Abstract
Pancreatoblastoma (PB) is a rare tumor of the pancreas. In case of metastases, the treatment options are sparse and targeted approaches are not developed. We here evaluate MCL1 amplification as a putative target in PB.
Thirteen samples from adult (10/13) and pediatric patients (3/13) were collected. Three of these samples had been previously subjected to whole-exome sequencing (2 cases) or whole-genome sequencing (1 case) within a precision oncology program (NCT/DKTK MASTER), and this analysis had shown copy number gains of MCL1 gene. We established a fluorescence in situ hybridization (FISH) test to assess the copy number alterations of MCL1 gene in 13 formalin-fixed paraffin-embedded PBs, including the 3 cases assessed by genome sequencing. FISH analysis showed the amplification of MCL1 in 2 cases (both were adult PB), one of which was a case with the highest copy number gain at genomic analysis. In both cases, the average gene copy number per cell was ≥ 5.7 and the MCL1/1p12 ratio was ≥ 2.4. Our data support MCL1 as a putative target in PB. Patients with MCL1-amplified PB might benefit from MCL1 inhibition. Sequencing data is useful to screen for amplification; however, the established FISH for MCL1 can help to determine the level and cellular heterogeneity of MCL1 amplification more accurately.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatoblastoma (PB) is a very rare cancer but the most common malignant pancreatic tumor in young children [1]. It can also occur in adults at an even lower rate. Although PB seems to derive from the fetal anlage of pancreatic acinar cells and shows predominantly acinar differentiation, the exact origin of this tumor remains unclear [2]. Histologically, PB is a solid neoplasm with acinar differentiation and with the typical presence of squamoid nests, which represent its diagnostic hallmark. It is described as a slow-growing tumor [2] and the clinical presentation is unspecific with abdominal pain, mass effect, vomiting, and weight loss. When diagnosed, most tumors are rather large (> 5 cm) [1]. As a biomarker, alpha-fetoprotein (AFP) may be useful [3].
Complete surgical resection is the primary goal of the initial treatment which is feasible in the majority of cases [1]. Due to the high recurrence rate [4] and the fact that 17–35% of patients have metastases at the time of diagnosis [4, 5], (neoadjuvant) systemic chemotherapy is the therapy of choice. Most authors recommend cisplatin and doxorubicin (so-called PLADO schedule) based on anecdotal reference only given the rarity of the disease [1, 3].
Metastatic PB is associated with a dismal prognosis. Metastases primarily occur in the liver and less frequently in the lungs or regional lymph nodes [4]. The overall survival rates at 5 years for patients without metastases at presentation are 49% (95% confidence interval [CI], 31–66) and with metastases 25% (95% CI, 0–63). Post resection metastatic disease was associated with a significantly lower 5-year overall survival (21% [95% CI, 0–41] vs. 91% [95% CI, 83–100]). Collectively, these data demonstrate the need for additional therapeutic options. However, due to the rarity of this disease, clinical trials evaluating targeted therapies are neither feasible nor available.
Using next-generation sequencing (NGS) for metastatic PB from four adult patients (two samples were assessed by whole-exome sequencing, one sample by whole-genome sequencing, and one sample by targeted next-generation sequencing), Berger et al. identified molecular alterations that affected the FGFR signaling in three out of four patients which is potentially targetable and under current evaluation for different tumors [6]. The comprehensive sequencing identified a high-level amplification of MCL1 encoding induced myeloid leukemia cell differentiation protein 1 (MCL1) in three patients. MCL1 belongs to the anti-apoptotic group of Bcl-2 (B-cell lymphoma 2) proteins regulating apoptosis. It has been well characterized in several tumor entities [7, 8], and MCL1 inhibitors have shown efficacy in preclinical trials for hematological neoplasms [9, 10] and solid tumors [11,12,13]. The prevalence of MCL1 amplification in PB is unknown and might offer a rationale for targeted approaches with MCL1 inhibitors.
