Abstract
Deep brain stimulation (DBS), a treatment for modulating the abnormal central neuronal circuitry, has become the standard of care nowadays and is sometimes the only option to reduce symptoms of movement disorders such as dystonia. However, on the one hand, there are still open questions regarding the pathomechanisms of dystonia and, on the other hand, the mechanisms of DBS on neuronal circuitry. That lack of knowledge limits the therapeutic effect and makes it hard to predict the outcome of DBS for individual dystonia patients. Finding electrophysiological biomarkers seems to be a promising option to enable adapted individualised DBS treatment. However, biomarker search studies cannot be conducted on patients on a large scale and experimental approaches with animal models of dystonia are needed. In this review, physiological findings of deep brain stimulation studies in humans and animal models of dystonia are summarised and the current pathophysiological concepts of dystonia are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For decades, clinicians and scientists have searched for a model of the pathophysiology of dystonia, the third most common movement disorder after Parkinson’s disease and essential tremor with a prevalence of 0.03 to 0.06% of the population [30, 33]. Dystonia is a heterogeneous hyperkinetic neurological movement disorder characterised by sustained or intermittent involuntary muscle contraction, which leads to abnormal and often repetitive movements or postures, or both [2].
In 2013, dystonia was reclassified into a bi-axial system, with Axis I referring to clinical characteristics, and Axis II to aetiology. This system is now widely used [2, 33]. If dystonia is the only motor dysfunction, it is classified as isolated dystonia (previously referred to as “pure”, “idiopathic”, or “primary”). Dystonia may also occur in combination with other movement disorders (also known as secondary dystonia in the past), such as myoclonus or parkinsonism [2]. In the following, the term “dystonia” only refers to isolated dystonia in this review. It is hard to clarify the pathophysiology of the broad spectrum of symptoms and multiple causes, including several genetic types of dystonia [106]. Even if dystonia affects several muscle groups, the origin of the pathomechanisms is the central nervous brain. Numerous studies emphasise the role of the cortico-basal ganglia-thalamo-cortical and cerebellar-thalamo-cortical networks in the pathophysiology of dystonia, whereby different forms of dystonia may have different origins. In multiple brain regions, such as the basal ganglia, thalamus, brainstem, or cerebellum, microstructural abnormalities have been reported for a few specific forms of dystonia [66]. Although lesions can cause dystonia, there is generally no evidence of anatomical abnormalities in isolated dystonia [9]. Instead, it is debated that genetic and functional network factors cause dystonia. Here, several brain regions may be differentially affected, and various forms of dystonia may include several responsible genes, which makes it hard to treat patients with dystonia optimally. Apart from dopa-responsive dystonia, there is no rational treatment option or a causal therapy (also due to the lack of a clear pathophysiological concept). Symptoms are usually treated by using physical (e.g. physiotherapy, transcranial magnetic stimulation), pharmacological (e.g. botulinum toxin injections, anticholinergic drugs), and surgical approaches in drug-refractory dystonia (e.g. deep brain stimulation, pallidotomy) [112]. Deep brain stimulation (DBS) appears to be the most promising procedure for treating [33]. Despite an increase in clinical trial datasets, it remains hard to predict the outcome of DBS for individual patients [121], which also depends on careful patient selection [22, 60]. To improve efficacy and reduce the risks of stimulation-induced side effects such as parkinsonism and dysarthria [82, 128], research and development are increasingly adopting the approach of adaptive DBS systems consisting of responsive, adaptive, and closed-loop control modes [62]. However, such adaptive DBS systems require electrophysiological biomarkers, e.g. local field potentials, to predict dystonic symptoms. These biomarkers can be used as a signal for punctually turning on the DBS within a closed-loop system to obviate dystonic movements.
This review summarises current pathophysiological concepts of isolated generalised dystonia. We are concentrating on recent electrophysiological findings helping to elucidate the pathomechanisms of generalised dystonia. Since it would go beyond the scope of the present review, here we do not dwell further on genetic factors and refer to the work of Christine Klein [57]. In addition, we discuss recent electrophysiological results from DBS studies in humans and animal models complemented by our hypotheses on the mechanism.
Hypotheses for the pathophysiology of isolated dystonia
Movement is controlled through the cortico-basal ganglia-thalamo-cortical loop of the central nervous system. Information from the cortex is directed to the striatum, a part of the basal ganglia, through glutamatergic afferents. The striatum modulates the information via cholinergic and GABAergic interneurons as well as dopaminergic and glutamatergic afferents from the midbrain and thalamus, respectively. Experimental studies established the first link between dystonia and a functional disturbance of the basal ganglia, especially in the cortico-striatal network [32, 95]. It was then thought that an imbalance between the direct and indirect pathways leads to excessive movement, but conclusive evidence for dystonia in humans is lacking [87]. As shown in Fig. 1, in the striatum, the cortical glutamatergic input is directly relayed to the globus pallidus internus (GPi), and the substantia nigra pars reticulata (SNr) (direct pathway). Moreover, cortical input is indirectly interconnected to the GPi via the globus pallidus externus (GPe) and the subthalamic nucleus (STN) (indirect pathway). For the sake of completeness, the hyperdirect pathway should also be mentioned here, which bypasses the striatum and forms a monosynaptic connection from cortical areas to STN, mediating rapid movement inhibition [20]. Basal ganglia output from the GPi/SNr is routed to ventral motor thalamic nuclei and forwarded to the frontal cortical areas. Moreover, the collaterals of the GPi/SNr projections run to the two primary components of the intralaminar thalamic nuclei, the center median (CM) and parafascicular (Pf) nuclei [125] (Fig. 1). CM and Pf neurons return projections to the striatal projection neurons (MSN; medium spiny neurons) and the aspiny interneurons. These interneurons may act as a feedback system that provides information on sensory events and are likely essential for arousal, attention, orientation, and action selection [64, 125]. In the classical model of basal ganglia function, the direct pathway is responsible for and facilitates desired movements, whereas the indirect pathway (although it can be co-activated for selected actions [21]) attenuates and inhibits unwanted movements [19, 39].
