Abstract
The Gleason grading system remains one of the most powerful prognostic factors in prostate cancer and is the dominant method around the world in daily practice. It is based solely on the glandular architecture performed at low magnification. The Gleason grading system should be performed in needle core biopsies and radical prostatectomy specimens where it shows a reasonable degree of correlation between both specimens, and most importantly, it remains vital in the treatment decision-making process. This review summarizes the current status of Gleason grading in prostate cancer, incorporating recent proposals for the best contemporary practice of prostate cancer grading.
Similar content being viewed by others
References
Allsbrook WC Jr, Mangold KA, Johnson MH, Lane RB, Lane CG, Amin MB, Bostwick DG, Humphrey PA, Jones EC, Reuter VE, Sakr W, Sesterhenn IA, Troncoso P, Wheeler TM, Epstein JI (2001) Interobserver reproducibility of Gleason grading of prostatic carcinoma: urologic pathologists. Hum Pathol 32:74–80
Allsbrook WC Jr, Mangold KA, Johnson MH, Lane RB, Lane CG, Epstein JI (2001) Interobserver reproducibility of Gleason grading of prostatic carcinoma: general pathologist. Hum Pathol 32:81–88
Amin M, Boccon-Gibod L, Egevad L, Epstein JI, Humphrey PA, Mikuz G, Newling D, Nilsson S, Sakr W, Srigley JR, Wheeler TM, Montironi R (2005) Prognostic and predictive factors and reporting of prostate carcinoma in prostate needle biopsy specimens. Scand J Urol Nephrol Suppl 216:20–33
Amin MB, Grignon DJ, Humphrey PA, Srigley JR (2004) Gleason grading of prostate cancer: a contemporary approach. Lippincott Williams & Wilkins, Philadelphia, PA
Amin MB, Schultz DS, Zarbo RJ (1994) Analysis of cribriform morphology in prostatic neoplasia using antibody to high-molecular-weight cytokeratins. Arch Pathol Lab Med 118:260–264
Augustin H, Eggert T, Wenske S, Karakiewicz PI, Palisaar J, Daghofer F, Huland H, Graefen M (2004) Comparison of accuracy between the Partin tables of 1997 and 2001 to predict final pathological stage in clinically localized prostate cancer. J Urol 171:177–181
Babaian RJ, Troncoso P, Bhadkamkar VA, Johnston DA (2001) Analysis of clinicopathologic factors predicting outcome after radical prostatectomy. Cancer 91:1414–1422
Bailar JC 3rd, Mellinger GT, Gleason DF (1966) Survival rates of patients with prostatic cancer, tumor stage, and differentiation–preliminary report. Cancer Chemother Rep 50:129–136
Boccon-Gibod L, van der Kwast TH, Montironi R, Bono A (2004) Handling and pathology reporting of prostate biopsies. Eur Urol 46:177–181
Bostwick DG (1994) Gleason grading of prostatic needle biopsies. Correlation with grade in 316 matched prostatectomies. Am J Surg Pathol 18:796–803
Bostwick DG, Grignon DJ, Hammond ME, Amin MB, Cohen M, Crawford D, Gospadarowicz M, Kaplan RS, Miller DS, Montironi R, Pajak TF, Pollack A, Srigley JR, Yarbro JW (2000) Prognostic factors in prostate cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 124:995–1000
Chan TY, Partin AW, Walsh PC, Epstein JI (2000) Prognostic significance of Gleason score 3+4 versus Gleason score 4+3 tumor at radical prostatectomy. Urology 56:823–827
Cheng L, Koch MO, Juliar BE, Daggy JK, Foster RS, Bihrle R, Gardner TA (2005) The combined percentage of Gleason patterns 4 and 5 is the best predictor of cancer progression after radical prostatectomy. J Clin Oncol 23:2911–2917
Eble JN, Sauter G, Epstein JI, Sesterhenn IA (2004) Pathology and genetics. Tumors of the urinary system and male genital organs. IARC, Lyon
