Abstract
Tumor budding is a long-established independent adverse prognostic marker in colorectal cancer, yet methods for its assessment have varied widely. In an effort to standardize its reporting, a group of experts met in Bern, Switzerland, in 2016 to reach consensus on a single, international, evidence-based method for tumor budding assessment and reporting (International Tumor Budding Consensus Conference [ITBCC]). Tumor budding assessment using the ITBCC criteria has been validated in large cohorts of cancer patients and incorporated into several international colorectal cancer pathology and clinical guidelines. With the wider reporting of tumor budding, new issues have emerged that require further clarification. To better inform researchers and health-care professionals on these issues, an international group of experts in gastrointestinal pathology participated in a modified Delphi process to generate consensus and highlight areas requiring further research. This effort serves to re-affirm the importance of tumor budding in colorectal cancer and support its continued use in routine clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The phenomenon of tumor budding (TB), defined as single cells and isolated cells clusters up to 4 cells at the tumor invasive front, has captured the interest of pathologists, clinicians, and researchers since it was first described in the 1950s [1]. A large body of evidence has since firmly established TB as a strong and independent predictor of lymph node metastasis (LNM), disease recurrence, and cancer-related death in patients with colorectal cancer (CRC) [2]. Despite wide variation in the criteria, methods, and reporting systems for the assessment of TB across different studies, TB has proved a remarkably consistent predictor of adverse outcome in CRC. However, until recently, the absence of a standardized scoring system made it difficult to implement TB in routine pathology practice. This prompted a group of international experts to meet in Bern, Switzerland, in 2016 to host the International Tumor Budding Consensus Conference (ITBCC) to reach consensus on a single, evidence-based method for TB assessment and reporting in CRC [3]. Since the publication of the ITBCC consensus recommendations in 2017, TB has been incorporated as an additional prognostic factor in the World Health Organization Classification of Tumors (2019), the Tumor, Nodes, Metastasis (TNM) staging system, and included in the reporting guidelines and protocols of the College of American Pathologists (CAP) [4], the National Comprehensive Cancer Network (NCCN) [5], and the International Collaboration on Cancer Reporting [6]. The ITBCC recommendations have since been validated in several large cohorts of colorectal cancer and a prospective multi-center clinical trial [7,8,9,10,11,12]. With the wider application of TB in both the research setting and clinical practice, several issues have emerged which require further clarification. Some relate to aspects of TB assessment, risk stratification based on TB in different clinical scenarios, and the relationship of TB to other biomarkers at the invasive front. Since the ITBCC recommendations were not intended to be an end point, but rather a foundation for further research, refinement, and periodic review, its members organized a modified Delphi consensus process. The aim of this effort was to reach consensus on a number of emerging issues, ongoing challenges, and areas in need of further research.
Material and methods
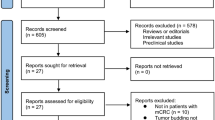
A group of 27 international pathologists with expertise in colorectal cancer pathology were invited to participate in the Delphi consensus survey. A total of 14 experts agreed to participate. The format of the consensus process is outlined in Fig. 1. The survey implemented an adapted version of the original Delphi method [13], which is designed to achieve consensus among a group of experts using a series of surveys. Based on a review of the TB literature (Supplementary Data Figure 1), two independent non-voting moderators (I.N and A.L) generated the Round 1 questionnaire consisting of a series of general questions and consensus statements. Rather than using open-ended questions in the first round, as has been done in other studies, general questions and agree/disagree statements were used. The general questions related to the implementation of TB by pathologists, the awareness of TB among clinicians, and the application of TB in clinical decision-making at the experts’ institutions.
The consensus statements solicited the experts’ opinions regarding the assessment and reporting of TB, its clinical application (particularly in malignant colorectal polyps (pT1) and stage II CRC), and its relationship to other biomarkers at the invasive front. The moderators disseminated the questionnaire to the participants using SurveyMonkey on August 7, 2019. Participants were able to provide commentary on questions to support their responses or express a particular opinion. Participants were also able to state “no opinion” on consensus statements. Individual votes were anonymized, and a consensus was considered achieved when ≥70% of participants either agreed/strongly agreed or disagreed/strongly disagreed with the statement. After the results of Round 1 were gathered, the moderators reviewed the results. Statements which did not achieve consensus (Supplementary Data Table 1) were later re-formulated and used by the moderators to generate new consensus statements for the next round of questioning.