We here describe the analysis of MCL1 amplification using FISH in 13 assessable cases to estimate the prevalence of MCL1 amplification as potential biomarker in PB.
Materials and methods
Sample collection
This retrospective study was conducted on 13 formalin-fixed paraffin-embedded (FFPE) tumor samples from 13 patients with PB (Table 1). Three samples were obtained from the NCT/DKTK MASTER (Molecularly Aided Stratification for Tumor Eradication Research) cohort and previously published [6]. For whole-genome (patients 1 and 2), whole-exome (patient 3), or whole-transcriptome (patients 2 and 3) sequencing, fresh-frozen tissue specimens from the primary tumors of patients 1 and 3 as well as from a metastatic lesion of patient 2 were collected according to the standard protocols of the NCT/DKTK MASTER program [14, 15]. DNA extracted from buffy coats served as germline controls for the patients 3 and 2; a whole-blood sample was used for patient 1. Patients of the NCT/DKTK MASTER cohort gave written informed consent under protocol S-206/2011, which has been approved by the Ethics Committee of the University of Heidelberg. The present study was approved by the local Ethics Committee of the University Duisburg-Essen (20–9337-BO).
Next-generation sequencing and computational processing
The fresh-frozen tissue samples from patients 1 and 2 were subject to whole-exome sequencing (WES); the sample from patient 3 to whole-genome sequencing (WGS). In addition, we performed whole-transcriptome sequencing on the tumor/metastasis samples from patients 2 and 3. Library preparation, Illumina next-generation sequencing, and computational processing were carried out as described before [16].
Fluorescence in situ hybridization (FISH)
FFPE samples were processed by using the ZytoLight FISH-Tissue Implementation Kit and SPEC MCL1/1p12 Dual Color Probe (Zytovision-Z-2173–200, ZytoVision GmbH, Bremerhaven, Germany). FISH assays were basically performed as previously described [17]. Pepsin digestion was used for proteolysis. For FISH evaluation, the entire tumor area was scanned for amplification hot spots. If MCL1 signals showed a homogenous distribution, random areas were used for reading the slides. Twenty contiguous tumor cell nuclei from three areas, either hot spots or from randomly selected regions, resulting in a total of 60 nuclei, were individually evaluated by counting green MCL1 and orange 1p12 signals. MCL1/1p12 ratio and the average MCL1 copy number per cell were calculated and percentages of tumor cells with ≥ 4.0, ≥ 5.0, and ≥ 15.0 MCL1 copies were recorded. All FISH assays were evaluated by one reader (HUS) and who was blinded to sequencing results. Based on the observed distribution of parameters within our cohort and comparison with sequencing data (see below), MCL1 amplification was defined by a MCL1/1p12 ratio ≥ 2.0 and/or an average MCL1 copy number per tumor cell ≥ 5.0.
Results
High-level amplification of MCL1 in pancreatoblastoma in adult patients
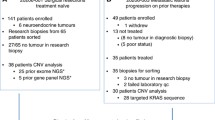
The NCT/DKTK MASTER (Molecularly Aided Stratification for Tumor Eradication Research), a multicenter, prospective observational study, analyzes tumors of advanced stage of young patients and rare tumors in search of potential therapeutic approaches [14, 15]. To date, four PBs were included and fresh-frozen tissue of three tumors was assessed by WES/WGS [6]. Analyzing all PB samples within NCT/DKTK MASTER for MCL1 alterations, copy number gains of MCL1 were observed in all three PBs with total copy numbers (TCN) of 5.83, 6.74, and 3.09 for patients 1 to 3, respectively. The chromosomal region corresponding with MCL1, 1q21.2 [18], was one of the most amplified regions in patient 3 and the highest in patients 1 and 2 (see Fig. 1).
