Abstract
In view of the associations of “a disintegrin and metalloprotease” (ADAM) with respiratory diseases, we assessed the expression of various ADAMs in human lung tissue. Lung tissue was obtained from nine individuals who underwent surgery for lung cancer or underwent lung transplantation for emphysema. Also, 16HBE 14o- (human bronchial epithelial) and A549 (alveolar type II epithelium-like) cell lines were used. Immunohistochemistry was performed with antibodies recognizing different ADAM domains. The ADAMs were typically distributed over the bronchial epithelium. ADAM8 and ADAM10 were expressed diffusely in all layers of the epithelium. ADAM9, ADAM17, and ADAM19 were predominantly expressed in the apical part of the epithelium, and ADAM33 was predominantly and strongly expressed in basal epithelial cells. In smooth muscle, ADAM19 and ADAM17 were strongly expressed, as was ADAM33, though this expression was weaker. ADAM33 was strongly expressed in vascular endothelium. All ADAMs were generally expressed in inflammatory cells. The typical distribution of ADAMs in the lung, especially in the epithelium, is interesting and suggests a localized function. As most ADAMs are involved in release of (pro-) inflammatory mediators and growth factors, they may play an important role in the first line of defense and in initiation of repair events in the airways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the “a disintegrin and metalloprotease” (ADAM) molecules are known for quite some time, it has more recently become clear that these molecules play a central role in many normal and abnormal biological processes. ADAMs are thought to be implicated in the control of membrane fusion and in cell–cell and cell–matrix interactions by the binding capacity of the disintegrin domain to specific integrins [1]. ADAMs have also been demonstrated to play a role in the shedding of proprotein ectodomains like membrane-anchored cytokines and growth factors [1]. The ADAM molecules are members of a disintegrin and metalloprotease family, which are type I transmembrane zymogen glycoproteins that typically contain a N-terminal secretion signal domain, an epidermal growth factor (EGF)-like-transmembrane part, and a cytoplasmic (C-terminal) domain [2, 3]. The EGF-like transmembrane domain has a prodomain, a metalloprotease-, a disintegrin-, and a cysteine-rich domain. For several ADAMs, the specific substrates have not been identified yet. The most extensively studied ADAM molecule is ADAM17 (also known as tumor necrosis factor (TNF)-alpha-converting enzyme (TACE)), which cleaves membrane-bound TNF-alpha, thereby releasing this molecule in its active, soluble form [4].
Because of their biological role in humans, further knowledge about the localization and function of ADAM-family members is also of importance to understand their role in disease development. In recent studies, ADAMs have been suggested to play a role in a pulmonary disease like asthma [5–9] but also in interstitial lung disease [10], eosinophilic pneumonia [11], and lung cancer [12]. Moreover, single nucleotide polymorphisms (SNPs) in ADAM33 have been found to be associated with asthma development and progression [7] as well as with progressive lung function loss in the general population and development of COPD [13, 14]. In view of the association of ADAMs with respiratory diseases, our study was undertaken to assess the expression and localization of various ADAMs with metalloproteinase activity (ADAM8, ADAM9, ADAM10, ADAM17, ADAM19, and ADAM33) in human lung tissue. To verify epithelial localization, ADAM expression was also assessed in a human bronchial and alveolar epithelial cell line.
Materials and methods
Human lung tissue
Lung tissue was obtained from six individuals (age median [range], 65 [62–74]; four men, two women; three current smokers, two ex-smokers, one non-smoker) who underwent surgery for lung cancer and from three patients (age median [range], 61 [53–70]; two men, one woman, all ex-smokers) that underwent lung transplantation for emphysema. Lung tissue was taken as far as possible from the tumor and was normal on inspection. The lung tissue was only included in the study after exclusion of any lung pathology (for the emphysema cases, any lung pathology other than seen in COPD) as based on clinical data, lung function, and routine histological examination of lung tissue performed by an experienced pulmonary pathologist (WT). The procedures followed were in accordance with the ethical local and national guidelines.