An in-person meeting with the participants of the survey took place in Nice, France, on September 10, 2019. Prior to the meeting, an e-book containing all relevant TB studies published since ITBCC 2016 (Supplementary Data Figure 1) was circulated to the participants to ensure that all were familiar with new evidence related to TB in CRC. Participants were asked to review the e-book prior to the meeting. At the meeting, the results of the first round of the survey were presented by the moderators, and all questions and statements were then opened to discussion and debate among participants. Opinions expressed during this discussion as well as the statements not achieving consensus (Supplementary Data Table 1) were later used by the moderators to formulate new consensus statements for the next round of questioning. The moderators generated the statements for Round 2 and disseminated them on December 19, 2019. The statements which did not achieve consensus (Supplementary Data Table 2) and corresponding commentary for Round 2 were used to generate new consensus statements for the next round. This yielded a final series of 10 consensus statements for Round 3 which were sent out on February 3, 2020. A final consensus analysis was conducted and incorporated all consensus statements achieving consensus as well as statements which could not achieve consensus by Round 3 (11 from Round 1, 6 from Round 2, and 10 from Round 3).
Results
All 14 experts who agreed to participate in the study completed all three rounds of the Delphi consensus process. The results are depicted in a flowchart outlining the survey process (Fig. 1). A total of 23 statements reached a consensus, while 4 did not.
General
In the first round, participants received a series of 8 general questions regarding the implementation, clinician awareness, and clinical use of TB in their clinical practice (Fig. 2). Eighty-five percent of participants indicated that they routinely report TB in both pT1 and stage II CRC, while 64% and 43% indicated that scoring of TB was included in their national guidelines for pT1 and stage II CRC, respectively (I, V, II, VI). Seventy-nine and 64 percent indicated that their clinicians are aware of the relevance of TB in pT1 and stage II CRCs, respectively (III, VII), while 50% and 15% indicated that TB is taken into account in clinical decision-making for pT1 and stage II CRCs, respectively (IV, VIII).
Consensus statements
The final consensus statements are listed graphically to depict consensus and levels of agreement among experts with corresponding no opinion votes per statement (Fig. 3).
Consensus statements. Results of Delphi study after final consensus analysis. Each statement has a corresponding bar graph where the level of agreement/disagreement (%) is depicted. Statements are ranked within each subcategory from greatest to least degree of consensus. No opinion (N/A) votes are votes considered neither agree nor disagree for all corresponding consensus statements. All experts were able to vote “no opinion” on each statement. *Statements which did not achieve consensus
Definition and assessment
There was consensus that the definition of TB and its method of assessment and scoring as recommended by the ITBCC remains useful and should be retained and that there was no new evidence to support modifying this definition (#1, #8, Box 1, Fig. 4). There is also an agreement that using digital pathology algorithms may help with the implementation of tumor budding within the clinical workflow (#6).

Tumor budding scores. Examples of different tumor budding scores (hotspot, 0.785 mm2) at the invasive front of colorectal cancer based on the ITBCC 2016. a Bd1 (low), b Bd2 (intermediate), c Bd3 (high). Each case was re-stained with pan-cytokeratin (AE1/AE3), and the same region is depicted on the right. Arrows indicate tumor budding. Scale bar = 125 μm
Several questions addressed challenges related to TB assessment in areas with substantial inflammation which can result in tumor fragmentation mimicking TB or can obscure true TB. Ninety three percent of participants agreed that TB counting should be avoided in areas of tumor/glandular fragmentation caused by heavy inflammation (#2). Seventy-nine percent supported the term “pseudobudding” (defined as individual cells or small groups of cells resulting from fragmentation of glands secondary to inflammation) to describe this phenomenon, which likely differs biologically from TB (#5) (Fig. 5). Seventy-nine percent indicated that inflammation often hinders their assessment of TB on H&E (#7), while 71% indicated that they use pan-cytokeratin immunohistochemistry (IHC) in this setting to better visualize TB (#9), with final bud counting performed on H&E.
Clinical scenarios
-
(1)
Malignant colorectal polyps (pT1)
With regard to TB in pT1 CRC, there was unanimous (100%) agreement that clinicians should be aware of its relevance and that TB should be included in national guidelines (#12, #13). Ninety-three percent felt that TB should be routinely scored and that clinicians should take TB into account in clinical decision-making after local resection of pT1 CRC (#14, #15). If TB (Bd2/Bd3) was the only risk factor present, the need for additional surgical resection should be discussed in a multidisciplinary meeting in which additional clinical factors should also be considered (#16). Experts agreed that when low TB (Bd1) is observed in pT1 CRC cases with no other risk factors present, surgical resection is not advised as the risk of LNM is considered very low (#17).