High total copy number (TCN) indicating MCL1 amplification. Total copy number (TCN), degree of homozygosity, and B-Allele Frequency (BAF) for the three adult patients with metastatic pancreatoblastoma in the MASTER cohort. Compared to the other chromosomes, chromosome 1q is highly amplified in all three patients with TCN from 3.09 up to 6.74
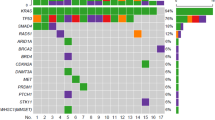
To further assess the amplification status of MCL1 in PB, we collected twelve additional cases, totaling eleven adult and four pediatric cases. Patients’ characteristics and FISH results are summarized in Table 1. FISH was performed on 13 samples (10 adult, 3 pediatric cases). Two samples were found to be positive for MCL1 amplification based on our established FISH criteria (see Fig. 2).
MCL1 FISH. a Pancreatoblastoma sample from an adult patient (H&E, original magnification: × 200). b MCL1 FISH. Orange signals label the reference locus on the short arm of chromosome 1 (1p12), green signals label a 575 kb chromosomal region on the long arm of chromosome 1 (1q21.3) including the MCL1 gene. This sample shows amplification of the MCL1 region. Non-neoplastic cells contain one or two orange or green signals
Assessing the NCT/DKTK MASTER samples, the sample with the highest TCN of 6.74 (patient 2) based on sequencing in the NCT/DKTK MASTER cohort also had a positive FISH result. MCL1/1p12 ratio was 2.5, average gene copy number was 5.7 per cell, and 80% of evaluated nuclei contained 5 or more MCL1 gene signals (93% ≥ 4.0 gene signals) (Fig. 1B). However, large signal clusters (≥ 15.0 gene signals per tumor cell) were not seen. Although the other two samples with sequencing data had TCN of 3.09 (patient 3) and 5.83 (patient 1), suggesting MCL1 amplification, the FISH were negative. Percentages of tumor cells with ≥ 4.0 gene copies were 2% and 20%, respectively, but MCL1/1p12 ratio was < 2.0 and average gene copy number was < 3.0 in both samples.
Analyzing the other ten samples without sequencing data, another sample fulfilled FISH criteria for MCL1 amplification (patient 10) with a MCL1/1p12 ratio of 2.6 (average gene copy number: 6.7, tumor cells with ≥ 4.0, ≥ 5.0, and ≥ 15.0 gene signals were 88%, 82%, and 0%, respectively). Signal distribution showed moderate to marked heterogeneity among tumor samples and between tissue blocks.
Overall, 2 out of 10 (20%) samples of adult patients were positive for MCL1 amplification, while no pediatric tumor showed amplification of MCL1 with the caveat that only few pediatric cases were included in our cohort. We are not aware of any association of MCL1 amplification with the clinical presentation including syndromal versus sporadic occurrence. Based on the NCT/DKTK MASTER inclusion criteria, patients with WES/WGS analyses were young adults (age range 18 to 50 years).
Discussion
Metastatic PB lacks therapeutic options. Identifying genetic biomarkers might help to find novel targeted treatment strategies. Here, we assessed a series of 13 PBs for MCL1 amplification by FISH after identification of amplified MCL1 in cases from the NCT/DKTK MASTER cohort. We show that two out of 13 samples (15%) were FISH positive for MCL1 amplification. Considering only samples from adult patients, the proportion of FISH positive cases increases to 20% (2/10). The exact frequency of MCL1 amplification among various clinical settings of PB patients still needs to be prospectively determined.
Currently, chemotherapy is the main therapeutic option in metastatic PB. The most common agents include cisplatin and doxorubicin [1, 3] whereas FOLFOX/FOLFIRINOX (folinic acid, fluorouracil, oxaliplatin with or without irinotecan) is also administered to adult patients with metastatic disease [6]. Although targeted agents are lacking, reported therapeutic targets include the Wnt/ß-catenin pathway, IGF2, and the R-spondin/LGR5/RNF43 module [19]. Berger et al. detected FGFR alterations in three out of four patients and thus inhibition of FGFR signaling pathway might be a reasonable therapeutic approach with reported efficacy in some other cancer entities with FGFR aberrations [20,21,22,23].
