history of MDS (case 773), two based on the presence of a complex karyotype (case 361 and 150), and the fourth (case 796) based on the presence of an MDS-related cytogenetic abnormality, being del(7)(q22). The latter case also showed a CDK6::MECOM aberration, which is a rare anomaly described in high-risk pediatric AML. The resulting overexpressed MECOM protein could be demonstrated by immunohistochemistry.
AML not otherwise specified
Three of the submitted AML cases were classified as AML-NOS. The first case (case 282) showed megakaryoblastic differentiation and a normal karyotype, but on FISH a KMT2A (MLL) translocation (fusion partner not identified).
The second AML-NOS case (case 766) had a FLT3-ITD and a WT1 mutation, which concurrent presence forms a poor prognostic factor in de novo pediatric AML [89].
The third case (case 247) was considered AML-NOS. Although areas rich in proerythroblasts were noticed, the overall presence of > 20% myeloblasts supported a diagnosis of AML-NOS (over one of pure erythroid leukemia).
Myeloid sarcoma
There were two cases of myeloid sarcoma (Table 5), of which case 522 was a myeloid sarcoma (monoblastic variant) occurring in the skin of a 3-month-old girl, and case 630 a myeloid sarcoma in the orbit of a 5-year-old boy, which was followed by an AML with t(8;20;21)(q22;q11.2;q22.1); RUNX1::RUNXT1.
Acute megakaryoblastic leukemia
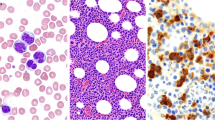
Interestingly, among the submitted AML cases, there was a relatively high frequency of AMKLs (Fig. 8), none of which associated with DS. Non-Down syndrome AMKL can be classified according to the WHO classification as AML-RGA, AML-MRC, or AML-NOS. Case 458 is an example of AML-RGA, being an AML (megakaryoblastic) with t(1;22)(p.13.3-q13.1); RBM15::MKL1. Other commonly recurring rearrangements in non-Down syndrome pediatric AMKL are CBFA2T3::GLIS2, NUP98::KDM5A, HOX rearrangements, and KMT2A rearrangements, the latter being illustrated by case 282. These other recurring rearrangements are, however, not separate WHO entities but currently classified as AML-NOS (megakaryoblastic), although they do have prognostic value as outcomes vary considerably [90]. Case 150 shows an example of AMKL classified as AML-MRC due to its complex karyotype.
Pediatric bone marrow biopsies showing acute myeloid leukemia (AML) with megakaryoblastic differentiation: a, b Case 282, classified as AML-NOS (megakaryoblastic) with KMT2A rearrangement (a HE, b CD61); c, d case 150, classified as AML-MRC due to a complex karyotype, showing partial megakaryoblastic differentiation (c HE, d CD61); e, f case 458, classified as AML-RGA, being an example of an AML (megakaryoblastic) with t(1;22)(p.13.3-q13.1); RBM15::MKL1 (e HE, f CD61)
Summary
The first section of the BM workshop of the EAHP 2020 virtual meeting was dedicated to pediatric myeloid neoplasms. Several interesting “take home messages” can be drawn from it:
-
CML is rare in childhood and CML biology in adults and children is different as underlined by the different BCR breakpoint distribution seen in the latter. One must always be aware of cytogenetically cryptic BCR::ABL1 variants and ABL1 TKI resistance mutations, as illustrated by the workshop cases 505 and 744.
-
Pediatric BCR::ABL1-negative MPNs are rare and differ from the adult cases at several points:
-
*
Mild splenomegaly is common even in ET and should therefore not be used as a criterion for separating ET from PMF.
-
*
Thrombotic events are less frequent than in adults and are largely venous, with a high frequency of Budd-Chiari syndrome.
-
*
High cellularity and lack of iron storages are common, especially in young children, and are therefore less reliable criteria for the distinction of ET versus PV.
-
*
WHO diagnostic criteria for diagnosing adult PV need to be adjusted in children by using appropriate age-related thresholds for establishing presence of erythrocytosis.
-
*
Although it has been reported that pediatric MPNs have a lower frequency of driver mutations (i.e., a higher frequency of triple negativity), this was not confirmed by the cases submitted to the workshop, in which a driver mutation was detected in 8 out of 11 (73%) cases. Further studies of adequately annotated cases diagnosed according to the WHO approach seem to be needed to clarify the exact frequency.
-
*
The features of pediatric PMF are overall similar to those seen in adult PMF, and the two submitted cases of prefibrotic (pre-)PMF underline the fact that that pre-PMF can also occur in children.
-
*
-
Apart from JMML, the “adult types” of MDS/MPN are basically not seen at the pediatric age. The workshop cases illustrate the following:
-
*
JMML may present as AML-MRC.
-
*
RRAS2 is one of the less frequently mutated genes of the RAS-pathway in JMML.
-
*
A second, often subclonal, mutation occurs in less than half of JMML cases; this mutation can occur in another RAS pathway gene or in SETBP1, JAK3, SH3BP1, SH2B3, or components of the polycomb repressive complex 2, including EZH2 and ASXL1.
-
*
Some of the JMMLs occur in the setting of an underlying RASopathy, which is a group of developmental disorders characterized by typical phenotypic features, caused by a germline mutation in genes that encode components of the RAS/MAPK pathway. Of these, Noonan syndrome, neurofibromatosis type 1, and CBL syndrome predispose to JMML.
-
*
JMML is generally an aggressive disease but milder forms and transient myeloproliferations occur: (1) Few cases with a KRAS or NRAS mutation show an indolent clinical course and long-term survival, which entity is called RAS-associated autoimmune leukoproliferative disorder (RALD), (2) infants with Noonan syndrome develop a transient JMML-like myeloproliferation in 2.5–10% of cases, which is almost invariably associated with a PTPN11 mutation, (3) JMML with a germline CBL mutation may show spontaneous regression.
-
*
Two rare cases of MDS/MPN with JMML-like features and t(4;17)(q12;q21); FIP1L1::RARA fusion are described. These cases manifest with monocytosis and an abnormal myelomonocytic proliferation similar to JMML but may be lacking some clinical features of JMML and do not contain identifiable mutations in the RAS pathway or other JMML defining genetic aberrations. FIP1L1::RARA fusion could also raise the possibility of acute promyelocytic leukemia, although typical features are lacking (no increase of promyelocytes with Auer rods, no disseminated intravascular coagulation). Whether these pediatric cases should be classified as JMML in the future remains to be determined.