Immunohistochemistry
Antibodies recognizing different domains of the ADAMs were commercially obtained (Table 1). Frozen lung sections were cut at 4 μm, dried for 20 min, and fixed in acetone (100%). Sections were incubated for 1 h with rabbit or goat antibodies for ADAMs in a proper dilution as determined previously. Endogenous peroxidase was blocked with 0.075% H2O2 in phosphate-buffered saline (PBS, pH 7.4) for 30 min. Subsequently, sections incubated with rabbit antibodies were incubated for 30 min with peroxidase conjugated goat-anti-rabbit (GARpo) anti-serum, followed by incubation with rabbit-anti-goat (RAGpo). Sections incubated with goat antibodies were incubated with RAGpo, followed by incubation with GARpo. Sections were rinsed in PBS for 5 min after each incubation step. Peroxidase activity was demonstrated by immersing the slides in sodium acetate buffer containing 0.2 mg/ml 3-amino-9-ethyl-carbazole (Sigma-Aldrich Chemie BV, Zwijndrecht, The Netherlands) and 0.03% H2O2 for 15 min. Sections were counterstained with Mayers hematoxylin for 1 min. Immunohistology staining results were evaluated by three independent observers. Staining intensity was for each of the indicated tissue elements (Table 1) graded as − (absent), ± (weak), + (moderate), or ++ (strong).
Cell lines
16HBE 14o- (human bronchial epithelial cell line, a gift of Prof. D.C. Gruenert, University of Vermont, San Francisco, CA, USA) and A549 (alveolar type II epithelium-like cell line, American Type Culture Collection, Rockville, MD, USA) cells were cultured in Earle's MEM (BioWhittaker Europe BV, Cambrex, Verviers, Belgium) and RPMI 1640 (BioWhittaker), respectively. Both culture media were supplemented with 10% heat inactivated fetal bovine serum (BioWhittaker), l-glutamine (2 mM, BioWhittaker), streptomycin (100 µg/ml, BioWhittaker), and penicillin (100 U/ml, BioWhittaker) and cultured at 37°C with 5% CO2. 16HBE and A549 cells were detached by trypsin-EDTA (BioWhittaker) treatment and cytospins were made. Subsequently, these cytospins were incubated with antibodies against the ADAMs and immunostained as described above.
Results
Expression of ADAMs in bronchial epithelial cells
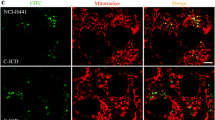
The expression of the various ADAMs studied in different locations of human lung tissue is shown in Table 1 and illustrated in Fig. 1. There was no difference in expression patterns in the emphysematous lung tissue when compared to the normal lung tissue from the other six patients. All ADAMs were expressed in bronchial epithelium, yet they have a different distribution between basal and apical cells. ADAM9, ADAM17, and ADAM19 are predominantly expressed in the apical part of the epithelium, whereas ADAM33 expression is higher in basal epithelial cells. ADAM10 and ADAM8 are diffusely expressed over the epithelium. Interestingly, staining for the C-terminal end of ADAM10 is mainly seen in the apical part, and for the N-terminal end, this is located in the basal cells of the epithelium.
Expression of ADAMs in normal human lung, immunostaining with antibodies designated to different domains of ADAMs (as indicated by manufacturers): a ADAM8 ectodomain, b ADAM10 N-terminal domain, c ADAM10 catalytic site, d ADAM17 cytoplasmic domain, e ADAM19 catalytic site, f ADAM19 N-terminal domain, g ADAM33 prodomain, h ADAM33 N-terminal domain, i ADAM33 cytoplasmic domain. Note specific localization patterns in different tissue compartments, in particular in different parts of the bronchial epithelium (immunoperoxidase, original magnification ×200)
To verify our tissue findings, we stained ADAMs on the bronchial cell line 16HBE (Table 2), illustrated in Fig. 2. In 16HBE cells, ADAM9 and ADAM10 are most strongly expressed, whereas ADAM33 is weakly expressed. Not all 16HBE cells show expression of all ADAM subdomains; the percentage and intensity of positive cells are given in Table 2. Staining for the catalytic site of ADAM19 and ADAM33 showed no positive cells at all. When comparing the results of epithelial cell lines and lung tissue, expression in the 16HBE cell line matches the findings in bronchial epithelial cells in lung tissue.