The cortico-basal ganglia-cerebellar-thalamo-cortical network. Movement formation is controlled by the motor circuitry, where the cortex, basal ganglia, cerebellum, and thalamus are interconnected and partly linked via collaterals, forming feedforward and feedback loops. Three pathways can be distinguished from each other: (1) the direct pathway, responsible for desired movements; (2) the indirect pathway is classically seen as a damping mechanism for undesired movements; and (3) the hyperdirect pathway, which bypasses the striatum and forms a monosynaptic connection from cortical areas to STN, mediating rapid movement inhibition. The green arrows represent glutamatergic inputs, the dark blue arrows represent dopaminergic inputs, and the red arrows represent inhibitory GABAergic inputs. The scaling of the nuclei is larger than the real anatomical sizes. Abbreviations: D1/D2, dopaminergic receptors class 1/2; STN, subthalamic nucleus; GPe/GPi, globus pallidus externus/internus; SNr/SNc, substantia nigra pars reticulata/compacta; VA, ventral anterior thalamic nucleus; VL, ventrolateral thalamic nucleus; VM, ventromedial thalamic nucleus; VA-VL-VM are part of the ventral motor thalamic nuclei (in red); CM-Pf, thalamic center median/parafascicular complex (figure created with BioRender.com)
Role of GABAergic inhibition
Regarding functional network factors, previous animal and human studies suggest reduced excitability of inhibitory connections at the cortical, brainstem, and spinal levels and a partial loss of inhibition [46]. The loss of inhibitory tone within the striatum is indeed one possible mechanism discussed for the pathophysiology of dystonia.
The striatal GABAergic projection neurons, the MSN, represent the main proportion of striatal neurons (~95 %). The remaining ~5 % are interneurons, however, significantly impacting striatal output. Three-quarters of the interneurons comprise GABAergic interneurons, which can be divided into five classes: fast-spiking, 5HT3a-expressing, neuropeptide Y-expressing, calretinin-expressing, and tyrosine hydroxylase-expressing [111]. In the dtsz mutant hamsters, an animal model of paroxysmal generalised dystonia, the maturation of fast-spiking striatal parvalbumin-positive GABAergic (PV+) interneurons is disturbed [13, 37]. Although the PV+ interneurons represent less than 5 % of total neurons in the striatum, the fast-spiking characteristic of these neurons (10–100 Hz) enables balancing MSN’s excitation coming from thousands of cortical glutamatergic excitatory inputs [39]. These fast-spiking interneurons balance the striatal activity and control the inhibitory tone of the striatum. PV+ interneurons are more responsive to excitatory cortical input than MSN, and due to their frequency-independent short-term synaptic plasticity, PV+ interneurons act as an attenuating filter for the MSN. Notably, the feedforward inhibition by PV+ interneurons of the MSN of the direct pathway seems to be stronger than that of the indirect pathway (Fig. 2) [39]. Therefore, a deficit of PV+ interneurons may have a more significant impact on the GABAergic MSN of the direct pathway and thus result in increased inhibition of GPi, which would consequently lead to less inhibition of the thalamus and could cause hyperkinetic movements. Single-unit recordings in the entopeduncular nucleus (EPN; homolog of the human GPi) of the dtsz mutant hamster confirm this assumption and indicate a reduced mean discharge rate [36]. However, a decreased firing rate of the GPi cannot be considered the primary cause of dystonia due to the ameliorating effect after pallidotomy (which is typically restricted to the sensorimotor portion of GPi) [36]. Therefore, an abnormal pattern of GPi activity may be more relevant than an altered discharge rate [36].
The intrastriatal network. The striatum plays an essential role within the movement loop and relays the glutamatergic cortical input. The striatal output to GPi (direct pathway) and the GPe (indirect pathway) is mediated through GABAergic projection neurons (medium spiny neurons, MSN), in which D1 or D2 receptors predominate, respectively. This striatal inhibitory output is modulated e.g. by GABAergic (PV+; parvalbumin-positive, purple) and cholinergic (CSI, green) interneurons as well as dopaminergic input (blue) from the substantia nigra pars compacta (SNc), glutamatergic thalamic, and cortical inputs. The small dots on the neurons and connections represent the appropriate dopaminergic, glutamatergic, and GABAergic synapses (figure created with BioRender.com)
Current theories stress the importance of spatial and temporal coding of activity patterns within GPi and SNr in the context of the overall network activity of the cortex, basal ganglia, thalamus, and cerebellum. Detections of local field potentials, which reflect the synchronised oscillatory synaptic activity surrounding a measuring electrode, demonstrated abnormal activity patterns with excessive pallidal low-frequency oscillation (delta and theta range; 4–12 Hz) in correlation to motor symptom severity in patients with cervical dystonia [79, 105]. Turning back to experimental data, in vivo extracellular single-unit recordings of the dtsz mutant hamster with delayed maturation of striatal PV+ interneurons demonstrated a significant shift toward an irregular burst-like firing of EPN neurons in comparison to non-dystonic control animals [36]. Neumann and colleagues, in addition, showed reduced pallido-cerebellar connectivity, the synchrony of which was inversely correlated to the degree of symptom severity in dystonia patients [70, 79]. The cerebellum, on his part, appears indirectly connected to the striatum via the intralaminar thalamic nuclei, which modulate striatal dopamine release on synapses of dopaminergic midbrain neurons [113]. Excessive pallidal theta activity may thus change the spatial and temporal coding in the basal ganglia-thalamic-cerebellar loop in total and lead to abnormal striatal transmitter release and the generation of dystonic muscle contraction.