MCL1 could be a candidate for targeted therapies currently evaluated in clinical trials (i.e., NCT04178902, NCT02992483). Preclinical evidence showed promising results in hematologic neoplasia such as acute myelogenous leukemia [9, 24] and multiple myeloma [24] as well as in some solid cancers [25]. In lung cancer, the combination of trametinib (MEK inhibitor) and AM-4907 (MCL1 inhibitor) showed tumor regression in xenograft tumors [11]. Adding AM-4907 to docetaxel or trastuzumab prolonged survival and induced tumor regression in two triple-negative and one HER2-amplified PDX breast cancer models [26]. Given our results of two identified cases with high-level MCL1 amplification, MCL1 inhibitors might be a reasonable approach in MCL1-amplified PBs. Additionally, MCL1 inhibitors can be offered to patients where targeted therapies for the above-mentioned Wnt/ß-catenin pathway and R-spondin/LGR5/RNF43 module are lacking.
There remains uncertainty concerning the true proportion of PBs with MCL1 amplification, although our cohort comprising 13 analyzable patient samples can be regarded as one of the larger series for this very rare tumor. The rarity of PB renders comprehensive analyses in large cohorts difficult. Bigger consortia on rare cancers such as the EXPeRT [1] or the Italian TREP project [27] might help to determine the frequency. As most biomaterial in our sample set was considerably older, only basic clinical parameters could be retrieved.
FISH is an established and straight-forward applicable technique in clinical routine diagnostics for the detection of amplifications with the potential of prognostic or predictive biomarkers in various cancer entities [28,29,30,31,32], e.g., ERBB2 in breast and gastric cancer [33,34,35]. Criteria for amplification obtained by FISH need to be carefully established and are dependent on and specific for (i) the gene of interest and (ii) the tumor subtype. One approach to establish FISH positivity criteria is to analyze larger cohorts of a tumor entity and to describe the unbiased distribution of parameters. Thus, unequivocal amplification levels can be defined [28]. In this study, a larger cohort of PB samples was investigated by MCL1 FISH. Based on our observations, criteria for FISH positivity in PB could be defined (MCL1 amplification: MCL1/1p12 ratio ≥ 2.0 and/or average gene MCL1 count per tumor cell ≥ 5.0). By applying these criteria, we could identify two MCL1-amplified cases among ten evaluable PB samples from adult patients. One of these two FISH-positive samples was also sequenced in the NCT/DKTK MASTER cohort and had the highest total copy number for MCL1 of all sequenced PB samples. Although sequencing data showed higher TCN for MCL1 in the other two samples from the NCT/DKTK MASTER cohort, the MCL1 FISH did not confirm these results. First, lower values of TCN in patients 1 and 3 might be a reason. Second, technical issues might interfere with the analyses as fresh frozen tissue has to be strictly kept at less than − 80 °C and even short periods of more than − 80 °C might lead to degradation of the tissue. Moreover, another bias might come from the different tissues analyzed as the NGS data were acquired from fresh frozen tissue whereas the FISH analyses were performed on FFPE tissue. Third, other contributing factors may include sensitivity differences, clonal heterogeneity, sampling bias, and different tumoral ploidy. Intratumoral heterogeneity has been demonstrated in PB as well, and genetic heterogeneity seemed to be associated with morphologic differentiation lineages in a reported case of a PB patient [36]. We observed MCL1 amplification in cellular areas with more basophilic appearance. Further evaluations of larger case series, however, are needed to clarify potential associations between differentiation lineages and MCL1 amplification.