Expression of ADAMs in alveolar epithelial cells
All ADAMs are expressed in alveolar epithelium (type II cells); however, expression of ADAM10 and ADAM19 is weaker in alveolar than bronchial epithelial cells. ADAM8, ADAM17, ADAM9, and ADAM33 in contrast are equally expressed in both epithelial cell types.
In the A549 alveolar epithelial type 2 cell line, almost all ADAMs are expressed in all cells (Table 2; illustrated in Fig. 2) although the ADAM33 catalytic site and prodomain show a minor number (5–10%) of negative cells, and ADAM 19 catalytic site shows no staining at all. In general, expression in A549 cells matches the findings in the alveolar type 2 cells.
Expression of ADAMs in bronchial smooth muscle tissue
The expression of ADAM19 is higher in smooth muscle than in bronchial epithelial cells, whereas ADAM17 is equally expressed in smooth muscle and epithelium. ADAM9, ADAM10, and ADAM33 are also expressed in smooth muscle tissue, yet with a weaker staining in smooth muscle cells than in bronchial epithelial cells. ADAM8 is not expressed in smooth muscle tissue.
Expression of ADAMs in vascular endothelium
ADAM33 is the most strongly expressed ADAM in the vascular endothelium. Some weak expression of ADAM9, ADAM10, ADAM17, and ADAM19 is present, yet endothelial expression of these latter ADAMs is not found in all subjects.
Expression of ADAMs in inflammatory cells
All ADAMs are uniformly and very profoundly expressed in interstitial inflammatory cells.
Glandular cells and nerves
ADAMs are incidentally expressed in glandular cells and nerves that are present in some of the specimen.
Discussion
ADAMs have been suggested to play an important role in lung diseases [11–15]. As a starting point to understand the role of ADAMs in lung disease, it is important to note that we have found several ADAMs expressed specifically in both bronchial epithelium and alveolar type 2 epithelial cells, interstitial inflammatory cells, smooth muscle, and endothelium. Individual ADAMs showed specific distribution patterns in these cell types, whereas some ADAMs showed remarkable co-localization, suggestive for similar or mutual interacting functions. ADAM expression in a human lung bronchial and alveolar type epithelial cell line confirmed the expression in epithelium in human lung tissue. Interestingly, several ADAMs had a very topical (predominantly apical or basal) expression, in bronchial epithelium, suggesting that the more precise localization of individual ADAM molecules may signify their functional relevance.
Given the apical localization in airway epithelial cells, ADAM17, ADAM19, and ADAM9 may play a role in early immune defense mechanisms. This is exemplified by both ADAM17 and ADAM19, which are both capable of shedding TNF-alpha. ADAM17 plays a key role in this release of soluble TNF-alpha by cleavage of the membrane-anchored precursor of TNF-alpha [16–18]. TNF-alpha is a proinflammatory cytokine and a key mediator in immune defense with a role in induction and amplification of inflammation, as a response to external, potential threatening stimuli. The prominent apical distribution of ADAM17 in the bronchial epithelium may thus enable easy activation and hence a low threshold for rapid and early release of TNF-alpha in the airway lumen in the defense to disease-initiating inhaled substances. In addition, cigarette smoke exposure of human airway epithelial cells has been shown to lead to ADAM17-mediated release of amphiregulin, which is a ligand for the epidermal growth factor receptor (EGFR) [19]. This can be of clinical relevance since stimulation of EGFR on epithelial cells contributes to mucus production and epithelial cell proliferation.
ADAM19 can, besides TNF-alpha, release tumor necrosis factor-related activation-induced cytokine (TRANCE) [20]. TRANCE is part of the tumor necrosis factor superfamily and has an immunity-modulating role as well. The joint apical expression of ADAM17 and ADAM19 is of interest and raises the question of whether this represents ability of coordinated action of the two molecules or that the regulation of each molecule is individually organized and may thus indicate their different roles in pathogenesis of disease. ADAM17, but in particular ADAM19, was also strongly expressed in smooth muscle. It is conceivable that particularly with chronic airway wall inflammation, as in asthma, these ADAMs may become activated and contribute to the perpetuation of the inflammatory process.