-
*
-
Pediatric MDS is rare. Most of the workshop cases were classified as MDS-U or MDS-EB1 or 2:
-
*
Five of the 16 MDS cases submitted to the workshop had fibrosis, with a female predominance (M:F = 1:4) and a mean age of 12.2 years (range 2–18 years). All fibrotic cases showed chromosomal aberrations, including trisomy 8, trisomy 15, monosomy 7, and 11q translocation.
-
*
Especially in children and young adults, MDS and AML may develop secondary to aplastic anemia, an inherited bone marrow failure syndrome or in the context of another underlying germline mutation which predisposes to the development of a myeloid neoplasm, of which GATA2 and SAMD9/SAMD9L are at the moment the most common.
-
*
-
All types of AML can occur at the pediatric age, and several cases of AML-RGA, AML-MRC, and AML-NOS, as well as 2 cases of myeloid sarcoma, were included in the workshop:
-
*
Some recurrent cytogenetic aberrations are typical of childhood, such as AML (megakaryoblastic) with t(1;22)(p13.3;q13.1); RBM15::MKL1 and AML with CBFA2T3::GLIS2 (equivalent to inv(16)(p13.3;q24.3)) as illustrated by the workshop. Others are more common in adults, but can be seen in childhood as well, as illustrated by a case of AML with t(8;21); RUNX1T1::RUNX1.
-
*
The workshop contained a relatively high frequency of AMKL, not associated with DS. These can be classified as AML-RGA, AML-MRC, or AML-NOS. The t(1;22)(p13.3;q13.1); RBM15::MKL1 is the only recurrent cytogenetic abnormality in AMKL classified by the WHO as a separate entity, but the other recurrent cytogenetic aberrations in non-Down syndrome AMKL are also of prognostic importance and therefore deserve further investigation.
-
*
References
Millot F, Traore P, Guilhot J, Nelken B, Leblanc T, Leverger G, Plantaz D, Bertrand Y, Bordigoni P, Guilhot F (2005) Clinical and biological features at diagnosis in 40 children with chronic myeloid leukemia. Pediatrics 116:140–143. https://doi.org/10.1542/peds.2004-2473
Madabhavi I, Patel A, Modi G, Anand A, Panchal H, Parikh S (2020) Pediatric chronic myeloid leukemia: a single-center experience. J Cancer Res Ther 16:110–115. https://doi.org/10.4103/jcrt.JCRT_833_15
Millot F, Guilhot J, Baruchel A, Petit A, Bertrand Y, Mazingue F, Lutz P, Verite C, Berthou C, Galambrun C, Sirvent N, Yakouben K, Schmitt C, Gandemer V, Reguerre Y, Couillault G, Mechinaud F, Cayuela JM (2014) Impact of early molecular response in children with chronic myeloid leukemia treated in the French Glivec phase 4 study. Blood 124:2408–2410. https://doi.org/10.1182/blood-2014-05-578567
Hijiya N, Schultz KR, Metzler M, Millot F, Suttorp M (2016) Pediatric chronic myeloid leukemia is a unique disease that requires a different approach. Blood 127:392–399. https://doi.org/10.1182/blood-2015-06-648667
Knofler R, Lange BS, Paul F, Tiebel O, Suttorp M (2020) Bleeding signs due to acquired von Willebrand syndrome at diagnosis of chronic myeloid leukaemia in children. Br J Haematol 188:701–706. https://doi.org/10.1111/bjh.16241
Marin D, Ibrahim AR, Lucas C, Gerrard G, Wang L, Szydlo RM, Clark RE, Apperley JF, Milojkovic D, Bua M, Pavlu J, Paliompeis C, Reid A, Rezvani K, Goldman JM, Foroni L (2012) Assessment of BCR-ABL1 transcript levels at 3 months is the only requirement for predicting outcome for patients with chronic myeloid leukemia treated with tyrosine kinase inhibitors. J Clin Oncol 30:232–238. https://doi.org/10.1200/JCO.2011.38.6565
Krumbholz M, Karl M, Tauer JT, Thiede C, Rascher W, Suttorp M, Metzler M (2012) Genomic BCR-ABL1 breakpoints in pediatric chronic myeloid leukemia. Genes Chromosom Cancer 51:1045–1053. https://doi.org/10.1002/gcc.21989
Youn M, Smith SM, Lee AG, Chae HD, Spiteri E, Erdmann J, Galperin I, Jones LM, Donato M, Abidi P, Bittencourt H, Lacayo N, Dahl G, Aftandilian C, Davis KL, Matthews JA, Kornblau SM, Huang M, Sumarsono N, Redell MS, Fu CH, Chen IM, Alonzo TA, Eklund E, Gotlib J, Khatri P, Sweet-Cordero EA, Hijiya N, Sakamoto KM (2021) Comparison of the transcriptomic signatures in pediatric and adult CML. Cancers (Basel) 13. https://doi.org/10.3390/cancers13246263
Millot F, Guilhot J, Suttorp M, Gunes AM, Sedlacek P, De Bont E, Li CK, Kalwak K, Lausen B, Culic S, Dworzak M, Kaiserova E, De Moerloose B, Roula F, Biondi A, Baruchel A (2017) Prognostic discrimination based on the EUTOS long-term survival score within the International Registry for Chronic Myeloid Leukemia in children and adolescents. Haematologica 102:1704–1708. https://doi.org/10.3324/haematol.2017.170035
Tafesh L, Musgrave K, Roberts W, Plews D, Carey P, Biss T (2019) Myeloproliferative neoplasms in children and adolescents and thrombosis at unusual sites: the role of driver mutations. J Pediatr Hematol Oncol 41:490–493. https://doi.org/10.1097/MPH.0000000000001173
Ianotto JC, Curto-Garcia N, Lauermanova M, Radia D, Kiladjian JJ, Harrison CN (2019) Characteristics and outcomes of patients with essential thrombocythemia or polycythemia vera diagnosed before 20 years of age: a systematic review. Haematologica 104:1580–1588. https://doi.org/10.3324/haematol.2018.200832