Based on our findings, we suggest utilizing WES/WGS or FISH for detecting MCL1 high level amplification in PBs to identify patients as potential candidates for a clinical trial or individual personalized treatment with MCL1 inhibitors. Also, other NGS applications including hybrid capture and amplicon-based NGS may be used if carefully established and validated on FFPE materials. If FISH is applied, we propose a potential definition for assay positivity. As a caveat, the predictive value of our approach remains to be validated with clinical treatment data. FISH as a technology has some clinical advantages since it is fast and works usually reliably with FFPE material even if tissue blocks contain only few tumor cells. Intratumoral heterogeneity was observed, which requires careful screening of tumor samples for amplification hotspots. Thus, we regard our definition of MCL1 FISH positivity as preliminary and a subject to potential adjustments. However, NGS-based findings should be validated by FISH analysis. This is why we suggest MCL1/1p12 ratio ≥ 2.0 and/or average MCL1 gene count per tumor cell ≥ 5.0 as reasonable selection criteria for potential targeted treatments since these criteria reflect the highest unequivocal amplification level based on our data from a larger series of adult and pediatric PBs. In contrast to sequencing methods, especially comprehensive ones such as whole-genome or whole-exome sequencing, FISH is a robust, cheap, fast, and easily applicable method which may be useful to identify patients potentially benefitting from targeted therapy.
In summary, FISH criteria were established and MCL1 amplification was identified in a subset of adult patients with PB. Given available MCL1 inhibitors, our study supports the rationale to test MCL1 amplification in a clinical setting to evaluate targeted treatment approaches.
Data availability
The data that support the findings of this study are available from the corresponding authors upon reasonable request.
References
Bien E, Godzinski J, Dall’Igna P et al (2011) Pancreatoblastoma: A report from the European cooperative study group for paediatric rare tumours (EXPeRT). Eur J Cancer 47:2347–2352. https://doi.org/10.1016/j.ejca.2011.05.022
Glick RD, Pashankar FD, Pappo A, LaQuaglia MP (2012) Management of pancreatoblastoma in children and young adults. J Pediatr Hematol Oncol 34:S47–S50. https://doi.org/10.1097/MPH.0b013e31824e3839
Défachelles AS, de Lassalle EM, Boutard P et al (2001) Pancreatoblastoma in childhood: clinical course and therapeutic management of seven patients. Med Pediatr Oncol 37:47–52. https://doi.org/10.1002/mpo.1162
Dhebri AR, Connor S, Campbell F et al (2004) Diagnosis, treatment and outcome of pancreatoblastoma. Pancreatology 4:441–453. https://doi.org/10.1159/000079823
Klimstra DS, Wenig BM, Adair CF, Heffess CS (1995) Pancreatoblastoma. A clinicopathologic study and review of the literature. Am J Surg Pathol 19:1371–1389. https://doi.org/10.1097/00000478-199512000-00005
Berger AK, Mughal SS, Allgäuer M et al (2020) Metastatic adult pancreatoblastoma: multimodal treatment and molecular characterization of a very rare disease. Pancreatology. https://doi.org/10.1016/j.pan.2020.02.017
Beroukhim R, Mermel CH, Porter D et al (2010) The landscape of somatic copy-number alteration across human cancers. Nature 463:899–905. https://doi.org/10.1038/nature08822
Czabotar PE, Lessene G, Strasser A, Adams JM (2014) Control of apoptosis by the BCL-2 protein family: implications for physiology and therapy. Nat Rev Mol Cell Biol 15:49–63. https://doi.org/10.1038/nrm3722
Ramsey HE, Fischer MA, Lee T et al (2018) A novel MCL1 inhibitor combined with venetoclax rescues venetoclax-resistant acute myelogenous leukemia. Cancer Discov 8:1566–1581. https://doi.org/10.1158/2159-8290.CD-18-0140
