Abstract
The intensification of the stress response during resistance training (RT) under hypoxia conditions could trigger unwanted effects that compromise muscle health and, therefore, the ability of the muscle to adapt to longer training periods. We examined the effect of acute moderate terrestrial hypoxia on metabolic, inflammation, antioxidant capacity and muscle atrophy biomarkers after a single RT session in a young male population. Twenty healthy volunteers allocated to the normoxia (N < 700 m asl) or moderate altitude (HH = 2320 m asl) group participated in this study. Before and throughout the 30 min following the RT session (3 × 10 reps, 90 s rest, 70% 1RM), venous blood samples were taken and analysed for circulating calcium, inorganic phosphate, cytokines (IL-6, IL-10 and TNF-α), total antioxidant capacity (TAC) and myostatin. Main results displayed a marked metabolic stress response after the RT in both conditions. A large to very large proportional increase in the adjusted to pre-exercise change of inflammatory and anti-inflammatory markers favoured HH (serum TNF-α [ES = 1.10; p = 0.024] and IL-10 [ES = 1.31; p = 0.009]). The exercise produced a similar moderate increment of myostatin in both groups, followed by a moderate non-significant reduction in HH throughout the recovery (ES = − 0.72; p = 0.21). The RT slightly increased the antioxidant response regardless of the environmental condition. These results revealed no clear impact of RT under acute hypoxia on the metabolic, TAC and muscle atrophy biomarkers. However, a coordinated pro/anti-inflammatory response balances the potentiated effect of RT on systemic inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent decades, the scientific community has focused on understanding the benefits of hypoxia exposure on sports performance. At moderate terrestrial hypobaric hypoxia (HH), athletes can benefit from the stimulus of hypoxia, avoiding the adverse effects that could accompany the ascent and staying at higher altitudes [3]. The most sought-after adaptations are haematological, primarily related to long-distance disciplines due to their potential linkage to haemodynamic adaptation, involving vasodilation and blood flow improvement [27] (Fig. 1). Conversely, research on resistance training (RT) under hypoxic conditions on muscle mass development is inconclusive and quite scarce when it comes to the overall well-being and functionality of skeletal muscle (muscle health) analysis [8].
A cascade of inflammatory events initiates during and after acute resistance exercise in hypoxia [18, 38]. The inflammation constitutes a significant source of reactive oxygen and nitrogen species (RONS) and plays an essential role in skeletal muscle repair after exercise-induced muscle injury [25]. Furthermore, RONS derived from RT may contribute to enhance muscle protein synthesis and reduce muscle damage via the modulation of antioxidant signalling pathways [15]. Tissue hypoxia and RONS are involved in the activation of hypoxia-inducible factor-1α (HIF-1α), which has a key function in immune cell mobilisation and activation of cell survival mechanisms in skeletal muscle [21, 24]. Furthermore, HIF-1α stabilisation leads to inflammation and directly modulates the secretion of pro-inflammatory cytokines, such as tumour necrosis factor-alpha (TNF-α) and the interleukin-6 (IL-6)/soluble IL-6 receptor (sIL-6R) complex, among others [23].
TNF-α is synthesised by multiple immune cells and rapidly released into the blood after acute RT [29, 37]. Several authors have suggested that TNF-α activation is an early mediator of muscle damage and apoptosis, protein degradation and promotion of the inhibition of satellite cell differentiation via upregulation of the inflammatory response and myostatin expression [35]. Myostatin is a member of the transforming growth factor-beta superfamily secreted in skeletal muscle, among other tissues, due to oxidative stress, inflammation and glucocorticoid stimuli, and acts as a negative regulator of skeletal muscle mass [40]. It has also been shown that overexpression of inflammation-related proteins increases intracellular RONS and may induce cellular and extracellular damage due to a feedback loop in the TNF-α/myostatin axis [35] being expected that hypoxia further stimulates inflammation compared with normoxia [20]. It has also been demonstrated that chronic inflammatory status is associated with several diseases, including sarcopenia, which leads to progressive loss of muscle mass, highlighting the crucial role of the pro/anti-inflammatory balance in muscle health status [13].