Han EY, Catherwood M, McMullin MF (2021) Hereditary thrombocytosis: the genetic landscape. Br J Haematol 194:1098–1105. https://doi.org/10.1111/bjh.17741
Stockklausner C, Duffert CM, Cario H, Knofler R, Streif W, Kulozik AE, Hamostaseforschung TH-PSdGfT-u, of Gesellschaft fur Padiatrische Onkologie und H, (2021) Thrombocytosis in children and adolescents-classification, diagnostic approach, and clinical management. Ann Hematol 100:1647–1665. https://doi.org/10.1007/s00277-021-04485-0
Yoshimitsu M, Hachiman M, Uchida Y, Arima N, Arai A, Kamada Y, Shide K, Ito M, Shimoda K, Ishitsuka K (2019) Essential thrombocytosis attributed to JAK2-T875N germline mutation. Int J Hematol 110:584–590. https://doi.org/10.1007/s12185-019-02725-8
Teofili L, Giona F, Torti L, Cenci T, Ricerca BM, Rumi C, Nunes V, Foa R, Leone G, Martini M, Larocca LM (2010) Hereditary thrombocytosis caused by MPLSer505Asn is associated with a high thrombotic risk, splenomegaly and progression to bone marrow fibrosis. Haematologica 95:65–70. https://doi.org/10.3324/haematol.2009.007542
Mead AJ, Rugless MJ, Jacobsen SEW, Schuh A (2021) Germline JAK2 mutation in a family with hereditary thrombocytosis. N Engl J Med 366:967–969. https://doi.org/10.1056/NEJMc1200349
Prins D, Gonzalez Arias C, Klampfl T, Grinfeld J, Green AR (2020) Mutant calreticulin in the myeloproliferative neoplasms. Hemasphere 4:e333. https://doi.org/10.1097/HS9.0000000000000333
McMullin MF (2019) Diagnostic workflow for hereditary erythrocytosis and thrombocytosis. Hematol Am Soc Hematol Educ Program 2019:391–396. https://doi.org/10.1182/hematology.2019000047
de la Chapelle A, Träskelin AL, Juvonen E (1993) Truncated erythropoietin receptor causes dominantly inherited benign human erythrocytosis. Proc Natl Acad Sci U S A 15:1195–1199. https://doi.org/10.1073/pnas.90.10.4495
Cario H, McMullin MF, Pahl HL (2009) Clinical and hematological presentation of children and adolescents with polycythemia vera. Ann Hematol 88:713–719. https://doi.org/10.1007/s00277-009-0758-y
Kucine N, Al-Kawaaz M, Hajje D, Bussel J, Orazi A (2019) Difficulty distinguishing essential thrombocythaemia from polycythaemia vera in children with JAK2 V617F-positive myeloproliferative neoplasms. Br J Haematol 185:136–139. https://doi.org/10.1111/bjh.15386
Brugnara C, Oski FA, Nathan DG (2015) Diagnostic approach to the anemic patient. In: Orkin S, Fisher D, Ginsburg D, Look AT, Lux S, Nathan D (eds) Nathan and Oski's hematology and oncology of infancy and childhood. Elseivier Saunders
DeLario MR, Sheehan AM, Ataya R, Bertuch AA, Vega C 2nd, Webb CR, Lopez-Terrada D, Venkateswaran L (2012) Clinical, histopathologic, and genetic features of pediatric primary myelofibrosis–an entity different from adults. Am J Hematol 87:461–464. https://doi.org/10.1002/ajh.23140
An W, Wan Y, Guo Y, Chen X, Ren Y, Zhang J, Chang L, Wei W, Zhang P, Zhu X (2014) CALR mutation screening in pediatric primary myelofibrosis. Pediatr Blood Cancer 61:2256–2262. https://doi.org/10.1002/pbc.25211
Teofili L, Giona F, Martini M, Cenci T, Guidi F, Torti L, Palumbo G, Amendola A, Foa R, Larocca LM (2007) Markers of myeloproliferative diseases in childhood polycythemia vera and essential thrombocythemia. J Clin Oncol 25:1048–1053. https://doi.org/10.1200/JCO.2006.08.6884
Nathany S, Chatterjee G, Ghai S, Moulik NR, Shetty D, Subramanian PG, Tembhare P, Gujral S, Dhamne C, Banavali S, Narula G, Patkar N (2021) Mutational landscape of juvenile myelomonocytic leukemia (JMML)-A real-world context. Int J Lab Hematol 43:1531–1538. https://doi.org/10.1111/ijlh.13680
Niemeyer CM, Arico M, Basso G, Biondi A, Cantu Rajnoldi A, Creutzig U, Haas O, Harbott J, Hasle H, Kerndrup G, Locatelli F, Mann G, Stollmann-Gibbels B, van ’t Veer-Korthof ET, van Wering E, Zimmermann M, (1997) Chronic myelomonocytic leukemia in childhood: a retrospective analysis of 110 cases. European Working Group on Myelodysplastic Syndromes in childhood (EWOG-MDS). Blood 15:3534–3543
Luna-Fineman S, Shannon KM, Atwater SK, Davis J, Masterson M, Ortega J, Sanders J, Steinherz P, Weinberg V, Lange BJ (1999) Myelodysplastic and myeloproliferative disorders of childhood: a study of 167 patients. Blood 92:459–466
Sakaguchi H, Okuno Y, Muramatsu H, Yoshida K, Shiraishi Y, Takahashi M, Kon A, Sanada M, Chiba K, Tanaka H, Makishima H, Wang X, Xu Y, Doisaki S, Hama A, Nakanishi K, Takahashi Y, Yoshida N, Maciejewski JP, Miyano S, Ogawa S, Kojima S (2013) Exome sequencing identifies secondary mutations of SETBP1 and JAK3 in juvenile myelomonocytic leukemia. Nat Genet 45:937–941. https://doi.org/10.1038/ng.2698
Bresolin S, De Filippi P, Vendemini F, D’Alia M, Zecca M, Meyer LH, Danesino C, Locatelli F, Masetti R, Basso G, Te Kronnie G (2016) Mutations of SETBP1 and JAK3 in juvenile myelomonocytic leukemia: a report from the Italian AIEOP study group. Oncotarget 7:28914–28919. https://doi.org/10.18632/oncotarget.8016