Egan AJ, Lopez-Beltran A, Bostwick DG (1997) Prostatic adenocarcinoma with atrophic features: malignancy mimicking a benign process. Am J Surg Pathol 21:931–935
Egevad L, Allsbrook WC Jr., Epstein JI (2005) Current practice of Gleason grading among genitourinary pathologists. Hum Pathol 36:5–9
Epstein JI (2000) Gleason score 2–4 adenocarcinoma of the prostate on needle biopsy: a diagnosis that should not be made. Am J Surg Pathol 24:477–478
Epstein JI, Allsbrook WCJ, Amin MB, Egevad LL, and The ISUP Grading Committee (2005) The 2005 International Society of Urological Pathoogy (ISUP) consensus conference on Gleason grading of prostatic carcinoma. Am J Surg Pathol 29:1228–1242
Epstein JI, Amin M, Boccon-Gibod L, Egevad L, Humphrey PA, Mikuz G, Newling D, Nilsson S, Sakr W, Srigley JR, Wheeler TM, Montironi R (2005) Prognostic factors and reporting of prostate carcinoma in radical prostatectomy and pelvic lymphadenectomy specimens. Scand J Urol Nephrol Suppl:34–63
Epstein JI, Partin AW, Sauvageot J, Walsh PC (1996) Prediction of progression following radical prostatectomy. A multivariate analysis of 721 men with long-term follow-up. Am J Surg Pathol 20:286–292
Gleason DF (1966) Classification of prostatic carcinomas. Cancer Chemother Rep 50:125–128
Gleason DF (1977) Histologic grading and clinical staging of prostatic carcinoma. In: Tannenbaum M (eds) Urologic pathology: the prostate. Lea & Feibiger, Philadelphia, PA
Gleason DF, Mellinger GT (1974) Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging. J Urol 111:58–64
Grober ED, Tsihlias J, Jewett MA, Sweet JM, Evans AJ, Trachtenberg J, Robinette M, Nam RK (2004) Correlation of the primary Gleason pattern on prostate needle biopsy with clinico-pathological factors in Gleason 7 tumors. Can J Urol 11:2157–2162
Humphrey PA (2003) Prostate pathology. ASCP Press, Chicago, IL
Kattan MW, Eastham JA, Wheeler TM, Maru N, Scardino PT, Erbersdobler A, Graefen M, Huland H, Koh H, Shariat SF, Slawin KM, Ohori M (2003) Counseling men with prostate cancer: a nomogram for predicting the presence of small, moderately differentiated, confined tumors. J Urol 170:1792–1797
Kunz GM Jr, Epstein JI (2003) Should each core with prostate cancer be assigned a separate Gleason score? Hum Pathol 34:911–914
Lopez-Beltran A, Eble JN, Bostwick DG (2005) Pleomorphic giant cell carcinoma of the prostate. Arch Pathol Lab Med 129:683–685
Lopez-Beltran A, Qian J, Montironi R, Luque RJ, Bostwick DG (2005b) Atypical adenomatous hyperplasia (adenosis) of the prostate: DNA ploidy analysis and immunophenotype. Int J Surg Pathol 13:167–173
Makarov DV, Sanderson H, Partin AW, Epstein JI (2002) Gleason score 7 prostate cancer on needle biopsy: is the prognostic difference in Gleason scores 4+3 and 3+4 independent of the number of involved cores? J Urol 167:2440–2442
Mazzucchelli R, Lopez-Beltran A, Scarpelli M, Montironi R (2002) Predictive factors in prostate needle biopsy. Pathologica 94:331–337
Mazzucchelli R, Santinelli A, Lopez-Beltran A, Scarpelli M, Montironi R (2002) Evaluation of prognostic factors in radical prostatectomy specimens with cancer. Urol Int 68:209–215
Mian BM, Troncoso P, Okihara K, Bhadkamkar V, Johnston D, Reyes AO, Babaian RJ (2002) Outcome of patients with Gleason score 8 or higher prostate cancer following radical prostatectomy alone. J Urol 167:1675–1680
Mills SE, Fowler JE Jr (1986) Gleason histologic grading of prostatic carcinoma. Correlations between biopsy and prostatectomy specimens. Cancer 57:346–349