Muscle contractions from acute RT increase and mobilise inflammatory cytokines, such as IL-6 [30] and immune cells, followed by the release of anti-inflammatory markers (IL-10, IL-1ra and sTNF-R1) [12]. Although IL-6 is considered an inflammatory cytokine, there is an association between satellite cell proliferation and transitory augments of IL-6, while chronic elevation is negatively associated with muscle health [8]. Furthermore, it also participates in the transition to an anti-inflammatory phenotype [4, 28] by inducing the subsequent release of IL-10, a key factor in the upregulation and control of the anti-inflammatory response [39]. IL-10 leads to positive self-feedback via ROS-dependent responses [22], preventing an exacerbation of the inflammatory state. However, the mechanisms through which the antioxidant response modulates the inflammatory system during RT performed under hypoxic conditions remain unknown. A recent meta-analysis on the topic concluded that exercise in hypoxia does not stimulate to a greater extent IL-6 or TNF-α than normoxia but leads to an increment in IL-10 [20]. However, this meta-analysis mixed terrestrial and normobaric hypoxia (NH) studies of different severity and duration with different types of exercise (i.e. the majority of the 23 included studies used aerobic exercise, and only 3 of them referred to RT exercise). Interestingly, the physiological impact of exercise in terrestrial hypoxia is described as more severe than NH for the same effective FiO2 [31]. Moreover, data from RT under acute exposition to terrestrial hypoxia constitute scarce but very useful information on muscle stress response during the acclimatisation phase, critical training days during altitude training camps.
Therefore, this research aimed to compare the acute effect of a single RT session on exercise-induced metabolic stress (such as circulating calcium and inorganic phosphate), inflammation (IL-6 and TNF-α), total antioxidant capacity and muscle mass atrophy (myostatin) biomarkers in normoxia and moderate HH. We hypothesised that HH will favour higher accumulation of stress-derived metabolites after RT exercise, thus impacting total antioxidant capacity (TAC) and inflammatory response than the same exercise in N.
Materials and methods
Design
A cross-sectional design with two independent controlled groups and intra-/inter-group measurements was used to analyse the acute effect of a traditional hypertrophy training session [9] on metabolic stress, inflammation, antioxidant capacity and muscle atrophy biomarkers. Following the successful completion of baseline assessments, the participants were aleatory allocated to the N or HH group (HH 2320 m asl; N 690 m asl) (Table 1).
Participants
Twenty physically active Caucasian male volunteers participated in this study. All participants had performed RT for a minimum of three times per week for at least the previous year. The participants had no health or muscular disorders, reported that they had not consumed any agents associated with muscle size development during the previous month and were unacclimated to high altitude (no altitude exposure in the 2 months before the study). All participants lived in N and were exclusively exposed to altitude during the training session. This study was approved by the local Ethics Committee (PEIBA: 2212-N-21) and was conducted in accordance with the Declaration of Helsinki and Biomedical Research (14/2007). Informed written consent was obtained from all participants prior to beginning the study.
Procedure
One week before the RT session, the participants engaged in a preparatory session to determine the training load (70% of 1 repetition maximum [1RM]) for each exercise. After a specific warm-up, the participants performed 1 set at the perceived 75% of 1RM (10 RM) followed by 1–2 additional sets with increasing loads until performing 2–3 repetitions to failure. The rest period between sets was kept to 5 min. 1RM values were predicted using Brzycki’s equation [6]. The participants rested for 72 h between the training session and refrained from performing any additional resistance-type or high-intensity training throughout the duration of the study. Two days before the beginning of the study, the participants visited the laboratory for baseline anthropometric measurements (height [Seca 202, Seca Ltd., Hamburg, Germany] and body mass [Tanita TBF-300, Tokyo, Japan]) after they had fasted since midnight of the previous day. Testing sessions were conducted at the same time of day, at a temperature of ~ 22 °C and ~ 60% humidity for the N condition or ~ 22 °C and ~ 28% humidity for the HH condition. The participants travelled by car to the HH training centre (32 km) to perform the training session. Arrival at the HH training centre occurred ~ 30 min before the training began. Arterial oxygen saturation (SpO2; Onyx Vantage 9590; Nonin, Plymouth, MN, USA) was assessed per duplicate before the start of the warm-up of the RT session to test the HH condition. Sensors displayed high reliability mean SpO2 values of 93.9% ± 1.63% and 97.2% ± 1.25% (CV < 1.74%), respectively, for the HH and N condition (p < 0.001).