Tartaglia M, Gelb BD (2010) Disorders of dysregulated signal traffic through the RAS-MAPK pathway: phenotypic spectrum and molecular mechanisms. Ann N Y Acad Sci 1214:99–121. https://doi.org/10.1111/j.1749-6632.2010.05790.x
Lasho T, Patnaik MM (2020) Juvenile myelomonocytic leukemia - a bona fide RASopathy syndrome. Best Pract Res Clin Haematol 33:101171. https://doi.org/10.1016/j.beha.2020.101171
Tartaglia M, Niemeyer CM, Fragale A, Song X, Buechner J, Jung A, Hählen K, Hasle H, Licht JD, Gelb BD (2003) Somatic mutations in PTPN11 in juvenile myelomonocytic leukemia, myelodysplastic syndromes and acute myeloid leukemia. Nat Genet 34:148–150. https://doi.org/10.1038/ng1156
Hecht A, Meyer JA, Behnert A, Wong E, Chehab F, Olshen A, Hechmer A, Aftandilian C, Bhat R, Choi SW, Chonat S, Farrar JE, Fluchel M, Frangoul H, Han JH, Kolb EA, Kuo DJ, MacMillan ML, Maese L, Maloney KW, Narendran A, Oshrine B, Schultz KR, Sulis ML, Van Mater D, Tasian SK, Hofmann WK, Loh ML, Stieglitz E (2022) Molecular and phenotypic diversity of CBL-mutated juvenile myelomonocytic leukemia. Haematologica 107:178–186. https://doi.org/10.3324/haematol.2020.270595
Niemeyer C (2018) JMML genomics and decisions. Hematol Am Soc Hematol Educ Program 2018:30–312. https://doi.org/10.1182/asheducation-2018.1.307
Stieglitz E, Taylor-Weiner AN, Chang TY, Gelston LC, Wang YD, Mazor T, Esquivel E, Yu A, Seepo S, Olsen S, Rosenberg M, Archambeault SL, Abusin G, Beckman K, Brown PA, Briones M, Carcamo B, Cooper T, Dahl GV, Emanuel PD, Fluchel MN, Goyal RK, Hayashi RJ, Hitzler J, Hugge C, Liu YL, Messinger YH, Mahoney DH Jr, Monteleone P, Nemecek ER, Roehrs PA, Schore RJ, Stine KC, Takemoto CM, Toretsky JA, Costello JF, Olshen AB, Stewart C, Li Y, Ma J, Gerbing RB, Alonzo TA, Getz G, Gruber T, Golub T, Stegmaier K, Loh ML (2015) The genomic landscape of juvenile myelomonocytic leukemia. Nat Genet 47:1326–1333. https://doi.org/10.1038/ng.3400
Siano MA, Marchetti V, Pagano S, Di Candia F, Alessio M, De Brasi D, De Luca A, Pinna V, Sestito S, Concolino D, Tartaglia M, Strisciuglio P, D’Esposito V, Cabaro S, Perruolo G, Formisano P, Melis D (2021) Risk of autoimmune diseases in patients with RASopathies: systematic study of humoral and cellular immunity. Orphanet J Rare Dis 16:410. https://doi.org/10.1186/s13023-021-02050-6
Quaio CR, Carvalho JF, da Silva CA, Bueno C, Brasil AS, Pereira AC, Jorge AA, Malaquias AC, Kim CA, Bertola DR (2012) Autoimmune disease and multiple autoantibodies in 42 patients with RASopathies. Am J Med Genet A 158A:1077–1082. https://doi.org/10.1002/ajmg.a.35290
Roberts AE, Allanson JE, Tartaglia M, Gelb BD (2013) Noonan syndrome. The Lancet 381:333–342. https://doi.org/10.1016/s0140-6736(12)61023-x
Tartaglia M, Kalidas K, Shaw A, Song X, Musat DL, van der Burgt I, Brunner HG, Bertola DR, Crosby A, Ion A, Kucherlapati RS, Jeffery S, Patton MA, Gelb BD (2002) PTPN11 mutations in Noonan syndrome: molecular spectrum, genotype-phenotype correlation, and phenotypic heterogeneity. Am J Hum Genet 70:1555–1563. https://doi.org/10.1086/340847
Strullu M, Caye A, Lachenaud J, Cassinat B, Gazal S, Fenneteau O, Pouvreau N, Pereira S, Baumann C, Contet A, Sirvent N, Mechinaud F, Guellec I, Adjaoud D, Paillard C, Alberti C, Zenker M, Chomienne C, Bertrand Y, Baruchel A, Verloes A, Cave H (2014) Juvenile myelomonocytic leukaemia and Noonan syndrome. J Med Genet 51:689–697. https://doi.org/10.1136/jmedgenet-2014-102611
Schubbert S, Zenker M, Rowe SL, Boll S, Klein C, Bollag G, van der Burgt I, Musante L, Kalscheuer V, Wehner LE, Nguyen H, West B, Zhang KY, Sistermans E, Rauch A, Niemeyer CM, Shannon K, Kratz CP (2006) Germline KRAS mutations cause Noonan syndrome. Nat Genet 38:331–336. https://doi.org/10.1038/ng1748
Kratz CP, Niemeyer CM, Castleberry RP, Cetin M, Bergstrasser E, Emanuel PD, Hasle H, Kardos G, Klein C, Kojima S, Stary J, Trebo M, Zecca M, Gelb BD, Tartaglia M, Loh ML (2005) The mutational spectrum of PTPN11 in juvenile myelomonocytic leukemia and Noonan syndrome/myeloproliferative disease. Blood 106:2183–2185. https://doi.org/10.1182/blood-2005-02-0531
Choong K, Freedman MH, Chitayat D, Kelly EN, Taylor G, Zipursky A (1999) Juvenile myelomonocytic leukemia and Noonan syndrome. J Pediatr Hematol Oncol 21:523–527
Xu G, O’Connell P, Viskochil D, Cawthon R, Robertson M, Culver M, Dunn D, Stevens J, Gesteland R, White R, Weiss R (1990) The neurofibromatosis type 1 gene encodes a protein related to GAP. Cell 62:599–608. https://doi.org/10.1016/0092-8674(90)90024-9
Loh ML, Sakai DS, Flotho C, Kang M, Fliegauf M, Archambeault S, Mullighan CG, Chen L, Bergstraesser E, Bueso-Ramos CE, Emanuel PD, Hasle H, Issa JP, van den Heuvel-Eibrink MM, Locatelli F, Stary J, Trebo M, Wlodarski M, Zecca M, Shannon KM, Niemeyer CM (2009) Mutations in CBL occur frequently in juvenile myelomonocytic leukemia. Blood 114:1859–1863. https://doi.org/10.1182/blood-2009-01-198416
Shiba N, Kato M, Park MJ, Sanada M, Ito E, Fukushima K, Sako M, Arakawa H, Ogawa S, Hayashi Y (2010) CBL mutations in juvenile myelomonocytic leukemia and pediatric myelodysplastic syndrome. Leukemia 24:1090–1092. https://doi.org/10.1038/leu.2010.49