Montironi R, Mazzuccheli R, Scarpelli M, Lopez-Beltran A, Fellegara G, Algaba F (2005) Gleason grading of prostate cancer in needle biopsies or radical prostatectomy specimens: contemporary approach, current clinical significance and sources of pathology discrepancies. BJU Int 95:1146–1152
Montironi R, Mazzucchelli R, Stramazzotti D, Scarpelli M, Lopez Beltran A, Bostwick DG (2005) Basal cell hyperplasia and basal cell carcinoma of the prostate: a comprehensive review and discussion of a case with c-erbB-2 expression. J Clin Pathol 58:290–296
Montironi R, Mazzucchelli R, van der Kwast T (2003) Morphological assessment of radical prostatectomy specimens. A protocol with clinical relevance. Virchows Arch 442:211–217
Montironi R, van der Kwast T, Boccon-Gibod L, Bono AV (2003b) Handling and pathology reporting of radical prostatectomy specimens. Eur Urol 44:626–636
Montironi R, Scarpelli M, Lopez Beltran A (2004) Carcinoma of the prostate: inherited susceptibility, somatic gene defects and androgen receptors. Virchows Arch 444:503–508
Mosse CA, Magi-Galluzzi C, Tsuzuki T, Epstein JI (2004) The prognostic significance of tertiary Gleason pattern 5 in radical prostatectomy specimens. Am J Surg Pathol 28:394–398
Pacelli A, Lopez-Beltran A, Egan AJ, Bostwick DG (1998) Prostatic adenocarcinoma with glomeruloid features. Hum Pathol 29:543–546
Pan CC, Chiang H, Chang YH, Epstein JI (2000) Tubulocystic clear cell adenocarcinoma arising within the prostate. Am J Surg Pathol 24:1433–1436
Pan CC, Potter SR, Partin AW, Epstein JI (2000) The prognostic significance of tertiary Gleason patterns of higher grade in radical prostatectomy specimens: a proposal to modify the Gleason grading system. Am J Surg Pathol 24:563–569
Partin AW, Kattan MW, Subong EN, Walsh PC, Wojno KJ, Oesterling JE, Scardino PT, Pearson JD (1997) Combination of prostate-specific antigen, clinical stage, and Gleason score to predict pathological stage of localized prostate cancer. A multi-institutional update. JAMA 277:1445–1451
Rubin MA, Bismar TA, Curtis S, Montie JE (2004) Prostate needle biopsy reporting: how are the surgical members of the Society of Urologic Oncology using pathology reports to guide treatment of prostate cancer patients? Am J Surg Pathol 28:946–952
Rubin MA, Dunn R, Kambham N, Misick CP, O’Toole KM (2000) Should a Gleason score be assigned to a minute focus of carcinoma on prostate biopsy? Am J Surg Pathol 24:1634–1640
Sakr WA, Tefilli MV, Grignon DJ, Banerjee M, Dey J, Gheiler EL, Tiguert R, Powell IJ, Wood DP (2000) Gleason score 7 prostate cancer: a heterogeneous entity? Correlation with pathologic parameters and disease-free survival. Urology 56:730–734
Srigley JR, Amin M, Boccon-Gibod L, Egevad L, Epstein JI, Humphrey PA, Mikuz G, Newling D, Nilsson S, Sakr W, Wheeler TM, Montironi R (2005) Prognostic and predictive factors in prostate cancer: historical perspectives and recent international consensus initiatives. Scand J Urol Nephrol Suppl 216:8–19
Steinberg DM, Sauvageot J, Piantadosi S, Epstein JI (1997) Correlation of prostate needle biopsy and radical prostatectomy Gleason grade in academic and community settings. Am J Surg Pathol 21:566–576
Tran TT, Sengupta E, Yang XJ (2001) Prostatic foamy gland carcinoma with aggressive behavior: clinicopathologic, immunohistochemical, and ultrastructural analysis. Am J Surg Pathol 25:618–623
Acknowledgement
This work was supported by the Grant FIS 03/0952 (Madrid, Spain).