The RT session comprised 3 sets of 8–10 repetitions at 70% 1RM of six functional exercises involving the main muscle groups of the body (full-body routine: back squat, deadlift, seated cable row, wide grip lat pulldown, bench press and barbell military press). The participants rested 90 s between each set. A standardised warm-up of 15 min was completed at the beginning of the training session (10 min of low-intensity aerobic exercise and stretching exercises followed by a specific warm-up of 2 sets of 10 repetitions [the first with 20 kg and the second at 50% 1RM estimated from the preliminary test, 120 s rest] of the back squat, seated cable row and bench press).
Blood samples
Blood samples were taken throughout the 30 min following the RT session to analyse the kinetics of release/clearance of the studied variables in this time window. Serum circulating variables, such as metabolites, inorganic phosphate (Pi) and calcium (Ca2+), TAC and cytokines (IL-6, IL-10, TNF-α and myostatin), were determined. Immediately following the exercise, an antecubital vein of the arm was canalised via a catheter and remained permeable by using a physiological saline solution. Two millilitres of blood before each extraction were discarded to avoid dilution of the sample. Five millilitres of blood were extracted at 5, 10 and 30 min after the RT session. All blood samples were kept in cold conditions after extraction and centrifuged to isolate serum within 4 h at 3000 rpm for 10 min. Finally, several 500 µl aliquots of serum were stored at − 70 °C until use. The basal condition was established before the beginning of the study at N conditions from a blood collection after two days of refraining from any exercise.
Cytokines were assessed at 5 and 30 min following the RT session using the Milliplex Human High Sensitivity T Cell Panel (HSTCMAG-28SK) from Sigma-Aldrich (Darmstadt, Germany). The assay sensitivity for cytokines is 0.11–8.17 pg/ml. Myokine analyses were performed using the GDF-8/Myostatin Quantikine ELISA Kit (DGDF80) from R&D Systems (Minneapolis, MN, USA). The detection range of the Myostatin kit is 0.922–5.32 pg/ml. Antioxidant and metabolic response analyses (TAC, Pi and Ca2+) were assessed at 5, 10 and 30 min following the RT session. TAC was determined using a Total Antioxidant Capacity Assay Kit (MAK187-1KT) from Sigma-Aldrich. The detection range of the kit is 4–20 nmol/µl. Quantitative data were obtained using the Luminex-200 system (Luminex Corporation, Austin, TX, USA), and data analysis was performed with Luminex 100™ IS v2.3 software. Serum Pi and Ca2+ were analysed in a COBAS C-311 instrument from Roche (Indianapolis, IN, USA). The detection range of the kits is 0.62–5.54 mmol/l for Pi and 0.28–4.65 mmol/l for Ca2+. All procedures followed the manufacturers’ instructions. All analyses were performed in normoxia using the same equipment by specialised staff.
Statistical analyses
The data are generally presented as the mean ± standard deviation (SD), except the figures that present them as median and interquartile range. Shapiro–Wilk test was used to determine data distribution. The variables that did not follow a normal distribution were subjected to a transformation process. To determine the presence of outliers in the raw data, we employed the three-sigma rule of thumb method [2].
Firstly, differences between the environmental condition and time following the RT session were interpreted through repeated measures analysis of variance (ANOVA). A two-factor ANOVA with repeated measures was used to assess the effect of time during the recovery (within-group factor with 3 levels [minutes 5, 10 and 30]) and the environmental condition (inter-group factor with 2 levels [HH vs. N]) on the ions (i.e. Pi and Ca2+) and TAC. A second two-factor ANOVA with repeated measures was used to assess the effect of time during the recovery (within-group factor with 2 levels [minutes 5 and 30]) and the environmental condition (inter-group factor with 2 levels [HH vs. N]) on the cytokines (i.e. IL-6, TNF-α, IL-10 and myostatin). The pre-test value was included as a covariate to control participant variability. Significant main effects and interactions were subsequently analysed with Bonferroni post hoc tests. When the sphericity assumption for ANOVA was violated, we applied the Greenhouse–Geisser correction. Partial eta squared for main effects was calculated from the ANOVA (η2p) and was interpreted as ≥ 0.01 (small), ≥ 0.06 (medium) and ≥ 0.14 (large) [7]. Significant main effects and interactions were subsequently analysed with the Bonferroni post hoc test.