Role of dopaminergic activity
Several dystonia forms have also been linked to dopaminergic dysfunctions. The neurotransmitter dopamine is released by afferents from the midbrain. Here, neurons from the ventral tegmental area (VTA) innervate the ventral striatum and neurons from the substantia nigra pars compacta (SNc) innervate the dorsal striatum. Dopamine affects the MSN directly via the D1-class or D2-class dopamine receptors (D1-DR or D2-DR, respectively) or indirectly via synaptically coupled neurons, e.g. GABAergic and cholinergic striatal interneurons (CSI). MSN directly projecting to the GPi/SNr (striatonigral) express high levels of D1-DR, while MSN of the indirect pathway (striatopallidal) strongly express D2-DR [110].
Dopamine concentrations and related metabolites are decreased in the dopa-responsive dystonia syndrome (Segawa syndrome), characterised by mutations in genes encoding enzymes involved in dopamine syntheses such as GCH1, TH, and SPR [9]. That dystonia form typically manifests as lower limb-onset dystonia and is characterised by a diurnal fluctuation of symptoms. Patients with dopa-responsive dystonia respond very well to treatment with the dopamine prodrug levodopa, even at low doses. In contrast, dopamine-depleting drugs sometimes improve other types of dystonia [112].
In DYT1 and DYT6 dystonia, the most common inherited forms of generalised dystonia, neuroimaging studies in patients and animal models revealed a significant reduction in the D2-DR availability and binding in the striatum [3, 15, 18]. In contrast to the D1-DR, primarily located on the postsynaptic site, the D2-DR can also be found at presynapses of glutamatergic and dopaminergic afferents and directly autoregulate the dopamine level in the striatum [23]. The D1-DR is coupled to Golf-protein, whose activation increases the intracellular cAMP level that leads to the activation of protein kinase A and affects various intracellular targets, e.g. voltage-dependent Na+ and Ca+ channels. The D2-DR is coupled to Gi/o protein, whose activation leads to adenylyl cyclase inhibition and phospholipase C stimulation. Overall, the activation of D1-DR facilitates the direct pathway by increasing the excitability of striatonigral MSN, while D2-DR activation restricts the indirect pathway by reducing the excitability of striatopallidal MSN [109]. Due to the heterogeneous distribution of receptors and synaptic inputs in the striatum, the overall effect of a dopaminergic dysfunction on the striatal output is hard to predict. Although reduced striatal D2-DR binding has been demonstrated in patients with DYT1 or DYT6 dystonia, animal models carrying the same DYT1 mutation and showing reduced striatal D2-DR binding are absent the dystonic motor symptoms [54]. However, in the symptomatic animal model of the dtsz mutant hamster, which displays the type of paroxysmal generalised dystonia, autoradiographic analyses demonstrated decreased dopamine D1- and D2-DR in the dorsomedial striatum [80]. In another study that investigated the striatal extracellular levels of dopamine by microdialysis, dopamine release was significantly increased in correlation with a dystonic attack in the dtsz mutant hamster [48]. Together with the findings in humans, these results suggest that overactivity of the dopaminergic system may be critically involved in the pathophysiology of dystonia. Besides the MSN, the D1- and D2-DR have also been identified in GABAergic interneurons and CSI. However, the interaction of dopamine and acetylcholine appears to play a crucial role in modulating striatal output [14, 32].
Role of cholinergic activity
An alternative pathophysiological hypothesis of dystonia assumes abnormal activity of cholinergic striatal interneurons (CSI) related to acetylcholine-dopamine imbalances [24, 32, 47, 85, 100]. CSI are a subgroup of tonically active neurons (TAN) which can be identified due to the expression of choline acetyltransferase. CSI are morphologically characterised by a sizeable polygonal soma (average 20–50 μm), aspiny dendrites, and an axon that branches densely and abundantly. Despite a small fraction of approximately 2 % of the overall striatal neuronal population, CSI regulate the duration, strength, and spatial patterns of striatonigral and striatopallidal MSN [102]. Due to a persistent Na+ current (via NaV1.6), Ca+-activated K+- currents (via CaV2.1, CaV2.2, BK- and SK- channels), and a hyperpolarization-activated cation current If, CSI show an autonomous activity of rhythmic single spiking (~5 Hz), even in the absence of synaptic inputs [12, 41, 78]. However, like TAN, the spontaneous firing pattern is synchronously paused, which is, on the one hand, mediated primarily by dopaminergic (acting via D2-DR) and partly by GABAergic afferents arising from SNc [27, 28, 96, 108]. On the other hand, the inhibition of CSI is mediated by intrastriatal GABAergic interneurons, for which tyrosine hydroxylase-expressing interneurons seem to be mainly responsible [28, 31]. This pause could be shown to respond to reward-related stimuli and is thought to act as a temporal window for the induction of synaptic plasticity in MSN [28, 41, 101]. Moreover, the synchronised pause exhibits variable patterns concerning the aforegoing bursts and the rebound spiking mediated by the CM-Pf complex [28, 96]. In the mouse model of DYT1 dystonia, an abnormal pause response in CSI was reported after repetitive thalamic stimulation [99]. It has been shown that the pause abnormality is caused by an altered activity of the D2-DR in CSI, which paradoxically excites the CSI rather than inhibiting it, as would be expected physiologically [32, 99]. A possible reason for the paradoxical effect of the D2-DR activity is an increase in the inhibitory coupling of D2-DR to the CaV2.2 channels, which, in turn, reduces Ca2+-activated SK-currents in CSI [99, 100]. Consequently, the abnormal activity of CSI affected the cortico-striatal synaptic communication of the MSN at presynapses via M4 and at postsynapses via M1 receptors [99].