Caenepeel S, Brown SP, Belmontes B et al (2018) AMG 176, a selective MCL1 inhibitor, is effective in hematological cancer models alone and in combination with established therapies. Cancer Discov CD-18–0387. https://doi.org/10.1158/2159-8290.CD-18-0387
Nangia V, Siddiqui FM, Caenepeel S et al (2018) Exploiting MCL1 dependency with combination MEK + MCL1 inhibitors leads to induction of apoptosis and tumor regression in KRAS-mutant non–small cell lung cancer. Cancer Discov 8:1598–1613. https://doi.org/10.1158/2159-8290.CD-18-0277
Kotschy A, Szlavik Z, Murray J et al (2016) The MCL1 inhibitor S63845 is tolerable and effective in diverse cancer models. Nature 538:477–482. https://doi.org/10.1038/nature19830
Yasuda Y, Ozasa H, Kim YH et al (2020) MCL1 inhibition is effective against a subset of small-cell lung cancer with high MCL1 and low BCL-X L expression. Cell Death Dis 11:1–15. https://doi.org/10.1038/s41419-020-2379-2
Horak P, Klink B, Heining C et al (2017) Precision oncology based on omics data: The NCT Heidelberg experience. Int J Cancer 141:877–886. https://doi.org/10.1002/ijc.30828
Horak P, Heining C, Kreutzfeldt S et al (2021) Comprehensive genomic and transcriptomic analysis for guiding therapeutic decisions in patients with rare cancers. Cancer Discov candisc.0126.2021. https://doi.org/10.1158/2159-8290.CD-21-0126
Gröschel S, Hübschmann D, Raimondi F et al (2019) Defective homologous recombination DNA repair as therapeutic target in advanced chordoma. Nat Commun 10:1635. https://doi.org/10.1038/s41467-019-09633-9
Schildhaus H-U, Schultheis AM, Rüschoff J et al (2015) MET amplification status in therapy-naïve adeno- and squamous cell carcinomas of the lung. Clin Cancer Res Off J Am Assoc Cancer Res 21:907–915. https://doi.org/10.1158/1078-0432.CCR-14-0450
Craig RW, Jabs EW, Zhou P et al (1994) Human and mouse chromosomal mapping of the myeloid cell leukemia-1 gene: MCL1 maps to human chromosome 1q21, a region that is frequently altered in preneoplastic and neoplastic disease. Genomics 23:457–463. https://doi.org/10.1006/geno.1994.1523
Isobe T, Seki M, Yoshida K et al (2018) Integrated molecular characterization of the lethal pediatric cancer pancreatoblastoma. Cancer Res 78:865–876. https://doi.org/10.1158/0008-5472.CAN-17-2581
Loriot Y, Necchi A, Park SH et al (2019) Erdafitinib in locally advanced or metastatic urothelial carcinoma. N Engl J Med 381:338–348. https://doi.org/10.1056/NEJMoa1817323
Javle M, Lowery M, Shroff RT et al (2018) Phase II study of BGJ398 in patients with FGFR-altered advanced cholangiocarcinoma. J Clin Oncol 36:276–282. https://doi.org/10.1200/JCO.2017.75.5009
Schuler M, Cho BC, Sayehli CM et al (2019) Rogaratinib in patients with advanced cancers selected by FGFR mRNA expression: a phase 1 dose-escalation and dose-expansion study. Lancet Oncol 20:1454–1466. https://doi.org/10.1016/S1470-2045(19)30412-7
Abou-Alfa GK, Sahai V, Hollebecque A et al (2020) Pemigatinib for previously treated, locally advanced or metastatic cholangiocarcinoma: a multicentre, open-label, phase 2 study. Lancet Oncol 21:671–684. https://doi.org/10.1016/S1470-2045(20)30109-1
Tron AE, Belmonte MA, Adam A et al (2018) Discovery of Mcl-1-specific inhibitor AZD5991 and preclinical activity in multiple myeloma and acute myeloid leukemia. Nat Commun 9:5341. https://doi.org/10.1038/s41467-018-07551-w
Munkhbaatar E, Dietzen M, Agrawal D et al (2020) MCL-1 gains occur with high frequency in lung adenocarcinoma and can be targeted therapeutically. Nat Commun 11:4527. https://doi.org/10.1038/s41467-020-18372-1
Merino D, Whittle JR, Vaillant F et al (2017) Synergistic action of the MCL-1 inhibitor S63845 with current therapies in preclinical models of triple-negative and HER2-amplified breast cancer. Sci Transl Med 9:eaam7049. https://doi.org/10.1126/scitranslmed.aam7049