Secondly, paired-sample t tests were used to evaluate the within-group exercise effect (pre-exercise vs. peak post-exercise value) for each variable. Complementary independent-sample t tests were used to identify differences in the exercise effect (absolute delta changes [peak post-exercise value–pre-exercise value]) between environmental conditions (HH vs. N) for each variable. The IL-10/TNF-α ratio was also compared between HH and N and interpreted as a systemic pro/anti-inflammatory index [34].
Complementary to the previous tests (repeated measures ANOVA and t test), the magnitude of the changes was quantified using the standardized differences based on Cohen’s effect sizes (ES). These measures were calculated as the mean change (HH-N; 30–10 min or 10–5 min or 30–5 min; and post–pre exercise values) divided by the pooled SD for all pairs comparisons. The thresholds for interpretation of Cohen’s d were set as follows: < 0.2 (trivial), 0.21–0.5 (small), 0.5–0.8 (moderate), 0.8–1.3 (large) and > 1.30 (very large) [17]. All analyses were performed using IBM SPSS Statistics version 28.0.1.0 for MacOS (IBM Corp., Armonk, NY, USA). The level of significance was set at p < 0.05.
Results
The results from intra-group (extreme post-exercise value vs. pre-exercise) and inter-group (HH vs. N) exercise effects are presented in Table 2. Compared with pre-exercise, RT session increased serum TAC levels in N (ES > 0.93 [95% CI 0.21, 1.62]; p = 0.011), and myostatin (ES > 0.75; all p < 0.041) and circulating Ca2+ in both conditions in a similar magnitude (ES > 1.16; all p < 0.005). Compared with N, HH showed a very large increase in IL-10 (ES = 1.31 [95% CI 0.32, 2.27]; p < 0.009). Similarly, exercise in HH maintained elevated TNF-α (ES = 1.10 [95% CI 0.14, 2.03]; p = 0.024) after RT with respect to N, while IL6 displayed no changes throughout the 30 min of recovery. Moreover, there was a moderate but non-significant exercise effect between conditions for TAC and Pi. IL-10/TNF-α ratio showed large increments in both groups after exercise (ES > 1.36; all p < 0.002) with no differences between them (ES = 0.02 [− 0.86, 0.90]; p = 0.96).
The serum cytokine recovery kinetics results are shown in Fig. 2a–c. IL-6 displayed large individual variability, which made it difficult to detect any change (Fig. 2a). Contrary, TNF-α displayed an environmental (F1,17 = 10.684; p = 0.005; η2p = 0.39) and a time effect (F1,17 = 11.294; p = 0.004; η2p = 0.40) during recovery (Fig. 2c). Pairwise comparisons revealed large increases for TNF-α in HH at 5 and 30 min following the RT session (all p < 0.05) (Fig. 2c). IL-10 only displayed an environmental effect during recovery (F1,18 = 4.608; p = 0.047; η2p = 0.21). The pairwise comparison test yielded a large increase in IL-10 favouring HH at 5 min after the RT (p = 0.02) (Fig. 2b).
Analysis of circulating cytokines IL-6 (a), IL-10 (b), and TNF-α (c) response throughout the 30 min of recovery. Boxes represent the median and interquartile range, whiskers minimum to maximum values. p-value (p < 0.05), partial eta squared from ANOVA (η2p), Cohen’s d effect size (ES). ES was calculated as (30–5 min post-exercise) or (HH-N) divided by the pooled standard deviation. Pre-exercise values were included as covariates
Figure 3 displays the box plots of serum myostatin levels. Post-exercise results revealed a moderate but nonsignificant reduction in HH conditions at minute 30 of the recovery (ES = − 0.71; p = 0.21).