Perez B, Mechinaud F, Galambrun C, Ben Romdhane N, Isidor B, Philip N, Derain-Court J, Cassinat B, Lachenaud J, Kaltenbach S, Salmon A, Desiree C, Pereira S, Menot ML, Royer N, Fenneteau O, Baruchel A, Chomienne C, Verloes A, Cave H (2010) Germline mutations of the CBL gene define a new genetic syndrome with predisposition to juvenile myelomonocytic leukaemia. J Med Genet 47:686–691. https://doi.org/10.1136/jmg.2010.076836
Murakami N, Yusuke O, Yoshida K, Yuichi Shiraishi Y, Nagae G, Suzuki K, Narita A, Sakaguchi H, Kawashima N, Wang X, Xu Y, Chiba K, Tanaka H, Hama A, Sanada M, Ito M, Hirayama M, Watanabe A, Ueno T, Kojima S, Aburatani H, Mano H, Miyano S, Ogawa S, Takahashi Y, Muramatsu H (2018) Integrated molecular profiling of juvenile myelomonocytic leukemia. Blood 131:1576–1586. https://doi.org/10.1182/blood-2017-07-798157
Cardoso L, Galan-Gomez V, Corral-Sanchez MD, Perez-Martinez A, Riesco S, Isidoro-Garcia M, Escudero A (2021) Juvenile myelomonocytic leukemia in CBL syndrome associated with germline splice-site mutations: Two case reports and a literature review. Clin Case Rep 9:e04260. https://doi.org/10.1002/ccr3.4260
Niemeyer CM, Wang MW, Shin DH, Furlan I, Erlacher M, Bunin NJ, Bunda S, Finklestein JZ, Gorr TA, Mehta P, Schmid I, Kropshofer G, Corbacioglu S, Lang PJ, Klein C, Schlegel P-G, Heinzmann A, Schneider M, Starý J, van den Heuvel-Eibrink MM, Hasle H, Locatelli F, Sakai D, Archambeault S, Chen L, Russell RC, Sybingco SS, Ohh M, Braun BS, Flotho C, Loh ML (2010) Germline CBL mutations cause developmental abnormalities and predispose to juvenile myelomonocytic leukemia. Nat Genet 42:794–800. https://doi.org/10.1038/ng.641
Ceremsak JJ, Yu A, Esquivel E, Lissewski C, Zenker M, Loh ML, Stieglitz E (2016) Germline RRAS2 mutations are not associated with Noonan syndrome. J Med Genet 53:728. https://doi.org/10.1136/jmedgenet-2016-103889
Niemela JE, Lu L, Fleisher TA, Davis J, Caminha I, Natter M, Beer LA, Dowdell KC, Pittaluga S, Raffeld M, Rao VK, Oliveira JB (2011) Somatic KRAS mutations associated with a human nonmalignant syndrome of autoimmunity and abnormal leukocyte homeostasis. Blood 117:2883–2886. https://doi.org/10.1182/blood-2010-07-295501
Oliveira JB, Bidère N, Niemela JE, Zheng L, Sakai K, Nix CP, Danner RL, Barb J, Munson PJ, Puck JM, Dale J, Straus SE, Fleisher TA, Lenardo M (2007) NRAS mutation causes a human autoimmune lymphoproliferative syndrome. Proc Natl Acad Sci U S A 104:8953–8958. https://doi.org/10.1073/pnas.0702975104
Calvo KR, Price S, Braylan RC, Oliveira JB, Lenardo M, Fleisher TA, Rao VK (2015) JMML and RALD (Ras-associated autoimmune leukoproliferative disorder): common genetic etiology yet clinically distinct entities. Blood 125:2753–2758. https://doi.org/10.1182/blood-2014-11-567917
Ragotte RJ, Dhanrajani A, Pleydell-Pearce J, Del Bel KL, Tarailo-Graovac M, van Karnebeek C, Terry J, Senger C, McKinnon ML, Seear M, Prendiville JS, Tucker LB, Houghton K, Cabral DA, Guzman J, Petty RE, Brown KL, Tekano J, Wu J, Morishita KA, Turvey SE (2017) The importance of considering monogenic causes of autoimmunity: a somatic mutation in KRAS causing pediatric Rosai-Dorfman syndrome and systemic lupus erythematosus. Clin Immunol 175:143–146. https://doi.org/10.1016/j.clim.2016.12.006
Miltiadous O, Petrova-Drus K, Kaicker S, Mathew S, Kluk M, Geyer JT, Rodriguez-Sanchez I, Bouvier N, Inghirami G, Stieglitz E, Khedoudja N, Benayed R, Richardson M, Anderson W, Benhamida J, You D, Londono D, Kung AL, Prockop SE, Roshal M, Zhang Y, Shukla N (2022) Successful treatment and integrated genomic analysis of an infant with FIP1L1-RARA fusion-associated myeloid neoplasm. Blood Adv 6:1137–1142. https://doi.org/10.1182/bloodadvances.2021004966
Menezes J, Acquadro F, Perez-Pons de la Villa C, Garcia-Sanchez F, Alvarez S, Cigudosa JC (2011) FIP1L1/RARA with breakpoint at FIP1L1 intron 13: a variant translocation in acute promyelocytic leukemia. Haematologica 96:1565–1566. https://doi.org/10.3324/haematol.2011.047134
Buijs A, Bruin M (2007) Fusion of FIP1L1 and RARA as a result of a novel t(4;17)(q12;q21) in a case of juvenile myelomonocytic leukemia. Leukemia 21:1104–1108. https://doi.org/10.1038/sj.leu.2404596
Kondo T, Mori A, Darmanin S, Hashino S, Tanaka J, Asaka M (2008) The seventh pathogenic fusion gene FIP1L1-RARA was isolated from a t(4;17)-positive acute promyelocytic leukemia. Haematologica 93:1414–1416. https://doi.org/10.3324/haematol.12854
Chao AK, Meyer JA, Lee AG, Hecht A, Tarver T, Van Ziffle J, Koegel AK, Golden C, Braun BS, Sweet-Cordero EA, Smith CC, Dvorak CC, Loh ML, Stieglitz E (2020) Fusion driven JMML: a novel CCDC88C-FLT3 fusion responsive to sorafenib identified by RNA sequencing. Leukemia 34:662–666. https://doi.org/10.1038/s41375-019-0549-y
Glaubach T, Robinson LJ, Corey SJ (2014) Pediatric myelodysplastic syndromes: they do exist! J Pediatr Hematol Oncol 36:1–7. https://doi.org/10.1097/MPH.0000000000000046