Acetylcholine modulates the activity of striatonigral MSN through muscarinic M1 and M4 receptors, while in striatopallidal MSN, the M1 receptor is the predominant one. M1 receptors are coupled to Gq/11 and are found on the dendrites and spines. Activation of M1 receptors enhances NMDA-receptor mediated currents and persistent Na+ currents, modulates Ca2+-currents, reduces KCNQ and Kir2 currents, and in the end, promotes depolarisation of MSN [1, 32]. The M4 receptor activation (coupled to Gi/o) leads to an inhibition of adenylate cyclase (AC) that mediates the inhibition of CaV2.1 and CaV2.1 [1]. The suppression of AC also opposes the D1-DR-induced cAMP/protein kinase A (PKA) signalling pathway in the striatonigral MSN, which induces long-term potentiation (LTP) at cortico-striatal synapses [1, 32, 78, 101]. It has been shown that M4 and D1 receptors interact asymmetrically in striatonigral MSN. That means that activation of the M4 receptor before activation of the D1 receptor leads to increased action potential frequency of striatonigral MSN. In contrast, prior activation of the D1 receptor causes a decrease in action potential frequency [51, 78].
Muscarinic acetylcholine receptors are widely expressed and identified on all striatal neurons, as autoreceptors on CSI, and on the axon terminals of most striatal afferents, except on dopaminergic midbrain neurons, where there is no anatomical evidence for the presence [5, 40, 113]. The expression of nicotinic acetylcholine receptors, with α7 and α4β2* as the most common subtypes in the striatum, is limited to the postsynapse of striatal interneurons and presynapse of striatal afferents [5]. The latter plays a crucial role in releasing dopamine from inactive midbrain afferents. With the help of fast-scan cyclic voltammetry, Threlfell and colleagues measured dopamine release extracellularly on presynapses of the non-active midbrain neurons due to endogenous striatal acetylcholine release via CSI [113].
Conversely to the modulation of acetylcholine on dopaminergic neurons, dopamine modulates the CSI through D2 and D5 receptors, at which D2 postsynaptic receptors have been identified as the key mediators whose activation leads to reduced release of acetylcholine [32]. As mentioned above, in DYT1 dystonia, D2-DR activation leads to a paradoxical excitation of the CSI [99]. Interestingly, imaging studies in human DYT1 dystonia patients indicated an age-dependent lower expression of vesicular acetylcholine transporters (VAChT) in the striatum and cerebellum [73]. VAChT is involved in the vesicular storage of acetylcholine in the presynapses of cholinergic neurons and is a potent indicator for acetylcholine release. A reduced VAChT expression and, therefore, a possible decrease in the extracellular acetylcholine levels within the striatum in young symptomatic humans seem to contrast with the hypothesis of hypercholinergic activity in the asymptomatic DYT1 mouse model. Mazere et al. discuss that contradiction as a consequence of synaptic physiology and disease duration [73]. Decreased VAChT expression was detected only in young human patients, where the putamen is involved in procedural learning of motor routines. In older patients with a lower learning demand, there is no aberrance in VAChT level against healthy controls. Age-dependent changes in the VAChT level were interpreted as a compensatory mechanism for excessive CSI activity induced by the abnormal D2-DR activity, which is again in line with the hypothesis from the DYT1 mouse model [73].
Role of adenosine receptors
Endogenous adenosine should also be considered in the pathophysiology of dystonia [90]. High levels of adenosine receptors are expressed in the striatum. A2A adenosine receptors co-expressing with the D2-DR in striatopallidal MSN [17, 34, 117] are particularly interesting. A2A receptors are also present (although less frequently) in presynaptic excitatory and inhibitory terminals. Flagmeyer and colleagues proved a modulation of the cortico-striatal and thalamo-striatal glutamatergic neurotransmission in the presence of an A1 adenosine receptor agonist [34]. In a study by Tozzi and colleagues, the A2A and the D2-DR modulate the excitatory cortico-striatal transmission [117]. In the adult-onset dystonia DYT25, characterised by gene mutation encoding the stimulatory G-Protein Gαolf (GNAL), the cAMP pathway in the MSN is disordered. Since Gαolf is coupled to the A2A adenosine receptors of the striatonigral D2-DR MSN, the receptor becomes more and more attractive in the concept of the pathophysiology of dystonia [83].
Role of glutamatergic thalamo-striatal and cortico-striatal projections
Several lines of evidence indicate abnormal cortico-striatal activity in dystonia [49, 72], but in addition to the cortical input, MSN receive quantitatively similar glutamatergic inputs through thalamo-striatal synapses [6, 26, 76] (Fig. 2). The thalamic glutamatergic innervation, mainly arising from the CM-Pf complex, has also been mentioned for CSI, GABAergic interneurons, and nigrostriatal terminals, and partially with contrastive effects regarding synaptic plasticity [6]. The initial glutamatergic release probability at the thalamo-striatal synapse formed on MSN appears higher than at the cortico-striatal synapse since the former expresses paired-pulse depression, in contrast to paired-pulse facilitation in the cortico-striatal synapse after repetitive stimulation [26, 40].