Analysis of circulating myostatin throughout the 30 min of recovery. Boxes represent the median and interquartile range, whiskers minimum to maximum values. p-value (p < 0.05), partial eta squared from ANOVA (η2p), Cohen’s d effect size (ES). ES was calculated as (30–5 min post-exercise) or (HH-N) divided by the pooled standard deviation. Pre-exercise values were included as covariates
TAC serum levels are shown in Fig. 4. Results displayed similar post-exercise results between conditions (p > 0.05).
Total antioxidant capacity changes throughout the 30 min of recovery. Boxes represent the median and interquartile range, whiskers minimum to maximum values. p-value (p < 0.05), partial eta squared from ANOVA (η2p), Cohen’s d effect size (ES). ES was calculated as (30–10 or 10 − 5 or 30 − 5 min post-exercise) or (HH-N) divided by the pooled standard deviation. Pre-exercise values were included as covariates
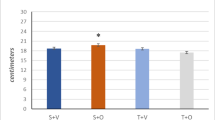
Figure 5a, b shows the serum Pi and Ca2+ levels throughout the 30-min recovery period. Post-exercise Ca2+ and Pi exhibited no differences between conditions (p > 0.05). Both groups showed large Pi removal from the bloodstream immediately after the RT session (ES < − 2.22; all p < 0.001).
Circulating calcium (a) and inorganic phosphate (b) response throughout the 30 min of recovery. Boxes represent the median and interquartile range, whiskers minimum to maximum values. p-value (p < 0.05), partial eta squared from ANOVA (η2p), Cohen’s d effect size (ES). ES was calculated as (30–10 or 10–5 or 30–5 min post-exercise) or (HH-N) divided by the pooled standard deviation. Pre-exercise values were included as covariates
Discussion
This study aimed to analyse the impact of RT in acute moderate HH on the muscle health. For this endeavour, the effect of a RT session on TAC, myostatin, several metabolites and pro- and anti-inflammatory modulation was measured throughout 30 min of recovery in N and acute moderate HH conditions. The main findings revealed an immediate and proportional moderate to very large increase in circulating IL-10 and TNF-α after RT in HH compared with N, suggesting a balanced pro/anti-inflammatory response with no clear impact on the metabolic, TAC and muscle atrophy biomarkers.
Combining the RT session with the ascent in altitude is expected to intensify the metabolic stress response. Conversely, our results failed to find clear increases in circulating Pi and Ca2+ after exercise in HH. Compared with pre-exercise, there was a similar reduction rate in serum Pi in N and HH throughout the first 5 min following the RT session. Consistently, other studies have reported no changes in circulating Pi concentrations 30 min after similar RT exercise between normoxia and moderate hypobaric hypoxia [11]. Pi clearance happens in the first minutes of recovery and is associated with the normal restoration of cellular functional demands involved in the adenosine triphosphate (ATP) synthetic rate. The 5-min time window until the first blood draw in this study may not detect the expected changes in this analyte. Similarly to other research [11], our results revealed an immediate and large increase of serum Ca2+ after the RT session regardless of the environmental condition (see Table 2). Although we did not find differences in the adjusted peak post-exercise Ca2+ value between conditions, the Ca2+ clearance was significantly higher at the end of the recovery period in N (ES = − 1.87; p < 0.001) (Fig. 5a). Maintenance of circulating Ca2+ levels above baseline in HH throughout the recovery with respect to the N group could suggest a net increase in the absolute magnitude of the metabolic stress response in HH.