Kardos G, Baumann I, Passmore SJ, Locatelli F, Hasle H, Schultz KR, Stary J, Schmitt-Graeff A, Fischer A, Harbott J, Chessells JM, Hann I, Fenu S, Rajnoldi AC, Kerndrup G, Van Wering E, Rogge T, Nollke P, Niemeyer CM (2003) Refractory anemia in childhood: a retrospective analysis of 67 patients with particular reference to monosomy 7. Blood 102:1997–2003. https://doi.org/10.1182/blood-2002-11-3444
Schwartz JR, Ma J, Lamprecht T, Walsh M, Wang S, Bryant V, Song G, Wu G, Easton J, Kesserwan C, Nichols KE, Mullighan CG, Ribeiro RC, Klco JM (2017) The genomic landscape of pediatric myelodysplastic syndromes. Nat Commun 8:1557. https://doi.org/10.1038/s41467-017-01590-5
Peterson LC, Bloomfield CD, Niemeyer CM, Döhner H, Godley LA (2017) Myeloid neoplams with germline predisposition. In: Swerdlow SH, Campo E, Lee Harris N, Jaffe ES, Pileri SA, Stein H, Thiele J (eds) WHO classification of tumours of haematopoietic and lymphoid tissues. Revised 4th Edition.edn. International Agency for Research on Cancer, Lyon, 121–128
Chen DH, Below JE, Shimamura A, Keel SB, Matsushita M, Wolff J, Sul Y, Bonkowski E, Castella M, Taniguchi T, Nickerson D, Papayannopoulou T, Bird TD, Raskind WH (2016) Ataxia-pancytopenia syndrome is caused by missense mutations in SAMD9L. Am J Hum Genet 98:1146–1158. https://doi.org/10.1016/j.ajhg.2016.04.009
Narumi S, Amano N, Ishii T, Katsumata N, Muroya K, Adachi M, Toyoshima K, Tanaka Y, Fukuzawa R, Miyako K, Kinjo S, Ohga S, Ihara K, Inoue H, Kinjo T, Hara T, Kohno M, Yamada S, Urano H, Kitagawa Y, Tsugawa K, Higa A, Miyawaki M, Okutani T, Kizaki Z, Hamada H, Kihara M, Shiga K, Yamaguchi T, Kenmochi M, Kitajima H, Fukami M, Shimizu A, Kudoh J, Shibata S, Okano H, Miyake N, Matsumoto N, Hasegawa T (2016) SAMD9 mutations cause a novel multisystem disorder, MIRAGE syndrome, and are associated with loss of chromosome 7. Nat Genet 48:792–797. https://doi.org/10.1038/ng.3569
Wlodarski MW, Hirabayashi S, Pastor V, Stary J, Hasle H, Masetti R, Dworzak M, Schmugge M, van den Heuvel-Eibrink M, Ussowicz M, De Moerloose B, Catala A, Smith OP, Sedlacek P, Lankester AC, Zecca M, Bordon V, Matthes-Martin S, Abrahamsson J, Kuhl JS, Sykora KW, Albert MH, Przychodzien B, Maciejewski JP, Schwarz S, Gohring G, Schlegelberger B, Cseh A, Noellke P, Yoshimi A, Locatelli F, Baumann I, Strahm B, Niemeyer CM, Ewog MDS (2016) Prevalence, clinical characteristics, and prognosis of GATA2-related myelodysplastic syndromes in children and adolescents. Blood 127:1387–1397. https://doi.org/10.1182/blood-2015-09-669937 (quiz 1518)
Sahoo SS, Pastor VB, Goodings C, Voss RK, Kozyra EJ, Szvetnik A, Noellke P, Dworzak M, Stary J, Locatelli F, Masetti R, Schmugge M, De Moerloose B, Catala A, Kallay K, Turkiewicz D, Hasle H, Buechner J, Jahnukainen K, Ussowicz M, Polychronopoulou S, Smith OP, Fabri O, Barzilai S, de Haas V, Baumann I, Schwarz-Furlan S, European Working Group of MDSiC, European Niewisch MR, Sauer MG, Burkhardt B, Lang P, Bader P, Beier R, Muller I, Albert MH, Meisel R, Schulz A, Cario G, Panda PK, Wehrle J, Hirabayashi S, Derecka M, Durruthy-Durruthy R, Gohring G, Yoshimi-Noellke A, Ku M, Lebrecht D, Erlacher M, Flotho C, Strahm B, Niemeyer CM, Wlodarski MW (2021) Clinical evolution, genetic landscape and trajectories of clonal hematopoiesis in SAMD9/SAMD9L syndromes. Nat Med 27:1806–1817. https://doi.org/10.1038/s41591-021-01511-6
Calvo KR, Vinh DC, Maric I, Wang W, Noel P, Stetler-Stevenson M, Arthur DC, Raffeld M, Dutra A, Pak E, Myung K, Hsu AP, Hickstein DD, Pittaluga S, Holland SM (2011) Myelodysplasia in autosomal dominant and sporadic monocytopenia immunodeficiency syndrome: diagnostic features and clinical implications. Haematologica 96:1221–1225. https://doi.org/10.3324/haematol.2011.041152
Spinner MA, Sanchez LA, Hsu AP, Shaw PA, Zerbe CS, Calvo KR, Arthur DC, Gu W, Gould CM, Brewer CC, Cowen EW, Freeman AF, Olivier KN, Uzel G, Zelazny AM, Daub JR, Spalding CD, Claypool RJ, Giri NK, Alter BP, Mace EM, Orange JS, Cuellar-Rodriguez J, Hickstein DD, Holland SM (2014) GATA2 deficiency: a protean disorder of hematopoiesis, lymphatics, and immunity. Blood 123:809–821. https://doi.org/10.1182/blood-2013-07-515528
Ganapathi KA, Townsley DM, Hsu AP, Arthur DC, Zerbe CS, Cuellar-Rodriguez J, Hickstein DD, Rosenzweig SD, Braylan RC, Young NS, Holland SM, Calvo KR (2015) GATA2 deficiency-associated bone marrow disorder differs from idiopathic aplastic anemia. Blood 125:56–70. https://doi.org/10.1182/blood-2014-06-580340
Wlodarski MW, Collin M, Horwitz MS (2017) GATA2 deficiency and related myeloid neoplasms. Semin Hematol 54:81–86. https://doi.org/10.1053/j.seminhematol.2017.05.002
Sahoo SS, Kozyra EJ, Wlodarski MW (2020) Germline predisposition in myeloid neoplasms: unique genetic and clinical features of GATA2 deficiency and SAMD9/SAMD9L syndromes. Best Pract Res Clin Haematol 33:101197. https://doi.org/10.1016/j.beha.2020.101197
Hasserjian RP, Orazi A, Brunning RD, Germing U, Le Beau MM, Porwit A, Baumann I, Hellström-Lindberg E, List AF, Cazzola M, Foucar K (2017) Myelodysplastic syndromes. In: Swerdlow SH, Campo E, Lee Harris N, Jaffe ES, Pileri SA, Stein H, Thiele J (eds) WHO classification of tumours of heamatopoietic and lymphoid tissues., Revised 4th edition.edn. International Agency for Researcht on Cancer, Lyon, 117–120