The thalamic inputs exert a significant excitatory influence on CSI, while PV+ interneurons and MSN were primarily excited through cortical inputs [6, 41]. Thalamo-striatal activity driven by salient stimuli is responsible for the burst and pause pattern in the CSI that is otherwise spontaneously active at low frequencies of approximately 5 Hz [27]. It has been demonstrated that the pause coincides with an increased discharge activity in dopaminergic midbrain neurons (SNc). Together with the findings from Reynold and colleagues [89], increased striatal dopamine level simultaneous to the pause in activity of CSI is speculated to underlie learning goal-directed behaviour very likely mediated by the basal ganglia-thalamo network.
Role of striatal synaptic plasticity
It is commonly accepted that the strength of excitatory glutamatergic synapses on MSN is involved in motor skill acquisition. Dysregulation has been implicated in several movement disorders, including dystonia and Parkinson’s disease [69, 101].
The polarity of long-term plasticity (depression or potentiation) at excitatory synapses onto MSN appears to depend on the coincidence of phasic dopamine activity, pause in CSI activity, and depolarised MSN [89]. Long-term potentiation (LTP) on cortico-striatal synapses requires isochronic elevated dopamine release, paused CSI activity, and depolarised postsynaptic MSN. Otherwise, if one of them is missing, it results in long-term depression (LTD) or no effect [89]. Going into detail, in striatopallidal MSN, LTD requires the activation of Gi/o protein-coupled D2-DR, which decreases adenylate cyclase activity and silences A2A receptors that mediate LTP. Moreover, postsynaptic mobilisation of endocannabinoids through the metabotropic glutamate receptor mGluR5 and L-type calcium channels induced LTD in the indirect pathway MSN [69, 101]. Endocannabinoids retrogradely diffuse across the synaptic cleft and activate the cannabinoid receptor CB1 at the presynapse. Activation of CB1 leads to decreased release probability of the presynapse and results in LTD. In direct-pathway striatonigral MSN, the mechanism of LTD induction by presynaptic activation of CB1 receptors seems similar to the indirect-pathway striatopallidal MSN. However, striatopallidal MSN does not express A2A and D2-DR, and, in contrast to the striatopallidal MSN, activation of the D1-DR prevents the induction of LTD [69, 101]. The critical mediator for LTD induction in striatonigral is assumed to be the Gi/o protein-coupled M4 receptor, whose role has not been investigated so far [69, 101]. However, the M4 receptor may act similarly to the D2-DR in striatopallidal MSN by decreasing the AC and suppressing the activity of the D1-DR [101].
LTP, as opposed to LTD, is only a mechanism in the postsynapse depending on NMDA receptor activation [69]. One unwanted adverse reaction of L-DOPA treatment in early- and mid-stage PD patients is dyskinetic movements, which are assumed to be pathological LTP of cortico-striatal synapses due to abnormal increase of D1-DR signalling [101]. In the striatonigral MSN of the direct pathway, activated Golf-protein coupled D1-DR led to increased activity of PKA. That, in turn, raises the phosphorylation of the NMDA receptor subunit NR2B, which enhances the receptor currents and may lead to LTP induction [69, 101]. In the indirect pathway MSN, the mechanisms are supposed to be similar to the direct pathway MSN, while enhancement of PKA activity is mediated by the A2A receptor [69, 101].
The complex mechanisms of synaptic plasticity of MSN reflect the crucial role of granular time-scaled activation of dopamine, acetylcholine, and adenosine receptors. It is widely assumed that plasticity at cortico-striatal synapses underlying motor learning is a critical factor in the pathophysiology of dystonia [8, 49, 87, 114]. There is evidence from clinical and experimental studies for abnormal synaptic plasticity and a prevailing in LTP, which lead to abnormal sensorimotor integration and consolidation of motor engrams [87]. The delayed effect of deep brain stimulation (DBS), which, in contrast to PD, could take several days, weeks, or even months, pointed out the abnormal plasticity that may be reorganised by the stimulation [10, 44, 49, 63, 84, 94, 124].
In summary, the current hypotheses on the pathophysiology of dystonia consider the dysfunctional effect on parts of the entire motor circuitry. The nuclei of the motor loop are interconnected, partly also linked via collaterals, and form feedforward and feedback loops. For several years, dystonia has been increasingly understood as an extensive network dysfunction involving the basal ganglia and the thalamus, cerebellum, and sensorimotor cortices [9, 56, 66, 70]. To elucidate the pathophysiology of the different forms of dystonia, the entire cortico-basal ganglia-thalamo-cortical network should be considered. Furthermore, cerebellar involvement has to be considered due to evidence of pathological cerebellar output transmitted to basal ganglia via the thalamus [88]. All in all, dystonia appears to be a network disorder, and besides the specific nuclei, the oscillatory patterns across the nuclei must be analysed. Due to the ethical limitations in human patients, especially due to the impossibility of obtaining data mirroring the physiological situation in healthy persons, symptomatic animal models are required to study the hypothesis of the pathophysiology of dystonia. In particular, multi-unit recordings in the mentioned brain areas are needed to elucidate the internal network communication patterns.
Deep brain stimulation in dystonia
Deep brain stimulation (DBS) is an essential electroceutical treatment option that allows for adjustable stimulation in neurological and psychiatric disorders correlated with dysfunctional neural circuitry [71]. It is widely used to treat movement disorders such as Parkinson’s disease (PD), tremors, and dystonia. After receiving FDA and Conformité Européene (CE) approvals, treatment with DBS became the standard of care in movement disorders [62]. Current DBS systems for clinical use consist of intracranial electrode(s), extension wire(s), and an implantable battery-operated pulse generator. Due to the attachment of proteins and cells directly to the DBS electrode surface and an accumulation of extracellular matrix proteins and glial cells, the impedance of the electrode-tissue interface varies over time [68]. For DBS with voltage pulses, the varied impedance caused instabilities in voltage magnitudes. Thus, the voltage induced in the brain tissue would deviate from the target voltage and require frequent programmed parameter adjustment. Current-controlled DBS, in contrast, minimises these voltage fluctuations generated by impedance changes [67]. Therefore, a current-controlled stimulation is preferred over voltage-controlled stimulation for an optimal DBS treatment.