-
(2)
Stage II colorectal carcinoma
With regard to TB in stage II CRC, there was strong consensus that TB should be routinely scored and that clinicians should be aware of its relevance (93% agreement) (#21, #20), while 79% agreed that TB should be included in national guidelines (#22). Seventy-nine percent of participants also agreed that if TB were the only risk factor in stage II CRC, then this should be considered a high-risk stage II CRC (#23). Participants did not reach consensus on whether clinicians should make decisions based solely on TB in stage II CRC (#24).
Poorly differentiated clusters (PDCs)
PDCs are clusters of cancer cells in the stroma composed of five or more cells and which lack a glandular structure [14]. There was consensus that TB and PDC are different and should not be combined within one definition (in keeping with ITBCC recommendations) (#25). There was also consensus that TB may arise from the main tumor mass and/or PDCs (#26).
Discussion
This survey, using a modified Delphi process and a panel of 14 experts in gastrointestinal pathology, was undertaken to evaluate new evidence related to TB, establish consensus on best practice, and identify areas in need of future research. The survey effectively generated consensus on several aspects of TB, the most important of which are discussed below.
There was strong consensus that TB scoring based on the ITBCC recommendations remains effective and should be used in daily practice for malignant colorectal polyps (pT1) and stage II CRC. This was underpinned by several large published studies validating the ITBCC recommendations [7,8,9,10,11,12] and the absence of any new evidence suggesting the need for their modification.
There was consensus that heavy inflammation at the invasive front often poses challenges in TB assessment. These challenges may be a consequence of tumor fragmentation by inflammatory cells resulting in detached tumor cells that may be mistaken for TB (“pseudobudding”) or due to inflammatory cells obscuring or mimicking TB. There was agreement that the term “pseudobudding” should apply to small groups of cells (maximum 4) that occur due to external influences such as inflammation and mechanical causes such as cutting artifacts. From a practical perspective, true tumor buds infiltrate the peritumoral stroma, while pseudobuds are typically surrounded by a mix of inflammatory cells, lack overt stromal infiltration, and tend to be limited to the immediate vicinity of fragmented glands/tumor nests (often following their original contours). Their biology likely differs from that of true TB since they are assumed to result from a reactive rather than active process; moreover, the heavy inflammation that produces pseudobudding is a feature generally associated with favorable outcomes. For these reasons, there was broad consensus that TB counting should be avoided in areas showing pseudobudding. Further studies need to be conducted to provide molecular evidence for the distinction between tumor budding and psuedobudding.
It is worth noting that pan-cytokeratin IHC can be misleading in the context of pseudobudding, since individual keratin positive cells can be mistaken for TB when viewed without morphologic context. Therefore, keratin stains are probably best avoided when the H&E features suggest pseudobudding. A recent study suggests that cancer gland rupture may be linked to LNM in pT1 CRC [15], but this remains to be confirmed by other groups. Until the relationship between gland rupture, TB, and LNM is better understood, pseudobudding should be excluded from the TB assessment. Finally, heavy inflammatory infiltrates may sometimes obscure TB, while reactive inflammatory and stromal cells can be difficult to distinguish from TB. In this setting, pan-cytokeratin IHC can be very helpful to better visualize TB, although the final bud count should be performed on H&E. Most participants indicated that they use pan-cytokeratin IHC in this scenario to aid visualization of TB.
The role of IHC alone in TB scoring remains controversial, with most participants indicating that more evidence is required before this can be considered routine practice. There was consensus that criteria for TB scoring based on IHC would need to differ from those based on H&E [16] since higher thresholds must be reached before TB assessed by H&E assumes prognostic significance [17, 18]. In addition, risk stratification does not appear to be improved with the use of IHC [16]. Some studies have shown improved reproducibility in TB scoring with IHC compared to H&E [19, 20], while others have not [21, 22]. While pan-cytokeratin IHC increases the sensitivity of TB detection, it is also associated with its own unique challenges. In particular, the nuclei of tumor buds are not always clearly visualized on IHC. This can be problematic if the presence of a nucleus is used as a minimum criterion for a tumor bud, as proposed in some studies [16]. Moreover, pseudobudding produced by inflammation-induced fragmentation, mechanical causes, or treatment may be difficult to distinguish from true TB on IHC stains alone since these may not capture the morphologic context. These challenges might explain the only moderate interobserver agreement reported among expert gastrointestinal pathologists at the individual tumor bud level, which was no better for pan-cytokeratin than for H&E [16]. Overall, most studies have shown TB scoring assessed with either IHC or H&E to be in the moderate or substantial range [21, 23,24,25,26], although this may be lower among non-subspecialist GI pathologists [27].