The available research has reported a fast IL-6 increase after RT in N followed by a gradual reduction to baseline concentrations within 4 h [5, 14]. Additionally, RT in hypoxia promotes anaerobic metabolism [18] and the upregulation of the inflammatory adaptative response. However, consistent with the absence of clear differences in the impact of the RT session analysed on the metabolic stress response between N and HH, the release of IL-6 in this study displayed a large variability that limits conclusive results (Table 2 and Fig. 2a). Conversely, serum TNF-α concentration showed a large increase in the magnitude of the inflammation after RT in HH throughout the recovery period with respect to N (Fig. 2c). Contrary to similar studies [5], the circulating TNF-α absolute delta change remained notably higher under HH compared with N (Table 2). Immediately after the RT session in HH, IL-10 increased at 5 min post-exercise, and there inducing a progressive reduction in TNF-α secretion into the bloodstream [33] (see Fig. 2b, c). Benavente et al. [4] also found a moderate to large but non-significant increase in the absolute peak values of IL-6, IL-10 and TNF-α in acute HH after similar RT exercise. The use of a longer rest period between sets (2 min) and the ingestion of a high-carb protein bar before RT in the Benavente et al. study could contribute to mitigate the acute post-exercise inflammatory response [26] and partially explain the differences between the studies. Unfortunately, the absence of data related to this topic makes it difficult to compare our results in a more consistent way. An inflammatory response based on TNF-α may negatively impact muscle remodelling and activation of growth pathways [36]. However, there were no significant differences in the post-exercise IL-10/TNF-α ratio [34] between the groups, indicating that each group had a similar anti-inflammatory status. The greatest impact of RT in HH on the serum IL-10 concentration suggests a larger modulation of the anti-inflammatory mechanisms [16] that must be further investigated. Notwithstanding, our data indicate a positive balance of the pro/anti-inflammatory mechanisms involved in counteracting the adverse consequences induced by a high-intensity RT under acute HH conditions.
Previous research described significant suppression of myostatin messenger ribonucleic acid (mRNA) during recovery in HH compared with NH and N in endurance athletes [32]. Contrary, in accordance with the results of our study, in RT exercise under acute NH, Britto et al. [5] observed an increase in myostatin mRNA within 4 h of exercise, concluding that the RTH seems to potentiate myogenesis through inflammation rather than protein balance alteration. Conversely, our results depicted a moderately lower rise of circulating myostatin after exercise in HH than in N (Table 2 and Fig. 3). Additionally, only HH depicted a moderate non-significant decline (ES = − 0.72; p = 0.21) in myostatin levels 30 min post-exercise (Fig. 3). The regulation of myostatin expression can be explained, almost in part, by the overexpression of IL-10 and follistatin, both myostatin inhibitors [10]. Previous studies have reported a relationship between an increase in follistatin in response to RT exercise and hypoxia exposure, among other factors [41]. Consistently, we found a large increase in serum IL-10 in HH following the RT session while it remained similar to the pre-exercise in the N group (Fig. 2b and Table 2). The increase in IL-10 negatively affects the inflammatory response and consequently could restrict the increase in myostatin [19], as shown in the HH group, and stimulate muscle remodelling. In the Britto et al. [5] study, the IL-10 did not display any influence of exercise or hypoxic exposure. Differences in the procedure, such as the type of hypoxia (HH vs. NH), and the fact that recovery was conducted under normoxia conditions in the Britto et al. research, undoubtedly affect this result. Additional research is needed to elucidate the underlying mechanisms of the muscle remodelling process and cell differentiation pathways under hypoxic conditions.
Finally, a slight increase in TAC was observed in the N group after the exercise (Table 2). However, this increase was deemed of limited significance, as all recorded values for both groups remained well within the established normal range throughout the study [1]. Furthermore, consistent with Park et al. (36), serum TAC levels remained unchanged throughout the recovery in both conditions (Fig. 4). The stability in TAC levels did not impact on the inflammatory response through RONS-mediated signalling pathways.
This research has some limitations that should be noted: (1) only a few studies address the combination of HH and RT protocols on muscle health–related parameters, which limits the comparison of our results. (2) Future studies should incorporate a crossover design to control intra-group variability. (3) Sample size was relatively small, which could influence the width of probability distributions across the outcomes. However, it must be considered that this population is of interest and is understudied, probably due to the high economical cost associated with the analysis of the procedure and the high personal cost associated with the data acquisition through vein canalisation. These results could be used for larger confirmatory studies.