Due to lower morbidity and reversibility, DBS has increasingly been preferred over thalamotomy or pallidotomy for dystonia [61, 97]. In 1977, Mundinger published the first data on short-term intermittent thalamic DBS (30 min several times per day for up to 8 months) in 7 patients with cervical dystonia [77]. Since then, many patients have been effectively treated with DBS. Fan and colleagues recently analysed the effectiveness of GPi-DBS and STN-DBS in different types of dystonia based on published literature with the help of the Meta-analysis of Observational Studies in Epidemiology [33]. They confirmed GPi- and STN-DBS to be safe methods and provided evidence for improvement of the quality of life in patients with dystonia. Symptoms of patients with focal dystonia generally improved better than patients with segmental dystonia, and patients with primary dystonia had a better response than those with secondary dystonia. All in all, the improvement of dystonia severity is reported by 50 to 60 % for patients with segmental or generalised or cervical dystonia treated with high-frequency pallidal (GPi) DBS [16, 25, 55, 65, 71, 120, 122, 123].
Electrophysiological data in patients with dystonia treated with DBS suggest modifications of the synaptic plasticity within the cortical motor circuit [114]. With electrophysiological studies from primates and patients, DBS can be described as a functional blockade of transmission of information, also known as the term “informational lesion”, that alters the activity of axons within the volume of tissue activated [42, 124]. However, DBS has to be more than a disconnection of the pathological area through the synaptic blockade. In imaging studies with positron emission tomography, DBS treatment enhanced the prefrontal or frontal cortico-basal ganglia-thalamocortical loop [124]. It is therefore assumed that DBS acts as a selective filter, which, on the one hand, functionally decouples the structure being stimulated. Moreover, on the other hand, it leads to activation of the structures within the volume of activated tissue, which results in a more regular firing pattern and changes in bursting activity already seen in local field recordings in patients treated with DBS [74, 79, 115, 124].
Given the diversity of dystonia in patients, such as type and age at the onset of dystonia, questions arise regarding optimal DBS targeting and adapted individualised stimulation settings. More data from specific dystonia subtypes are necessary, which are difficult to collect due to the heterogeneity of dystonia [106]. Matters are further complicated by the fact that target region choice and technical parameter settings are interdependent since different DBS targets appear to require other stimulation parameters. Thus, STN stimulation needs a significantly lower voltage and pulse width than GPi stimulation [10, 118], which seems to be due to the differences in nuclei volume [129]. Another aspect which makes it difficult to assess the effectiveness of DBS for dystonia is that improvement in tonic dystonic symptoms after pallidal stimulation may be delayed and take several days, weeks, or even months [10, 44, 63, 94, 124]. To bridge the lack of insufficient data from human patients with dystonia, translational research on animal models remains an essential approach for clarifying the pathophysiology of dystonia and providing insights into the mechanisms of DBS at the molecular and cellular levels. With this knowledge, we can develop effective treatment options for the different dystonia types. As mentioned below, pallidal theta oscillation is currently the most promising biomarker for individual-adapted DBS treatment of patients with cervical dystonia [79]. An abnormal activity pattern with excessive pallidal theta frequency oscillations can be used as a signal for turning on the DBS within the closed-loop system. However, most of the current DBS systems for chronic implantation in freely moving rodents are limited by the runtime or, especially for small rodents such as mice and hamsters, by volume restrictions [86], such that data on long-term stimulation remain rare. Concerning the variable clinical outcome of DBS, however, further studies are needed on the specific forms of dystonia in a search for significant biomarkers that allow for optimised and adapted DBS treatment. Such biomarker search studies cannot be performed on patients on a large scale and need to be flanked by experimental approaches. Thus, we need to uncover the pathophysiology of dystonia using animal models of dystonia [84].
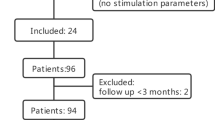
Electrophysiological data on DBS in dystonia models
During the last decades, the number of animal models for dystonia has risen due to the need to test hypotheses suggested by human studies, where it is often impossible to investigate the underlying physiologic, molecular, and cellular abnormalities. Rauschenberger et al. showed that results from animal studies are transferable to patients with dystonia, considering the movement-related oscillations as a robust parameter among the different species [88, 104]. The animal models for dystonia have been divided into etiologic and symptomatic (phenotypic) animal models. The etiologic model focuses on genetic predisposition and often lacking motor symptoms in the phenotype [92]. The symptomatic model represents clinical features consistent with human disorders and is suitable for identifying anatomical and physiological processes that elicit motor symptoms [126]. However, there are very few symptomatic animal models of dystonia. We refer to the reviews, which summarise current animal models for dystonia [54, 92, 126], and discuss the suitability of non-human primate and rodent dystonia models for DBS research [84].