With regard to locally resected pT1 cancers, there was strong consensus that TB scoring should be routinely performed in practice, incorporated in national guidelines, and be factored into clinical decision-making. This is supported by strong evidence establishing intermediate and high TB (Bd2/Bd3) as independent predictors of LNM in pT1 CRC [28,29,30]. There was also consensus that locally resected pT1 cancers, in which intermediate or high TB was the only high-risk feature, should be discussed in a multidisciplinary meeting. In such cases, the decision regarding the need for surgical resection should take into account clinical factors, including operative risk and comorbidities, in order to balance the risks of over- and under-treatment. In pT1 cancers without TB (Bd1) or any other adverse risk factors, the risk of LNM is very low, and endoscopic resection is generally considered sufficient [31].
With regard to stage II CRC, there was consensus that TB scoring should be performed in daily practice, that TB should be included in national guidelines, and that clinicians be aware of its presence. There was also consensus that CRC with high TB (Bd3) should be considered at high risk for subsequent recurrence. This reflects strong evidence that high TB (Bd3) is an independent predictor of recurrence and mortality in stage II CRC [24, 32,33,34,35,36]. Consensus was not reached on whether clinical decisions should be made on the basis of TB alone in this setting. Adjuvant chemotherapy is currently not recommended for stage II CRC without high-risk features since the absolute benefits have been shown to be very small [37]. However, most oncology guidelines recommend that adjuvant chemotherapy be considered with high-risk stage II CRC [38]. Data from QUASAR [37] and SACURA [12] trials confirm the adverse prognostic value of TB in large cohorts of stage II CRC and suggest adjuvant chemotherapy may be beneficial in such patients. However, further prospective clinical trials are needed to confirm the benefit of adjuvant chemotherapy in stage II CRC with high TB.
The significance of the Bd2 category in the 3-tiered ITBCC scoring system is a potential source of confusion and may require some clarification. The Bd2 category assumes differing prognostic significance depending on the clinical scenario (i.e., pT1 or stage II CRC). Given the strong evidence that 5 or more tumor buds in a 0.785mm2 field is an independent predictor of LNM in pT1 CRC, Bd2 is considered a “high risk” in this setting. In contrast, in stage II CRC, the most significant risk for recurrence and mortality is seen when TB counts reach 10 or more (i.e., Bd3). As such, the Bd2 category is not considered a “high-risk” category in stage II CRC. Most participants (64%) agreed with the statement that “Bd2 can be considered either part of low TB (Stage II CRC) or high TB (pT1 CRC),” while 29% expressed “no opinion” and 7% disagreed. The lack of consensus on this statement may reflect the fact that Bd2, while not “high risk” in stage II, is not strictly “low risk” either, since the risk is intermediate between Bd1 and Bd3. However, for practical purposes, in pT1 CRC, Bd2 should be considered a risk factor for LNM, while in stage II CRC, Bd2 is not considered a high-risk feature.
TB shares several features in common with poorly differentiated clusters (PDC) from which they are distinguished by an arbitrary numerical cut-off (PDCs are defined as clusters of 5 or more tumor cells lacking glandular structure). PDCs have gained increasing recognition as an invasive front prognostic marker in CRC [39]. It has been suggested that PDC and TB may be part of a biologic continuum and reflect different stages of cancer cell invasion (#26). Although some studies have shown PDCs and TB to share biological similarities [40, 41], their relationship requires further investigation. There was consensus that, until more evidence regarding their underlying biology is available, TB and PDCs are best considered different and evaluated separately. It was acknowledged, however, that TB may arise from PDCs in addition to the main tumor mass.
Automated detection algorithms for TB, applied to either H&E- or IHC-stained sections, could prove effective in advancing our knowledge of TB and incorporating TB into routine clinical practice. Examples of these algorithms for TB in IHC have begun to emerge [42], yet there is still a need for a reliable algorithm that can automatically detect TB on H&E. There are several ways in which the digital interpretation of TB could help pathologists, such as detecting TB across an entire tissue slide, identifying hotspot areas, and potentially providing a TB score automatically. This will not come without its share of challenges but may serve to improve the efficiency, accuracy, and reproducibility of TB scoring which are all barriers to widespread implementation currently. In the research setting, digital interpretation of TB can help provide insight into how peritumoral budding, which is TB at the invasive margin, compares with intratumoral budding, which is TB within the tumor bulk [43]. How TB compares to PDCs prognostically, how current scoring cut-offs are set, and more dynamic scoring systems, such as continuous scaling method or scoring within multiple hotspots, can also be explored.