Niemeyer CM, Baumann I (2011) Classification of childhood aplastic anemia and myelodysplastic syndrome. Hematol Am Soc Hematol Educ Program 2011:84–89. https://doi.org/10.1182/asheducation-2011.1.84
Baumann I, Fuhrer M, Behrendt S, Campr V, Csomor J, Furlan I, de Haas V, Kerndrup G, Leguit RJ, De Paepe P, Noellke P, Niemeyer C, Schwarz S (2012) Morphological differentiation of severe aplastic anaemia from hypocellular refractory cytopenia of childhood: reproducibility of histopathological diagnostic criteria. Histopathology 61:10–17. https://doi.org/10.1111/j.1365-2559.2011.04156.x
Margolskee E, Hasserjian RP, Hassane D, Tam W, Mathew S, Ok CY, Wang SA, Oak J, Arber DA, Orazi A (2017) Myelodysplastic syndrome, unclassifiable (MDS-U) with 1% blasts is a distinct subgroup of MDS-U with a poor prognosis. Am J Clin Pathol 148:49–57. https://doi.org/10.1093/ajcp/aqx043
Bolouri H, Farrar JE, Triche T Jr, Ries RE, Lim EL, Alonzo TA, Ma Y, Moore R, Mungall AJ, Marra MA, Zhang J, Ma X, Liu Y, Liu Y, Auvil JMG, Davidsen TM, Gesuwan P, Hermida LC, Salhia B, Capone S, Ramsingh G, Zwaan CM, Noort S, Piccolo SR, Kolb EA, Gamis AS, Smith MA, Gerhard DS, Meshinchi S (2018) The molecular landscape of pediatric acute myeloid leukemia reveals recurrent structural alterations and age-specific mutational interactions. Nat Med 24:103–112. https://doi.org/10.1038/nm.4439
Rubnitz JE, Inaba H (2012) Childhood acute myeloid leukaemia. Br J Haematol 159:259–276. https://doi.org/10.1111/bjh.12040
Forestier E, Heim S, Blennow E, Borgström G, Holmgren G, Heinonen K, Johansson J, Kerndrup G, Andersen MK, Lundin C, Nordgren A, Rosenquist R, Swolin B, Johansson B, (NOPHO) NSoPHaO, (SCLSG) SCLSG, (NLCSG) NLCSG (2003) Cytogenetic abnormalities in childhood acute myeloid leukaemia: a Nordic series comprising all children enrolled in the NOPHO-93-AML trial between 1993 and 2001. Br J Haematol 121:566–577. https://doi.org/10.1046/j.1365-2141.2003.04349.x
Balgobind BV, Raimondi SC, Harbott J, Zimmermann M, Alonzo TA, Auvrignon A, Beverloo HB, Chang M, Creutzig U, Dworzak MN, Forestier E, Gibson B, Hasle H, Harrison CJ, Heerema NA, Kaspers GJ, Leszl A, Litvinko N, Nigro LL, Morimoto A, Perot C, Pieters R, Reinhardt D, Rubnitz JE, Smith FO, Stary J, Stasevich I, Strehl S, Taga T, Tomizawa D, Webb D, Zemanova Z, Zwaan CM, van den Heuvel-Eibrink MM (2009) Novel prognostic subgroups in childhood 11q23/MLL-rearranged acute myeloid leukemia: results of an international retrospective study. Blood 114:2489–2496. https://doi.org/10.1182/blood-2009-04-215152
Quessada J, Cuccuini W, Saultier P, Loosveld M, Harrison CJ, Lafage-Pochitaloff M (2021) Cytogenetics of pediatric acute myeloid leukemia: a review of the current knowledge. Genes (Basel) 12. https://doi.org/10.3390/genes12060924
Arber DA, Baumann I, Niemeyer C, Brunning RD, Porwit A (2017) Myeloid proliferations associated with Down syndrome. In: Swerdlow SH, Campo E, Lee Harris N, Jaffe ES, Pileri SA, Stein H, Thiele J (eds) WHO classification of tumours of haematopoietic and lymphoid tissues., Revised 4th edition.edn. International Agency for Research on Cancer, Lyon, 169–171
Mundschau G, Gurbuxani S, Gamis AS, Greene ME, Arceci RJ, Crispino JD (2003) Mutagenesis of GATA1 is an initiating event in Down syndrome leukemogenesis. Blood 101:4298–4300. https://doi.org/10.1182/blood-2002-12-3904
Wechsler J, Greene M, McDevitt MA, Anastasi J, Karp JE, Le Beau MM, Crispino JD (2002) Acquired mutations in GATA1 in the megakaryoblastic leukemia of Down syndrome. Nat Genet 32:148–152. https://doi.org/10.1038/ng955
Massey GV, Zipursky A, Chang MN, Doyle JJ, Nasim S, Taub JW, Ravindranath Y, Dahl G, Weinstein HJ, Children’s Oncology G (2006) A prospective study of the natural history of transient leukemia (TL) in neonates with Down syndrome (DS): Children’s Oncology Group (COG) study POG-9481. Blood 107:4606–4613. https://doi.org/10.1182/blood-2005-06-2448
Eidenschink Brodersen L, Alonzo TA, Menssen AJ, Gerbing RB, Pardo L, Voigt AP, Kahwash SB, Hirsch B, Raimondi S, Gamis AS, Meshinchi S, Loken MR (2016) A recurrent immunophenotype at diagnosis independently identifies high-risk pediatric acute myeloid leukemia: a report from Children’s Oncology Group. Leukemia 30:2077–2080. https://doi.org/10.1038/leu.2016.119
Niktoreh N, Walter C, Zimmermann M, von Neuhoff C, von Neuhoff N, Rasche M, Waack K, Creutzig U, Hanenberg H, Reinhardt D (2019) Mutated WT1, FLT3-ITD, and NUP98-NSD1 fusion in various combinations define a poor prognostic group in pediatric acute myeloid leukemia. J Oncol 2019:1609128. https://doi.org/10.1155/2019/1609128