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Gleason pattern 1
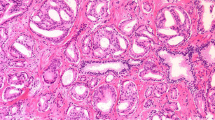
Nodule of separate, closely packed glands which do not infiltrate into adjacent benign prostatic tissue is very well circumscribed. The glands are of intermediate size and approximately equal in size and shape. The nucleus is typically small, and cytoplasm frequently is abundant and pale-staining. Nuclear and cytoplasm appearances are not taken into account in diagnosis. This pattern is exceedingly rare and usually seen in transition zone cancers (Fig. 1).
Gleason pattern 2
This pattern is characterized with round to oval glands with smooth ends. The glands are more loosely arranged and not quite as uniform in size and shape as those of Gleason pattern 1. There may be minimal invasion by neoplastic glands into the surrounding non-neoplastic prostatic tissue. The glands are of intermediate size and larger than those in Gleason pattern 1. The variation in glandular size and separation between glands is less than that seen in pattern 3. Although not evaluated in Gleason grading, the cytoplasm of Gleason pattern 2 cancers is abundant and pale-staining (Fig. 1). Gleason pattern 2 is usually seen in transition zone cancers but may occasionally be found in the peripheral zone.
Gleason pattern 3
This pattern is the most common pattern but is morphologically heterogeneous. The glands are infiltrative, and the distance between them is more variable than that in patterns 1 and 2. Malignant glands often infiltrate between adjacent non-neoplastic glands. The glands of pattern 3 vary in size and shape and are often angular (Fig. 1). Small glands are typical for pattern 3, but there may also be large and irregular glands. Each gland has an open lumen and is circumscribed by stroma. Cribriform pattern 3 is rare and difficult to distinguish morphologically from cribriform high-grade prostatic intraepithelial neoplasia (PIN). The latter shows the presence of basal cells. These are lacking in cribriform pattern 3 prostate cancer. This heterogeneous expression of Gleason grade 3 raised an initial subdivision in patterns A, B, and C, respectively.
Gleason pattern 4
Glands appear fused, cribriform, or they may be poorly defined and small. Fused glands are composed of a group of glands that are no longer completely separated by stroma (Fig. 1). The edge of a group of fused glands is scalloped, and there are occasional thin strands of connective tissue within this group. The hypernephroid pattern described by Gleason is a rare variant of fused glands with clear or very pale-staining cytoplasm. Cribriform pattern 4 glands are large or they may be irregular with jagged edges. As opposed to fused glands, there are no strands of stroma within a cribriform gland. Most cribriform invasive cancers should be assigned a pattern 4 rather than pattern 3. Poorly defined glands do not have a lumen that is completely encircled by epithelium.
Gleason pattern 5
This pattern is characterized with an almost complete loss of glandular lumina which are only occasionally present. The epithelium forms solid sheets, solid strands, or single cells invading the stroma; comedonecrosis may be present (Fig. 1). Care must be applied when assigning a Gleason pattern 4 or 5 to limited cancer on needle biopsy to exclude an artifact of tangential sectioning of lower-grade cancer.
Rights and permissions
About this article
Cite this article
Lopez-Beltran, A., Mikuz, G., Luque, R.J. et al. Current practice of Gleason grading of prostate carcinoma. Virchows Arch 448, 111–118 (2006). https://doi.org/10.1007/s00428-005-0102-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-005-0102-4