Lastly, a number of unresolved issues related to TB have been identified which require further research (Box 2). In conclusion, the standardized assessment and scoring system for TB established by the ITBCC 2016 have been incorporated into a number of international CRC guidelines and validated in large cohorts of CRC patients. We used a modified Delphi survey and in-person meeting to evaluate new evidence, generate consensus on a number of issues related to TB in CRC, and highlight areas in need of further research. This process has re-affirmed the importance of TB in CRC and supports its continued use in routine clinical practice. New technologies such as automated detection algorithms will be critical to improving the way TB assessment is conducted and implemented in clinical practice.

References
Imai (1954) The growth of human carcinoma: a morphological analysis. Fukuoka Igaku Zasshi 45:30
Lugli A, Zlobec I, Berger MD, Kirsch R, Nagtegaal ID (2020) Tumour budding in solid cancers. Nat Rev Clin Oncol. https://doi.org/10.1038/s41571-020-0422-y
Lugli A, Kirsch R, Ajioka Y, Bosman F, Cathomas G, Dawson H, El Zimaity H, Flejou JF, Hansen TP, Hartmann A, Kakar S, Langner C, Nagtegaal I, Puppa G, Riddell R, Ristimaki A, Sheahan K, Smyrk T, Sugihara K, Terris B, Ueno H, Vieth M, Zlobec I, Quirke P (2017) Recommendations for reporting tumor budding in colorectal cancer based on the International Tumor Budding Consensus Conference (ITBCC) 2016. Mod Pathol 30:1299–1311. https://doi.org/10.1038/modpathol.2017.46
Kakar S, Chanjuan S, Mariana BE, Driman DK, Fitzgibbons P, Frankel W, Hill KA, Jessup J, Krasinskas AM, Washington MK (2017) Protocol for the examination of specimens from patients with primary carcinoma of the colon and rectum. https://documents.cap.org/protocols/cp-gilower-colonrectum-17protocol-4010.pdf. Accessed October 2020
Benson A., Venook AP, Cederquist L ea (2020) National Comprehensive Cancer Network. Clinical practice guidelines in oncology (NCCN guidelines): colon cancer. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed October 2020
Loughrey MB, Arends M, Brown I, Burgart LJ, Cunningham C, Flejou JF, Kakar S, Kirsch R, Kojima M, Lugli A, Rosty C, Sheahan K, West NP, Wilson R, Nagtegaal I (2020) Colorectal cancer histopathology reporting guide. International Collaboration on Cancer Reporting. Sydney, Australia
Lang-Schwarz C, Melcher B, Haumaier F, Schneider-Fuchs A, Lang-Schwarz K, Krugmann J, Vieth M, Sterlacci W (2019) Budding, tumor-infiltrating lymphocytes, gland formation: scoring leads to new prognostic groups in World Health Organization low-grade colorectal cancer with impact on survival. Hum Pathol 89:81–89. https://doi.org/10.1016/j.humpath.2019.04.006
Landau MA, Zhu B, Akwuole FN, Pai RK (2019) Histopathological predictors of recurrence in stage III colon cancer: reappraisal of tumor deposits and tumor budding using AJCC8 criteria. Int J Surg Pathol 27:147–158. https://doi.org/10.1177/1066896918787275
van Wyk HC, Roseweir A, Alexander P, Park JH, Horgan PG, McMillan DC, Edwards J (2019) The relationship between tumor budding, tumor microenvironment, and survival in patients with primary operable colorectal cancer. Ann Surg Oncol 26:4397–4404. https://doi.org/10.1245/s10434-019-07931-6
Blank A, Schenker C, Dawson H, Beldi G, Zlobec I, Lugli A (2019) Evaluation of tumor budding in primary colorectal cancer and corresponding liver metastases based on H&E and pancytokeratin staining. Front Med (Lausanne) 6:247. https://doi.org/10.3389/fmed.2019.00247
Dawson H, Galuppini F, Trager P, Berger MD, Studer P, Brugger L, Zlobec I, Inderbitzin D, Lugli A (2019) Validation of the International Tumor Budding Consensus Conference 2016 recommendations on tumor budding in stage I-IV colorectal cancer. Hum Pathol 85:145–151. https://doi.org/10.1016/j.humpath.2018.10.023