ADAM9, which also is apically expressed in epithelial cells, has a quite different function. It is capable of shedding of heparin-binding epidermal growth factor (HB-EGF) from bronchial epithelial cells via protein kinase C-delta (PKC-delta) activation [21]. HB-EGF is an important growth factor, not only for epithelial cells but also for smooth muscle cells and fibroblasts. This particular apical localization could then represent low threshold ability to early tissue (epithelial) repair, in conjunction with the other local defense mechanisms at the epithelial interface. Furthermore, ADAM9-mediated cellular adhesion by integrin binding has been described in fibroblasts, which leads to induction of fibroblast motility [22]. This capacity suggests that ADAM9 also may play a role in remodeling of the airway wall by regulating motility and migration of fibroblasts and smooth muscle cells.
ADAM10 was diffusely expressed in the bronchial epithelium, and the N-terminal domain showed especially strong staining in basal epithelial cells. ADAM10 was also weakly expressed in smooth muscle. Similar to ADAM9, ADAM10 is capable of HB-EGF shedding. Considering the differences in distribution between these two ADAMs, it is tempting to speculate that once repair has set in by activating apically located ADAM9, ADAM10 in basal cells may be responsible for sustained repair effects, possibly also affecting underlying submucosal structures.
Human ADAM8 has been clustered as a human leukocyte differentiation antigen, CD156, and is thought to play a role in cell adhesion and infiltration of inflammatory cells [23, 24]. ADAM8 was expressed in bronchial and alveolar type II epithelium and interstitial inflammatory cells, predominantly with morphology of neutrophils and macrophages, without smooth muscle expression. These findings are consistent with its published expression in the epithelium and increased gene transcription in peribronchial and perivascular inflammatory cells in an allergen induced murine model of asthma [5]. ADAM8 can cleave CD23, the low-affinity IgE receptor (FcεRIIb) [25], which is involved in up regulation of IL-4 induced synthesis of IgE in B-cells [26]. CD23 shedding would counteract IgE-mediated immune responses, next to inducing release of proinflammatory mediators from macrophages [27].
ADAM33 was the only ADAM that was predominantly (and strongly) expressed in the basal cells of bronchial epithelium (Fig. 1g, h, i). Furthermore, ADAM33 was expressed in bronchial smooth muscle. A recent study showed several SNPs in the ADAM33 gene to be associated with susceptibility of asthma and bronchial hyperresponsiveness [6]. The latter study showed ADAM33 to be expressed in human pulmonary fibroblasts and bronchial smooth muscle tissue, yet not in epithelial cells. Our findings are in line with more recent publications that showed ADAM33 to be localized in epithelium [8, 28]. Low mRNA levels of ADAM33 are shown in bronchial biopsies although no mRNA was found in epithelial cells from bronchial brushes [29]. Considering our present findings, the latter might be explained by the content of the brushes, in which generally abundant ciliated cells and little basal epithelial cells are present. Yang et al. recently described a lack of ADAM33 mRNA in bronchial epithelium samples [30]. They suggested ADAM33 repression by a cell type-selective expression of ADAM33, which was epigenetically controlled by DNA methylation.
Our findings of basal epithelial cell expression of ADAM33 support its possible involvement in remodeling process, as in asthma [31]. This may well be initiated by shedding of c-kit ligand. Not only ADAM33 [32] but also ADAM8 [33], ADAM9 [34], ADAM17 [35, 36], and ADAM19 [20] are capable of shedding of c-kit ligand, also known as stem cell factor (SCF). SCF plays, apart from its main role as hemopoietic growth factor, a role in recruitment and in maturation of mast cell progenitors [37], sustaining the survival and maintaining phenotypic properties of mast cells in mucosal tissues [38, 39]. Furthermore, SCF may play a role in eosinophil migration and/or retention in activated tissue compartments [31], given its expression on human peripheral blood cells. Eosinophils express a functional c-kit receptor that stimulates very late antigen 4 (VLA-4)-mediated cell adhesion to fibronectin and vascular cell adhesion molecule 1 (VCAM-1). As mast cells and eosinophils are thought to play a key role in the pathogenesis of asthma [40, 41] and possibly also to be implicated in COPD [42, 43], the extensive presence of ADAMs capable of release of c-kit ligand in the airways suggests a regulatory role for these molecules in manifestation of these diseases.