Conclusion
In summary, the results suggest the increment of the inflammation response after a RT exercise in acute HH compared with the same exercise in N. However, the absence of a clear impact of the hypoxia on the metabolic, TAC and muscle atrophy biomarkers only allow a partial acceptance of the hypothesis of this study. In addition, HH also promoted a proportional large increase in IL-10 suggesting an anti-inflammatory response that ensures pro/anti-inflammatory balance. The potential association between the IL-10, myostatin and TNF-α response could favour muscle remodelling activity after a high-intensity exercise in HH, although this postulation requires further research.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Azizbeigi K et al (2014) Antioxidant enzymes and oxidative stress adaptation to exercise training: comparison of endurance, resistance, and concurrent training in untrained males. J Exerc Sci Fit 12(1):1–6
Bargees A, Al-Shuhail AA (2022) First arrival picking of zero-phase seismic data by Hilbert ENVELOPE EMPIRICAL HALF WINDOW (HEEH) method. Sensors 22(19):7580
Bärtsch P, Gibbs JSR (2007) Effect of altitude on the heart and the lungs. Circulation 116(19):2191–2202
Benavente C et al (2021) Hormonal and inflammatory responses to hypertrophy-oriented resistance training at acute moderate altitude. Int J Environ Res Public Health 18(8):4233
Britto FA et al (2020) Acute environmental hypoxia potentiates satellite cell-dependent myogenesis in response to resistance exercise through the inflammation pathway in human. FASEB J 34(1):1885–1900
Brzycki M (1993) Strength testing—predicting a one-rep max from reps-to-fatigue. J Phys Educ, Recreat Dance 64(1):88–90
Cohen J, Statistical power analysis for the behavioral sciences. New York, NY: Roudledge Academic. Computing R Foundation for Statistical Computing, Vienna, Austria, 1988
D’Souza DM, Al-Sajee D, Hawke TJ (2013) Diabetic myopathy: impact of diabetes mellitus on skeletal muscle progenitor cells. Front Physiol 4:379
Enes A et al (2021) Rest-pause and drop-set training elicit similar strength and hypertrophy adaptations compared with traditional sets in resistance-trained males. Appl Physiol Nutr Metab 46(11):1417–1424
Feraco A et al (2021) Exploring the role of skeletal muscle in insulin resistance: lessons from cultured cells to animal models. Int J Mol Sci 22(17):9327
Feriche B et al (2020) Altitude-induced effects on muscular metabolic stress and hypertrophy-related factors after a resistance training session. Eur J Sport Sci 20(8):1083–1092
Forti LN et al (2017) Effects of resistance training at different loads on inflammatory markers in young adults. Eur J Appl Physiol 117:511–519
Fountain WA et al (2023) Controlling inflammation improves aging skeletal muscle health. Exerc Sport Sci Rev 51(2):51–56
Hennigar SR, McClung JP, Pasiakos SM (2017) Nutritional interventions and the IL-6 response to exercise. FASEB J 31(9):3719–3728
Ismaeel A et al (2019) Resistance training, antioxidant status, and antioxidant supplementation. Int J Sport Nutr Exerc Metab 29(5):539–547
Izquierdo M et al (2009) Cytokine and hormone responses to resistance training. Eur J Appl Physiol 107:397–409
Juandi D et al (2021) The effectiveness of dynamic geometry software applications in learning mathematics: a meta-analysis study. 2021
Jung W-S et al (2021) Resistance training in hypoxia as a new therapeutic modality for sarcopenia—a narrative review. Life 11(2):106
Kazemi F (2016) The correlation of resistance exercise-induced myostatin with insulin resistance and plasma cytokines in healthy young men. J Endocrinol Invest 39:383–388
Khalafi M et al (2023) Impact of exercise in hypoxia on inflammatory cytokines in adults: a systematic review and meta-analysis. Sports Medicine-Open 9(1):1–14
Li J et al (2020) The molecular adaptive responses of skeletal muscle to high-intensity exercise/training and hypoxia. Antioxidants 9(8):656
Maiti S et al (2014) Mathematical modeling of pro-and anti-inflammatory signaling in macrophages. Processes 3(1):1–18
Malkov MI, Lee CT, Taylor CT (2021) Regulation of the hypoxia-inducible factor (HIF) by pro-inflammatory cytokines. Cells 10(9):2340