There are few studies of DBS on symptomatic animal models of dystonia. The dtsz mutant hamster, a symptomatic model of paroxysmal dystonia, displays clinical symptoms of human dystonia patients in association with increased cortico-striatal excitability [7, 8, 59], and abnormal theta band oscillations [38]. Moreover, single-unit recordings indicated increased activity of the MSN and reduced activity of the EPN (entopeduncular nucleus, homologue of the human GPi), which likely leads to increased inhibition of the thalamus in the motor circuitry [11, 36]. Taking this model as a bona fide model of symptomatic dystonia, DBS was tested for its antidystonic efficacy, comparing STN-DBS (following the notion that STN can be an alternative target for DBS) and GPi-DBS in the dtsz mutant hamster [10, 118]. Only GPi-DBS, but not STN-DBS, significantly reduced the severity score of dystonia within 3 h of stimulation in awake animals with no difference in the stimulation parameters (pulse frequency: 130 Hz, pulse width: 60 μs, current amplitude: 50 μA) [81]. Further, to test whether lower frequencies of GPi-DBS are as effective as 130 Hz, Paap and colleagues analysed the severity scores at 40 Hz and 15 Hz DBS with all other stimulation parameters remaining constant. Reducing the stimulation frequency incidentally would consume less power in a stimulation system, allowing for longer intervals between charging [86]. The experiments revealed that, at least for the dtsz mutant hamster, 130 Hz is the most effective frequency for short-term DBS of 3 h. Taking the optimal GPi-DBS parameters as determined by Paap et al. (2021), we could show that the frequency of miniature excitatory postsynaptic currents (mEPSC) recorded in MSN of the dtsz mutant hamster is significantly reduced [49]. Thus, compared to healthy, wild-type tissue, dtsz mutant hamster neurons exhibited more mEPSC, which may reflect increased cortico-striatal excitability. In the same study, GPi-DBS was also conducted in normal, healthy, wild-type animals. In these, DBS had no significant effect on mEPSC, showing that the effect of DBS depends on the dysfunctional dystonic state of the network. Moreover, comparing mEPSC in healthy and dystonic tissues, DBS normalised mEPSC frequencies in dystonic tissue. Several explanations are possible for the reduced effect on MSN’s mEPSC: (1) DBS may retrogradely affect cortical or intrastriatal synaptic transmission via hyperdirect or direct pathway fibres. (2) Direct thalamic or indirect projections via the pallido-thalamo-cortical loop to the striatum are other plausible hypotheses [49]. (3) It is also conceivable that DBS affected the adenosine level, possibly by stimulating astrocytes [4], which influences excitatory cortico-striatal transmission [116, 117]. In summary, the reduced mEPSC frequency recorded in MSN after GPi-DBS in dtsz mutant hamster can be interpreted as an adaptive process of the entire basal-ganglia network responding to DBS (Fig. 3).
Effects of pallidal deep brain stimulation (DBS) in dystonia. Pallidal DBS is thought to be retrogradely and anterogradely relayed through reciprocal connections to several areas of the cortico-basal ganglia-thalamo-cortical loop (yellow arrows). Effects of pallidal DBS were already experimentally confirmed in dystonia animal models for the numbers 1–3: (1) Striatal medium spiny neurons showed reduced excitatory input provided through cortico-striatal and thalamo-striatal projections [49]. (2) DBS was also confirmed to reduce the pallidal theta power of the GPi [58]. (3) Inhibitory input to ventral motor thalamic nuclei (VA-VL-VM) neurons appears to be quantitatively unchanged. However, the excitatory input increased, which is thought to originate from afferents from the M1 (layers IV–VI) and the DCN. The hypothetical consequences of the increased excitatory input are summarised in the cartoon at site number (4): feedforward inhibition through inhibitory interneurons of layer I (which receive excitatory synaptic inputs from VM neurons) is strengthened. Inhibitory interneurons in layer I, in turn, dampen the activity of pyramidal neurons in layers II/III via their dendritic tufts, alleviating dystonic symptoms. Abbreviations: M1, primary motor cortex; STN, subthalamic nucleus; GPe/GPi, globus pallidus externus/internus; SNr/SNc, substantia nigra pars reticulata/compacta; VA, ventral anterior thalamic nucleus; VL, ventrolateral thalamic nucleus; VM, ventromedial thalamic nucleus; VA-VL-VM are part of the ventral motor thalamic nuclei (in red); CM-Pf, thalamic centre median/parafascicular complex; DCN, deep cerebellar nuclei (figure created with BioRender.com)
As an example of a genetic dystonia model, the ΔETorA rat model genetically mirrors the most common inherited DYT1 dystonia due to an overexpression of the mutated human TOR1A gene. It lacks, however, a plain dystonic phenotype [43]. Such a dystonic phenotype emerges in this model only after inducing a severe peripheral nerve trauma by e.g. crushing the sciatic nerve, which results in dystonia-like movements of the hindlimbs (crushed ΔETorA rat). Though it cannot be excluded that sensory deafferentation or dysfunction also plays a role in the development of these dystonic-like movements, the crushed ΔETorA rat is used as a humanised genetic TOR1A dystonia model. Like the dtsz mutant hamster, abnormal theta band oscillations can also be observed in the crushed ΔETorA rat [58]. Continuous GPi-DBS (pulse frequency: 130 Hz, pulse width: 200 μs, current amplitude individually adjusted to values 10 % below the occurrence of side effects) for 3 weeks significantly improved the dystonic-like movement severity score. Knorr et al. detected a slight reduction in theta power within the GPi that could be observed ~10 min after GPi-DBS was terminated [58].
The current findings are the beginning of understanding the efficacy of DBS on the network or, rather, on cellular mechanisms. However, previous experimental data are insufficient to elucidate the DBS mechanisms in dystonia. Most of the experimental data were determined with pallidal DBS. Data rarely exist for other stimulation targets in dystonia, such as STN or thalamus. In the following, we hypothesise the effects of pallidal DBS on the cortico-basal ganglia-thalamo-cortical loop in isolated dystonia, considering recent findings from animal experiments.