de Rooij JD, Branstetter C, Ma J, Li Y, Walsh MP, Cheng J, Obulkasim A, Dang J, Easton J, Verboon LJ, Mulder HL, Zimmermann M, Koss C, Gupta P, Edmonson M, Rusch M, Lim JY, Reinhardt K, Pigazzi M, Song G, Yeoh AE, Shih LY, Liang DC, Halene S, Krause DS, Zhang J, Downing JR, Locatelli F, Reinhardt D, van den Heuvel-Eibrink MM, Zwaan CM, Fornerod M, Gruber TA (2017) Pediatric non-Down syndrome acute megakaryoblastic leukemia is characterized by distinct genomic subsets with varying outcomes. Nat Genet 49:451–456. https://doi.org/10.1038/ng.3772
Acknowledgements
The workshop panelists wish to thank the hosts for organizing the European Association of Haematopathology 2020 Virtual Meeting. The panel also likes to thank the case submitters for sharing their interesting and often challenging cases: Dr. K. Ofori, New York-Presbyterian Hospital/Columbia University Irving Medical Center, New York, USA (case 744); Dr. J. Wooldridge, Vagelos College of Physicians and Surgeons, Columbia University, New York, USA (case 743, case 730, case 723); Dr. Y-C. Liu, University of Pittsburgh School of Medicine, Pittsburgh, USA (case 505); Dr. S.M. Abd Own, Karolinska University Hospital, Stockholm, Sweden (case 722); Dr. A.A. Uner, Hacettepe, Ankara, Turkey (case 408), Dr. D.D. Grier, Cincinnati Children’s Hospital Medical Center, Cincinatti, USA (case 153 and 700); Dr. A. Kwiecinska, Karolinska University Hospital, Stockholm, Sweden (case 564); Dr. G. Gheorghe, Minnesota Childrens Hospital, Minneapolis, USA (case 602); Dr. M. Mays, Weill Cornell Medicine, New York, NY, USA (case 496); Dr. A. Orazi, TexasTech University Health Sciences Center, El Paso, TX, USA (case 678); Dr. B. Burroni, HOPITAL Cochin APHP, Paris, France (case 627); Dr. E. Margolskee, Children’s Hospital of Philadelphia, Philadelphia, PA, USA (case 182); Dr. K. Schafernak, Phoenix Children's Hospital, Phoenix, Arizona, USA (case 679); Dr. S. Gong, Northwestern University, Chicago, USA (case 521); Dr. J. Wang, Loma Linda University Medical Center, Loma Linda, Los Angeles, USA (case 279); Dr. B. Kaumeyer, University of Chicago, Chicago, USA (case 492); Dr. N. Zimmermann, Cincinnati Children’s Hospital, Cincinnati, United States (case 344); Dr. K. Petrova-Drus, Memoral Sloan Kettering Cancer Center, NY, USA (case 471); Dr. V. Hoang, Children’s Hospital Los Angeles, Los Angeles, USA (case 472); Dr. H. Fang, MD Anderson Cancer Center, Houston, USA (case 473); Dr. A. Shestakova, Children’s Hospital of Orange County, Orange, USA (case 689); Dr. J. Coviello, BAMC, Fort Sam Houston, USA (case 179); Dr. V. Nagrale, Sheikh Khalifa Medical City, Abu Dhabi, United Arab Emirates (case 779); Dr. S. Al-Khatib, Jordan University of Science and Technology, Irbid, Jordan (case 228); Dr. J. P. Kläger, Medical University of Vienna, Vienna, Austria (case 322), Dr. S.L.K. Laximanarayana, Kasturba Medical College, Manipal, Manipal Academy of Higher Education, Udupi, India (case 682); Dr. S. Sadigh, Massachusetts General Hospital, Boston, USA (case 329, case 282, case 361); Dr. V. Leventaki, Medical College of Wisconsin, Milwaukee, USA (case 754); Dr. G.K. Petrushevska, Medical faculty, UKIM, Skopje, Macedonia (case 545); Dr. L. Slonim, Northwestern University, Chicago, USA (case 503 and 511); Dr. A. Kaur, Northshore Health System, Chicago, USA (case 525); Dr. H. Tashkandi, University of Pittsburgh Medical Center, Pittsburgh, USA (case 677 and 726); Dr. K.A. Rozenova, Mayo Clinic, Rochester, USA (case 414); Dr. L. Saft, Karolinska University Hospital, Solna, Stockholm, Sweden (case 647); Dr. R.J. Leguit, University Medical Center Utrecht, Utrecht, the Netherlands (case 548); Dr. S. Loghavi, The University of Texas, MD Anderson Cancer Center, Houston, USA (case 583); Dr. A. Ruskova, Auckland city hospital, Auckland, NZL (case 187); Dr. S. Hussein, Mount Sinai Hospital, Icahn School of Medicine, New York, USA (case 766); Dr. L. Wang, University of California, San Francisco, USA (case 247); Dr. P. Kumar, St. Jude Children's Research Hospital, Memphis, USA (case 796); Dr. J. Reszec, Uniwersytet Medyczny w Białymstoku, Bialystok, Poland (case 773); Dr. C. Marcus, Beth Israel Deaconess Medical Center, Boston, USA (case 150); Dr. F. Liu, Foshan Hospital, Sun Yat-sen University, Foshan, China (case 522); Dr. H. Katerji, University of Rochester, Rochester, USA (case 630); Dr. G. Gasljevic, University Children's Hospital of Ljubljana, Ljubljana, Slovenia (case 523).
Author information
Authors and Affiliations
Contributions
All authors whose names appear on the submission (1) made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; (2) drafted the work or revised it critically for important intellectual content; (3) approved the version to be published; and (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Informed consent
Not applicable.
Conflict of interest
Only Dr. Kucine reports a possible conflict of interest: Member, Safety Monitoring Committee-Protagonist Therapeutics.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leguit, R.J., Orazi, A., Kucine, N. et al. EAHP 2020 workshop proceedings, pediatric myeloid neoplasms. Virchows Arch 481, 621–646 (2022). https://doi.org/10.1007/s00428-022-03375-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-022-03375-8