Another issue of importance is that a large number of alternatively spliced forms of ADAM33 have been identified [44, 45]. Some show structural similarity to a synthetic ADAM12-S that induces myogenesis [46], in turn suggesting ADAM33 to be able to induce airway smooth muscle proliferation and hypertrophy [44].
Interestingly, strong expression of ADAM33 was observed in vascular endothelial cells, whereas other ADAMs were more weakly expressed. This may reflect their role in adhesion, extravasation, and possibly activation of inflammatory cells, especially eosinophils. Furthermore, it might contribute to angiogenesis, which is thought to play a role in asthma and COPD as well [47, 48]. Furthermore, angiogenesis is important in tumor development; EGFR-signaling of ADAMs may contribute in this way [3].
We used commercially available antibodies that are designed to bind to different domains of the ADAM proteins. We found similar localization in expression of different antibodies to subdomains of the same ADAM and for some, like ADAM33, also for different antibodies to the same (cytoplasmic) subdomain. Interestingly, there is a lack of staining for the catalytic (metalloproteinase) site of ADAM19 and ADAM33, which may implicate that these ADAMs are lacking the metalloproteinase site and therefore are present in an inactive form. For ADAM33, there is suggestive evidence that this is indeed the case since alternative splice variants have been described that mostly lack the metalloproteinase site [44].
Our present study is the first to investigate expression of several ADAM proteins in lung tissue and discusses the findings as to their putative role in the pathogenesis of respiratory diseases. As emphysematous lung tissue shows a similar expression pattern as the other lung tissues from patients that underwent surgery for lung cancer, there seems to be no obvious effect of the lung tumors on the lung tissue with respect to ADAMs expression. Clearly, this survey should be expanded, including much more diseased lung tissue to get further information about possible ADAMs variations that may play a role in lung disease. ADAMs appear to have a typical, specific distribution over the bronchial epithelium and other parts of the bronchial wall like smooth muscle and vascular endothelium. This specific localization of ADAMs, especially in the apical and basal epithelial cells, is interesting as to their individual and joint contribution toward defense against inhaled substances. Given the current knowledge on their functional properties, the distribution suggests that ADAMs play a main regulatory role in the first line of defense at the epithelial barrier by coordinated release of proinflammatory mediators as well as in remodeling and tissue repair by topic release of various growth factors. A next step is to dissect the exact functional role of ADAMs and subtle functional expression differences of ADAMs and their splice variants in the development and progression of pulmonary diseases.
References
Primakoff P, Myles DG (2000) The ADAM gene family: surface proteins with adhesion and protease activity. Trends Genet 16:83–87
Black RA, White JM (1998) ADAMs: focus on the protease domain. Curr Opin Cell Biol 10:654–659
Blobel CP (2005) ADAMs: key components in EGFR signalling and development. Nat Rev Mol Cell Biol 6:32–43
Peschon JJ, Slack JL, Reddy P et al (1998) An essential role for ectodomain shedding in mammalian development. Science 282:1281–1284
King NE, Zimmermann N, Pope SM et al (2004) Expression and regulation of a disintegrin and metalloproteinase (ADAM) 8 in experimental asthma. Am J Respir Cell Mol Biol 31:257–265
Van Eerdewegh P, Little RD, Dupuis J et al (2002) Association of the ADAM33 gene with asthma and bronchial hyperresponsiveness. Nature 418:426–430