Ueno H, Ishiguro M, Nakatani E, Ishikawa T, Uetake H, Matsuda C, Nakamoto Y, Kotake M, Kurachi K, Egawa T, Yasumasa K, Murata K, Ikawa O (2019) Prospective multicenter study on the prognostic and predictive impact of tumor budding in stage II colon cancer: results from the SACURA Trial. J Clin Oncol 37:1886–1894. https://doi.org/10.1200/JCO.18
Gordon TJ (1994) The Delphi method. Futur Res Methodol 4:2–15
Ueno H, Kajiwara Y, Shimazaki H, Shinto E, Hashiguchi Y, Nakanishi K, Maekawa K, Katsurada Y, Nakamura T, Mochizuki H, Yamamoto J, Hase K (2012) New criteria for histologic grading of colorectal cancer. Am J Surg Pathol 32
Oishi K, Ito T, Sakonishi D, Uchida K, Sekine M, Negi M, Kobayashi D, Miura K, Akashi T, Eishi Y (2019) Cancer gland rupture as a potential risk factor for lymph node metastasis in early colorectal adenocarcinoma with deep submucosal invasion. Histopathology. https://doi.org/10.1111/his.14022
Bokhorst JM, Blank A, Lugli A, Zlobec I, Dawson H, Vieth M, Rijstenberg LL, Brockmoeller S, Urbanowicz M, Flejou JF, Kirsch R, Ciompi F, van der Laak J, Nagtegaal ID (2020) Assessment of individual tumor buds using keratin immunohistochemistry: moderate interobserver agreement suggests a role for machine learning. Mod Pathol 33:825–833. https://doi.org/10.1038/s41379-019-0434-2
Martinez-Ciarpaglini C, Fernandez-Sellers C, Tarazona N, Rosello S, Huerta M, Roda D, Mongort C, Ferrandez A, Navarro S, Cervantes A (2019) Improving tumour budding evaluation in colon cancer by extending the assessment area in colectomy specimens. Histopathology 75:517–525. https://doi.org/10.1111/his.13900
Mitrovic B, Schaeffer DF, Riddell RH, Kirsch R (2012) Tumor budding in colorectal carcinoma: time to take notice. Mod Pathol 25:1315–1325. https://doi.org/10.1038/modpathol.2012.94
Koelzer VH, Zlobec I, Berger MD, Cathomas G, Dawson H, Dirschmid K, Hadrich M, Inderbitzin D, Offner F, Puppa G, Seelentag W, Schnuriger B, Tornillo L, Lugli A (2015) Tumor budding in colorectal cancer revisited: results of a multicenter interobserver study. Virchows Arch 466:485–493. https://doi.org/10.1007/s00428-015-1740-9
Kai K, Aishima S, Aoki S, Takase Y, Uchihashi K, Masuda M, Nishijima-Matsunobu A, Yamamoto M, Ide K, Nakayama A, Yamasaki M, Toda S (2016) Cytokeratin immunohistochemistry improves interobserver variability between unskilled pathologists in the evaluation of tumor budding in T1 colorectal cancer. Pathol Int 66:75–82. https://doi.org/10.1111/pin.12374
Suzuki A, Togashi K, Nokubi M, Koinuma K, Yasuyuki M, Horie H, Lefor AT, Yasuda Y (2009) Evaluation of venous invasion by Elastica van Gieson stain and tumor budding predicts local and distant metastases in patients with T1 stage colorectal cancer. Am J Surg Pathol 33:1601–1607
Puppa G, Senore C, Sheahan K, Vieth M, Lugli A, Zlobec I, Pecori S, Wang LM, Langner C, Mitomi H, Nakamura T, Watanabe M, Ueno H, Chasle J, Conley SA, Herlin P, Lauwers GY, Risio M (2012) Diagnostic reproducibility of tumour budding in colorectal cancer: a multicentre, multinational study using virtual microscopy. Histopathology 61:562–575. https://doi.org/10.1111/j.1365-2559.2012.04270.x
Konishi T, Shimada Y, Lee LH, Cavalcanti MS, Hsu M, Smith JJ, Nash GM, Temple LK, Guillem JG, Paty PB, Garcia-Aguilar J, Vakiani E, Gonen M, Shia J, Weiser MR (2018) Poorly differentiated clusters predict colon cancer recurrence: an in-depth comparative analysis of invasive-front prognostic markers. Am J Surg Pathol 42:705–714. https://doi.org/10.1097/PAS.0000000000001059
Lai YH, Wu LC, Li PS, Wu WH, Yang SB, Xia P, He XX, Xiao LB (2014) Tumour budding is a reproducible index for risk stratification of patients with stage II colon cancer. Color Dis 16:259–264. https://doi.org/10.1111/codi.12454
Horcic M, Koelzer VH, Karamitopoulou E, Terracciano L, Puppa G, Zlobec I, Lugli A (2013) Tumor budding score based on 10 high-power fields is a promising basis for a standardized prognostic scoring system in stage II colorectal cancer. Hum Pathol 44:697–705. https://doi.org/10.1016/j.humpath.2012.07.026