Dall’Igna P, Cecchetto G, Bisogno G et al (2010) Pancreatic tumors in children and adolescents: the Italian TREP project experience. Pediatr Blood Cancer 54:675–680. https://doi.org/10.1002/pbc.22385
Overbeck TR, Cron DA, Schmitz K et al (2020) Top-level MET gene copy number gain defines a subtype of poorly differentiated pulmonary adenocarcinomas with poor prognosis. Transl Lung Cancer Res 9:603–616. https://doi.org/10.21037/tlcr-19-339
Schmitz K, Koeppen H, Binot E et al (2015) MET gene copy number alterations and expression of MET and hepatocyte growth factor are potential biomarkers in angiosarcomas and undifferentiated pleomorphic sarcomas. PLoS One 10:e0120079. https://doi.org/10.1371/journal.pone.0120079
Schildhaus H-U, Heukamp LC, Merkelbach-Bruse S et al (2012) Definition of a fluorescence in-situ hybridization score identifies high- and low-level FGFR1 amplification types in squamous cell lung cancer. Mod Pathol Off J U S Can Acad Pathol Inc 25:1473–1480. https://doi.org/10.1038/modpathol.2012.102
Mentzel T, Schildhaus HU, Palmedo G et al (2012) Postradiation cutaneous angiosarcoma after treatment of breast carcinoma is characterized by MYC amplification in contrast to atypical vascular lesions after radiotherapy and control cases: clinicopathological, immunohistochemical and molecular analysis of 66 cases. Mod Pathol Off J U S Can Acad Pathol Inc 25:75–85. https://doi.org/10.1038/modpathol.2011.134
Schultheis AM, Bos M, Schmitz K et al (2014) Fibroblast growth factor receptor 1 (FGFR1) amplification is a potential therapeutic target in small-cell lung cancer. Mod Pathol Off J U S Can Acad Pathol Inc 27:214–221. https://doi.org/10.1038/modpathol.2013.141
Stoss OC, Scheel A, Nagelmeier I et al (2015) Impact of updated HER2 testing guidelines in breast cancer–re-evaluation of HERA trial fluorescence in situ hybridization data. Mod Pathol Off J U S Can Acad Pathol Inc 28:1528–1534. https://doi.org/10.1038/modpathol.2015.112
Rüschoff J, Nagelmeier I, Baretton G et al (2010) Her2 testing in gastric cancer. What is different in comparison to breast cancer? Pathol 31:208–217. https://doi.org/10.1007/s00292-010-1278-1
Schildhaus H-U, Schroeder L, Merkelbach-Bruse S et al (2013) Therapeutic strategies in male breast cancer: clinical implications of chromosome 17 gene alterations and molecular subtypes. Breast Edinb Scotl 22:1066–1071. https://doi.org/10.1016/j.breast.2013.08.008
Suemitsu Y, Ono Y, Mizukami Y et al (2021) A case of adult pancreatoblastoma with novel APC mutation and genetic heterogeneity. Front Oncol 11:725290. https://doi.org/10.3389/fonc.2021.725290
Acknowledgements
We thank all patients and their families for participation in the MASTER trial. We thank Nicole Bielefeld for technical assistance. The authors are grateful to Sophia Berger for expert technical support with the FISH assays.
Funding
Open Access funding enabled and organized by Projekt DEAL. P.J.J. received grant support by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation SFB 1335 (Project-ID 360372040)). J.T.S. is supported by the German Cancer Consortium (DKTK), the Deutsche Forschungsgemeinschaft (DFG) through grant SI1549/3–1 (Clinical Research Unit KFO337) and SI1549/4–1, the German Cancer Aid (#70112505/PIPAC, #70113834/PREDICT-PACA), and the Wilhelm Sander-Stiftung (2019.008.1). The sequencing analyses were supported by the NCT Molecular Diagnostics Program and grant 021 from the DKFZ-Heidelberg Center for Personalized Oncology. The contribution from University and Hospital Trust of Verona is supported by the Associazione Italiana Ricerca sul Cancro (AIRC 5 × 1000 n. 12182), Fondazione Cariverona: Oncology Biobank Project “Antonio Schiavi” (prot. 203885/2017), Fondazione Italiana Malattie Pancreas (FIMP-Ministero Salute J38D19000690001), and Italian Ministry of Health (RF CO-2019–12369662: CUP: B39C21000370001).