Jongepier H, Boezen HM, Dijkstra A et al (2004) Polymorphisms of the ADAM33 gene are associated with accelerated lung function decline in asthma. Clin Exp Allergy 34:757–760
Lee JY, Park SW, Chang HK et al (2006) A disintegrin and metalloproteinase 33 protein in patients with asthma: relevance to airflow limitation. Am J Respir Crit Care Med 173:729–735
Holgate ST, Holloway J, Wilson S et al (2006) Understanding the pathophysiology of severe asthma to generate new therapeutic opportunities. J Allergy Clin. Immunol 117:496–506
Edwards ST, Cruz AC, Donnelly S et al (2005) c-Kit immunophenotyping and metalloproteinase expression profiles of mast cells in interstitial lung diseases. J Pathol 206:279–290
Matsuno O, Miyazaki E, Nureki S et al (2007) Elevated soluble ADAM8 in bronchoalveolar lavage fluid in patients with eosinophilic pneumonia. Int Arch Allergy Immunol 142:285–290
Rocks N, Paulissen G, Quesada-Calvo F et al (2006) Expression of a disintegrin and metalloprotease (ADAM and ADAMTS) enzymes in human non-small-cell lung carcinomas (NSCLC). Br J Cancer 94:724–730
van Diemen CC, Postma DS, Vonk JM et al (2005) A disintegrin and metalloprotease 33 polymorphisms and lung function decline in the general population. Am J Respir Crit Care Med 172:329–333
Gosman MM, Boezen HM, van Diemen CC et al (2007) A disintegrin and metalloprotease 33 and chronic obstructive pulmonary disease pathophysiology. Thorax 62:242–247
Holgate ST, Yang Y, Haitchi HM et al (2006) The genetics of asthma: ADAM33 as an example of a susceptibility gene. Proc Am Thorac Soc 3:440–443
Black RA, Rauch CT, Kozlosky CJ et al (1997) A metalloproteinase disintegrin that releases tumour-necrosis factor-alpha from cells. Nature 385:729–733
Moss ML, Jin SL, Milla ME et al (1997) Cloning of a disintegrin metalloproteinase that processes precursor tumour-necrosis factor-alpha. Nature 385:733–736
Zheng Y, Saftig P, Hartmann D et al (2004) Evaluation of the contribution of different ADAMs to tumor necrosis factor alpha (TNFalpha) shedding and of the function of the TNFalpha ectodomain in ensuring selective stimulated shedding by the TNFalpha convertase (TACE/ADAM17). J Biol Chem 279:42898–42906
Lemjabbar H, Li D, Gallup M et al (2003) Tobacco smoke-induced lung cell proliferation mediated by tumor necrosis factor alpha-converting enzyme and amphiregulin. J Biol Chem 278:26202–26207
Chesneau V, Becherer JD, Zheng Y et al (2003) Catalytic properties of ADAM19. J Biol Chem 278:22331–22340
Izumi Y, Hirata M, Hasuwa H et al (1998) A metalloprotease-disintegrin, MDC9/meltrin-gamma/ADAM9 and PKCdelta are involved in TPA-induced ectodomain shedding of membrane-anchored heparin-binding EGF-like growth factor. EMBO J 17:7260–7272
Nath D, Slocombe PM, Webster A et al (2000) Meltrin gamma(ADAM-9) mediates cellular adhesion through alpha(6) beta(1) integrin, leading to a marked induction of fibroblast cell motility. J Cell Sci 113(Pt 12):2319–2328
Yoshiyama K, Higuchi Y, Kataoka M et al (1997) CD156 (human ADAM8): expression, primary amino acid sequence, and gene location. Genomics 41:56–62
Higuchi Y, Yasui A, Matsuura K et al (2002) CD156 transgenic mice. Different responses between inflammatory types. Pathobiology 70:47–54
Fourie AM, Coles F, Moreno V et al (2003) Catalytic activity of ADAM8, ADAM15, and MDC-L (ADAM28) on synthetic peptide substrates and in ectodomain cleavage of CD23. J Biol Chem 278:30469–30477
Nakamura T, Kloetzer WS, Brams P et al (2000) In vitro IgE inhibition in B cells by anti-CD23 monoclonal antibodies is functionally dependent on the immunoglobulin Fc domain. Int J Immunopharmacol 22:131–141
Bonnefoy JY, Plater-Zyberk C, Lecoanet-Henchoz S et al (1996) A new role for CD23 in inflammation. Immunol Today 17:418–420
Foley SC, Mogas AK, Olivenstein R et al (2007) Increased expression of ADAM33 and ADAM8 with disease progression in asthma. J Allergy Clin Immunol 119:863–871