Karamitopoulou E, Zlobec I, Kolzer V, Kondi-Pafiti A, Patsouris ES, Gennatas K, Lugli A (2013) Proposal for a 10-high-power-fields scoring method for the assessment of tumor budding in colorectal cancer. Mod Pathol 26:295–301. https://doi.org/10.1038/modpathol.2012.155
Martin B, Schafer E, Jakubowicz E, Mayr P, Ihringer R, Anthuber M, Schenkirsch G, Schaller T, Markl B (2018) Interobserver variability in the H&E-based assessment of tumor budding in pT3/4 colon cancer: does it affect the prognostic relevance? Virchows Arch 473:189–197. https://doi.org/10.1007/s00428-018-2341-1
Zlobec I, Berger MD, Lugli A (2020) Tumour budding and its clinical implications in gastrointestinal cancers. Br J Cancer. https://doi.org/10.1038/s41416-020-0954-z
Cappellesso R, Luchini C, Veronese N, Lo Mele M, Rosa-Rizzotto E, Guido E, De Lazzari F, Pilati P, Farinati F, Realdon S, Solmi M, Fassan M, Rugge M (2017) Tumor budding as a risk factor for nodal metastasis in pT1 colorectal cancers: a meta-analysis. Hum Pathol 65:62–70. https://doi.org/10.1016/j.humpath.2017.04.013
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kinugasa Y, Murofushi K, Nakajima TE, Oka S, Tanaka T, Taniguchi H, Tsuji A, Uehara K, Ueno H, Yamanaka T, Yamazaki K, Yoshida M, Yoshino T, Itabashi M, Sakamaki K, Sano K, Shimada Y, Tanaka S, Uetake H, Yamaguchi S, Yamaguchi N, Kobayashi H, Matsuda K, Kotake K, Sugihara K, Japanese Society for Cancer of the C, Rectum (2020) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25:1–42. https://doi.org/10.1007/s10147-019-01485-z
Bosch SL, Teerenstra S, de Wilt JH, Cunningham C, Nagtegaal ID (2013) Predicting lymph node metastasis in pT1 colorectal cancer: a systematic review of risk factors providing rationale for therapy decisions. Endoscopy 45:827–834. https://doi.org/10.1055/s-0033-1344238
Petrelli F, Pezzica E, Cabiddu M, Coinu A, Borgonovo K, Ghilardi M, Lonati V, Corti D, Barni S (2015) Tumour budding and survival in stage II colorectal cancer: a systematic review and pooled analysis. J Gastrointest Cancer 46:212–218. https://doi.org/10.1007/s12029-015-9716-1
Okuyama T, Nakamura T, Yamaguchi M (2003) Budding is useful to select high-risk patients in stage II well differentiated or moderately differentiated colon adenocarcinoma. Dis Colon Rectum 46:1400–1406
Hayes BD, Maguire A, Conlon N, Gibbons D, Wang LM, Sheahan K (2010) Reproducibility of the rapid bud count method for assessment of tumor budding in stage II colorectal cancer. Am J Surg Pathol 34:746–748
Betge J, Kornprat P, Pollheimer MJ, Lindtner RA, Schlemmer A, Rehak P, Vieth M, Langner C (2012) Tumor budding is an independent predictor of outcome in AJCC/UICC stage II colorectal cancer. Ann Surg Oncol 19:3706–3712. https://doi.org/10.1245/s10434-012-2426-z
Canney AL, Kevans D, Wang LM, Hyland JM, Mulcahy HE, O'Donoghue DP, O'Sullivan J, Geraghty R, Sheahan K (2012) Stage II colonic adenocarcinoma: a detailed study of pT4N0 with emphasis on peritoneal involvement and the role of tumour budding. Histopathology 61:488–496. https://doi.org/10.1111/j.1365-2559.2012.04250.x
Group QC (2007) Adjuvant chemotherapy versus observation in patients with colorectal cancer: a randomised study. Lancet 370:2020–2029. https://doi.org/10.1016/s0140-6736(07)61866-2
Schmoll HJ, Van Cutsem E, Stein A, Valentini V, Glimelius B, Haustermans K, Nordlinger B, van de Velde CJ, Balmana J, Regula J, Nagtegaal ID, Beets-Tan RG, Arnold D, Ciardiello F, Hoff P, Kerr D, Kohne CH, Labianca R, Price T, Scheithauer W, Sobrero A, Tabernero J, Aderka D, Barroso S, Bodoky G, Douillard JY, El Ghazaly H, Gallardo J, Garin A, Glynne-Jones R, Jordan K, Meshcheryakov A, Papamichail D, Pfeiffer P, Souglakos I, Turhal S, Cervantes A (2012) ESMO Consensus Guidelines for management of patients with colon and rectal cancer. A personalized approach to clinical decision making. Ann Oncol 23:2479–2516. https://doi.org/10.1093/annonc/mds236