Author information
Authors and Affiliations
Contributions
PJJ, SF, HUS, and JTS conceived and designed the study. ASc, MA, VA, ASt, RTL, PJ, and GK provided resources. TMR, SU, CL, CV, HUS, and JTS performed the investigations/computations and acquired data. TMR, SU, STL, CL, CV, MA, ASc, ASt, HUS, and JTS analyzed and interpreted the data. TMR and SU prepared and wrote the original draft. TMR, STL, HUS, and JTS reviewed and edited the manuscript. HUS and JTS supervised the project. SF, HUS, and JTS acquired financial support for this project. HUS and JTS are the guarantors of this work and, as such, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors were involved in the critical review of the manuscript and approved the final version.
Corresponding authors
Ethics declarations
Ethics approval/consent to participate
Patients of the NCT/DKTK MASTER cohort gave written informed consent under protocol S-206/2011, which has been approved by the Ethics Committee of the University of Heidelberg. The present study was approved by the local Ethics Committee of the University Duisburg-Essen (20–9337-BO).
Competing interests
PJJ: Abbvie, Ariad, Bayer, Boehringer, Janssen (Johnson and Johnson), Novartis, Pfizer, Servier, Roche, BMS/Celgene (consulting or advisory role); Abbvie, Ariad, Bayer, Boehringer, Janssen (Johnson and Johnson), Novartis, Pfizer, Servier, Roche, BMS/Celgene (honoraria); Abbvie, Boehringer, Novartis, Roche, BMS/Celgene (research funding); Bayer, Boehringer, Janssen (Johnson and Johnson), MSD, Novartis, Pfizer, Pierre Fabre, Servier, Roche, BMS/Celgene (online registration/travel/accommodation).
SF: Consulting or advisory board membership: Bayer, Illumina, Roche; honoraria: Amgen, Eli Lilly, PharmaMar, Roche; research funding: AstraZeneca, Pfizer, PharmaMar, Roche; travel or accommodation expenses: Amgen, Eli Lilly, Illumina, PharmaMar, Roche.
ASt: Advisory Board/Speaker’s Bureau: Astra Zeneca, AGCT, Bayer, BMS, Eli Lilly, Illumina, Janssen, MSD, Novartis, Pfizer, Roche, Seattle Genetics, Takeda, Thermo Fisher. Grants: Bayer, BMS, Chugai.
HUS: Targos Molecular Pathology, Inc. (employment); Roche, Novartis Oncology, MSD, BMS, Pfizer, ZytoVision, Zytomed (honoraria); AstraZeneca, Agilent, Molecular Health, MSD (advisory boards); Novartis Oncology (research funding—outside of this study).
JTS: Bristol-Myers Squibb, Celgene, Roche (research funding—outside of this study); AstraZeneca, Bayer, Bristol-Myers Squibb, Celgene, Immunocore, Novartis, Roche, Shire (consulting or advisory role); AstraZeneca, Aurikamed, Baxalta, Bristol-Myers Squibb, Celgene, Falk Foundation, iomedico, Immunocore, Novartis, Roche, Shire (honoraria); minor equity in iTheranostics and Pharma15 and member of the Board of Directors for Pharma15 outside the submitted work.
All remaining authors declare no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Reissig, T.M., Uhrig, S., Jost, P.J. et al. MCL1 as putative target in pancreatoblastoma. Virchows Arch 481, 265–272 (2022). https://doi.org/10.1007/s00428-022-03349-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-022-03349-w