Haitchi HM, Powell RM, Shaw TJ et al (2005) ADAM33 expression in asthmatic airways and human embryonic lungs. Am J Respir Crit Care Med 171:958–965
Yang Y, Haitchi HM, Cakebread J et al (2008) Epigenetic mechanisms silence a disintegrin and metalloprotease 33 expression in bronchial epithelial cells. J Allergy Clin Immunol 121(1393–9):1399
Yuan Q, Austen KF, Friend DS et al (1997) Human peripheral blood eosinophils express a functional c-kit receptor for stem cell factor that stimulates very late antigen 4 (VLA-4)-mediated cell adhesion to fibronectin and vascular cell adhesion molecule 1 (VCAM-1). J Exp Med 186:313–323
Zou J, Zhu F, Liu J et al (2004) Catalytic activity of human ADAM33. J Biol Chem 279:9818–9830
Amour A, Knight CG, English WR et al (2002) The enzymatic activity of ADAM8 and ADAM9 is not regulated by TIMPs. FEBS Lett 524:154–158
Roghani M, Becherer JD, Moss ML et al (1999) Metalloprotease-disintegrin MDC9: intracellular maturation and catalytic activity. J Biol Chem 274:3531–3540
Mohan MJ, Seaton T, Mitchell J et al (2002) The tumor necrosis factor-alpha converting enzyme (TACE): a unique metalloproteinase with highly defined substrate selectivity. Biochemistry 41:9462–9469
Cruz AC, Frank BT, Edwards ST et al (2004) Tumor necrosis factor-alpha-converting enzyme controls surface expression of c-Kit and survival of embryonic stem cell-derived mast cells. J Biol Chem 279:5612–5620
Da Silva CA, Reber L, Frossard N (2006) Stem cell factor expression, mast cells and inflammation in asthma. Fundam Clin Pharmacol 20:21–39
Iemura A, Tsai M, Ando A et al (1994) The c-kit ligand, stem cell factor, promotes mast cell survival by suppressing apoptosis. Am J Pathol 144:321–328
MacDonald AJ, Thornton EM, Newlands GF et al (1996) Rat bone marrow-derived mast cells co-cultured with 3T3 fibroblasts in the absence of T-cell derived cytokines require stem cell factor for their survival and maintain their mucosal mast cell-like phenotype. Immunology 88:375–383
Boyce JA (2003) The role of mast cells in asthma. Prostaglandins Leukot Essent Fatty Acids 69:195–205
Oliveira SH, Lukacs NW (2003) Stem cell factor: a hemopoietic cytokine with important targets in asthma. Curr Drug Targets Inflamm Allergy 2:313–318
Grashoff WF, Sont JK, Sterk PJ et al (1997) Chronic obstructive pulmonary disease: role of bronchiolar mast cells and macrophages. Am J Pathol 151:1785–1790
Zhu J, Qiu YS, Majumdar S et al (2001) Exacerbations of Bronchitis: bronchial eosinophilia and gene expression for interleukin-4, interleukin-5, and eosinophil chemoattractants. Am J Respir Crit Care Med 164:109–116
Powell RM, Wicks J, Holloway JW et al (2004) The splicing and fate of ADAM33 transcripts in primary human airways fibroblasts. Am J Respir Cell Mol Biol 31:13–21
Umland SP, Garlisi CG, Shah H et al (2003) Human ADAM33 messenger RNA expression profile and post-transcriptional regulation. Am J Respir Cell Mol Biol 29:571–582
Gilpin BJ, Loechel F, Mattei MG et al (1998) A novel, secreted form of human ADAM 12 (meltrin alpha) provokes myogenesis in vivo. J Biol Chem 273:157–166
Hashimoto M, Tanaka H, Abe S (2005) Quantitative analysis of bronchial wall vascularity in the medium and small airways of patients with asthma and COPD. Chest 127:965–972
Santos S, Peinado VI, Ramirez J et al (2002) Characterization of pulmonary vascular remodelling in smokers and patients with mild COPD. Eur Respir J 19:632–638
Acknowledgment
This work was supported by the Netherlands Asthma Foundation, grant number 3.2.00.38.
Conflict of interest
We declare that we have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Dijkstra, A., Postma, D.S., Noordhoek, J.A. et al. Expression of ADAMs (“a disintegrin and metalloprotease”) in the human lung. Virchows Arch 454, 441–449 (2009). https://doi.org/10.1007/s00428-009-0748-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-009-0748-4