Shivji S, Conner J, Barresi V, Kirsch R (2020) Poorly differentiated clusters in colorectal cancer: a current review and implications for future practice. Histopathology. https://doi.org/10.1111/his.14128
Hong M, Kim JW, Shin MK, Kim BC (2017) Poorly differentiated clusters in colorectal adenocarcinomas share biological similarities with micropapillary patterns as well as tumor buds. J Korean Med Sci 32:1595–1602. https://doi.org/10.3346/jkms.2017.32.10.1595
Barresi V, Branca G, Vitarelli E, Tuccari G (2014) Micropapillary pattern and poorly differentiated clusters represent the same biological phenomenon in colorectal cancer: a proposal for a change in terminology. Am J Clin Pathol 142:375–383. https://doi.org/10.1309/AJCPFEA7KA0SBBNA
Studer L, Blank A, Bokhorst JM, Nagtegaal ID, Zlobec I, Lugli A, Fischer A, Dawson H (2020) Taking tumour budding to the next frontier - a post-ITBCC 2016 review. Histopathology. https://doi.org/10.1111/his.14267
Lugli A, Vlajnic T, Giger O, Karamitopoulou E, Patsouris ES, Peros G, Terracciano LM, Zlobec I (2011) Intratumoral budding as a potential parameter of tumor progression in mismatch repair-proficient and mismatch repair-deficient colorectal cancer patients. Hum Pathol 42:1833–1840. https://doi.org/10.1016/j.humpath.2011.02.010
Funding
This project has received funding from the Dutch Cancer Society, project number 10602/2016-2.
Author information
Authors and Affiliations
Contributions
Tariq Sami Haddad: Acquisition and interpretation of data, drafting, revision, and approval of the article.
Alessandro Lugli: Conception and design of study, acquisition and interpretation of data, drafting, revision, and approval of the article.
Susan Aherne: Acquisition of data, revision, and approval of the article.
Valeria Barresi: Acquisition of data, revision, and approval of the article.
Benoît Terris: Acquisition of data, revision, and approval of the article.
John-Melle Bokhorst: Acquisition of data, revision, and approval of the article.
Scarlet Fiona Brockmoeller: Acquisition of data, revision, and approval of the article.
Miriam Cuatrecasas: Acquisition of data, revision, and approval of the article.
Femke Simmer: Acquisition of data, revision, and approval of the article.
Hala El-Zimaity: Acquisition of data, revision, and approval of the article.
Jean-François Fléjou: Acquisition of data, revision, and approval of the article.
David Gibbons: Acquisition of data, revision, and approval of the article.
Gieri Cathomas: Acquisition of data, revision, and approval of the article.
Richard Kirsch: Acquisition of data, revision, and approval of the article.
Tine Plato Kuhlmann: Acquisition of data, revision, and approval of the article.
Cord Langner: Acquisition of data, revision, and approval of the article.
Maurice B. Loughrey: Acquisition of data, revision, and approval of the article.
Robert Riddell: Acquisition of data, revision, and approval of the article.
Ari Ristimäki: Acquisition of data, revision, and approval of the article.
Sanjay Kakar: Acquisition of data, revision, and approval of the article.
Kieran Sheahan: Acquisition of data, revision, and approval of the article.
Darren Treanor: Acquisition of data, revision, and approval of the article.
Jeroen van der Laak: Acquisition of data, revision, and approval of the article.
Michael Vieth: Acquisition of data, revision, and approval of the article.
Inti Zlobec: Acquisition of data, revision, and approval of the article.
Iris D. Nagtegaal: Conception and design of study, acquisition and interpretation of data, drafting, revision, and approval of the article.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 22 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Haddad, T.S., Lugli, A., Aherne, S. et al. Improving tumor budding reporting in colorectal cancer: a Delphi consensus study. Virchows Arch 479, 459–469 (2021). https://doi.org/10.1007/s00428-021-03059-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-021-03059-9