Nakajima T et al (2018) Muscle hypertrophy following blood flow-restricted, low-force isometric electrical stimulation in rat tibialis anterior: role for muscle hypoxia. J Appl Physiol 125(1):134–145
Nemes R et al (2018) Reactive oxygen and nitrogen species regulate key metabolic, anabolic, and catabolic pathways in skeletal muscle. Antioxidants 7(7):85
Nieman DC, Wentz LM (2019) The compelling link between physical activity and the body’s defense system. J Sport Health Sci 8(3):201–217
Pamenter ME et al (2020) Cross-species insights into genomic adaptations to hypoxia. Front Genet 11:743
Pedersen BK et al (2017) Role of myokines in exercise and metabolism. J Appl Physiol 2007
Rodriguez-Miguelez P et al (2015) Hypoxia-inducible factor-1 modulates the expression of vascular endothelial growth factor and endothelial nitric oxide synthase induced by eccentric exercise. J Appl Physiol 118(8):1075–1083
Rogeri PS et al (2020) Crosstalk between skeletal muscle and immune system: which roles do IL-6 and glutamine play? Front Physiol 11:582258
Rosales AM et al (2022) Independent effects of acute normobaric hypoxia and hypobaric hypoxia on human physiology. Sci Rep 12(1):19570
Ross CI et al (2019) Skeletal muscle mRNA response to hypobaric and normobaric hypoxia after normoxic endurance exercise. High Alt Med Biol 20(2):141–149
Rossato M et al (2012) IL-10–induced microRNA-187 negatively regulates TNF-α, IL-6, and IL-12p40 production in TLR4-stimulated monocytes. Proc Natl Acad Sci 109(45):E3101–E3110
Shamsi MM et al (2017) Combined effect of aerobic interval training and selenium nanoparticles on expression of IL-15 and IL-10/TNF-α ratio in skeletal muscle of 4T1 breast cancer mice with cachexia. Cytokine 90:100–108
Sriram S et al (2011) Modulation of reactive oxygen species in skeletal muscle by myostatin is mediated through NF-κB. Aging Cell 10(6):931–948
Torre-Villalvazo I et al (2019) Protein intake and amino acid supplementation regulate exercise recovery and performance through the modulation of mTOR, AMPK, FGF21, and immunity. Nutr Res 72:1–17
Townsend JR et al (2015) TNF-α and TNFR1 responses to recovery therapies following acute resistance exercise. Front Physiol 6:48
Turner G et al (2017) The time course of endogenous erythropoietin, IL-6, and TNFα in response to acute hypoxic exposures. Scand J Med Sci Sports 27(7):714–723
Van de Vyver M et al (2016) Neutrophil and monocyte responses to downhill running: intracellular contents of MPO, IL-6, IL-10, pstat3, and SOCS 3. Scand J Med Sci Sports 26(6):638–647
Verzola D et al (2019) Emerging role of myostatin and its inhibition in the setting of chronic kidney disease. Kidney Int 95(3):506–517
Zhang L et al (2018) The emerging role of follistatin under stresses and its implications in diseases. Gene 639:111–116
Acknowledgements
The authors thank the High-Performance Center of Sierra Nevada, Spain, and all the participants who volunteered for this investigation.
Funding
Funding for open access publishing: Universidad de Granada/CBUA This research was funded by the Spanish Ministry of Science, Innovation and Universities (grant number PGC2018-097388-B-I00-MCI/AEI/FEDER, UE) and the FEDER/Junta de Andalucía-Ministry of Economic Transformation, Industry, Knowledge and Universities (grant number B-CTS-374-UGR20).
Author information
Authors and Affiliations
Contributions
Conceptualization: B.F., P.P., J.L.; methodology: B.F., P.P.; formal analysis and investigation: S.P.R., C.B., B.F., P.P.; writing original draft preparation: B.F., P.P.; writing—review and editing: S.P.R., B.F., J.L., F.A., C.B., P-P.J.D.; funding acquisition: B.F., P.P.; Resources: B.F., P.P.; supervision: B.F., J.L. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (protocol code 10/18 and date of approval 06/11/2018).
Consent to participate
Written informed consent was received from all participants involved in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pérez-Regalado, S., León, J., Padial, P. et al. Effect of a resistance exercise at acute moderate altitude on muscle health biomarkers. Pflugers Arch - Eur J Physiol 476, 49–57 (2024). https://doi.org/10.1007/s00424-023-02868-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-023-02868-y