Hypotheses on the mechanisms of DBS on dystonia
The electrical stimulation of brain tissue is a complex matter mainly due to the anisotropy of the tissue surrounding the electrode and the heterogeneity of the stimulated cells and structures [44]. The therapeutic mechanisms of DBS remain still unclear. Due to the similarity in therapeutic outcomes reached with DBS and thalamotomy or pallidotomy, it has been debated that high-frequency stimulation inactivates the structures being stimulated. This notion was also supported by findings showing decreased firing activity of the stimulated nucleus [10, 29, 74]. Cell membranes located directly at the cathode are generally depolarised, while membranes proximal to the electrode are hyperpolarised. Based on chronaxie measurements, it was suggested that GPi- and thalamic DBS primarily stimulates the afferents and efferents fibres rather than dendrites or cell bodies [53]. DBS will not affect the somatodendritic membrane if the pulse width remains below the membrane time constant (> 1 ms) [52]. Hence, the axons’ activity can be considered decoupled from the soma within a minimal distance of the stimulation electrode [44]. As a general finding, DBS induces more than just a local effect close to the stimulation site. It should be considered to evoke systemic effects as it produces action potentials that propagate orthodromically and antidromically, thus affecting the overall pattern of activity in the network through interconnected nuclei [4, 44, 75]. DBS may not correct the specific abnormalities that may cause dystonia (see above) but rather lead to a compensatory effect of the entire network that counteracts the pathomechanisms. Here, the continuous stimulation with a constant frequency may lead to alterations in the spatial and temporal coding of the activity patterns, probably affecting long-term synaptic transmission and plasticity, reflected in the delayed effect of DBS treatment in dystonia.
The reduction in excitatory input to striatal MSN, as recently reported [49], may lead to decreased striatal activity (Fig. 3). This, in turn, can lead to reduced inhibition of the GPi, which in turn would suggest increased inhibition of the thalamus, specifically the ventral motor thalamic nuclei, consisting of the ventrolateral (VL), ventral anterior (VA), and ventromedial (VM) nucleus. However, our first data from patch clamp recordings within the ventral motor nuclei of the thalamus of the dtsz mutant hamster indicate that pallidal DBS does not affect the size of inhibitory postsynaptic currents [35]. Rather, there is a change in the inter-spike interval, which would be consistent with the reduced pallidal theta power in the study from the Ip group [58]. Alterations in the inter-spike interval would allow for synchronisation of the activity pattern with the stimulation frequency, rather than increasing the activity per se. In addition to changes in frequency of IPSC, EPSC in VL-VA-VM neurons in the DBS-treated group tended to be increased, again showing that DBS has network-wide effects [35]. Regarding the origin of the excitatory input to the ventral motor thalamic nuclei, the deep cortical layers (layer IV to layer VI) and the cerebellum are possible origins. What would be the effect of such increased excitation in thalamic neurons? Again, we can merely hypothesise that such increased excitatory input would strengthen feedforward inhibition through inhibitory interneurons of layer I, which receive excitatory synaptic inputs from VM neurons. The inhibitory interneurons in layer I inhibit pyramidal neurons in layers II/III over dendritic tufts [104], which could eventually alleviate dystonic symptoms. Alternatively, the increased excitatory input on the neurons of the ventral motor thalamic nuclei after long-term pallidal DBS may also result from strengthening the reciprocal positive feedback loop from the motor cortex (Fig. 3). On the whole, the impact of pallidal DBS can be retrogradely and anterogradely relayed through reciprocal and non-reciprocal connections to all areas of the cortico-basal ganglia-thalamo-cortical loop [45, 127] (Fig. 3).
Improvement of the dystonic symptoms can also be observed after thalamic DBS. In a study with a rat model of Parkinson’s disease, after 5-min electrical stimulation of the VA and VL, the number of induced action potentials in proximal neurons increased in vitro whole-cell patch clamp recordings [119]. VL neurons transitioned from bursting to non-bursting action potentials, while VA neurons were excited with little change in spiking phenotype. The authors speculated that thalamic DBS leads to increased excitation of the VA and VL neurons [119], which would be a similar effect as expected with pallidal DBS. The STN clinically is thought to be another promising stimulation target to improve dystonic symptoms [118]. However, at least experimentally, compared to GPi-DBS, short-term (3 h) STN-DBS did not alleviate dystonic symptoms in the dtsz mutant hamster [81]. This discrepancy may be due to differences in focal dystonia in patients with effective STN DBS vs. generalised dystonia in the hamster model, where STN-DBS is ineffective. In the cited publication, it was reasoned that STN-DBS is influencing SNr activity and, hence, GABAergic projections to the CM-Pf complex, more than GPi-DBS (Fig. 1). The somatotopic organisation of STN and CM-Pf was thus thought to allow for the stimulation of pathways for specific muscle groups, given the correct localisation of the stimulation electrodes. For generalised dystonia, such specific stimulation was speculated to be insufficient.
Overall, it seems certain that one cannot expect an alteration exclusively in a single projection within the cortico-basal ganglia-thalamo-cortical loop or one specific ion channel through DBS; rather DBS alters the entire network, likely resulting in an adaption of the activities of the specific nuclei within the movement loop to the electrical stimulation. Although DBS is thus causing a network effect, that obviously does not exclude effects on specific ion channel compositions and transmitter release resulting from altered neuronal activity and plasticity.
The choice of the ideal stimulation target, in turn, likely depends on the degree of abnormal network activity. Pallidal DBS seems more effective in generalised dystonia due to a more extensive effect within the entire cortico-basal ganglia-thalamo-cortical loop. In contrast, STN-DBS appears to be better suited for focal dystonia, where the cortico-basal ganglia-thalamo-cortical loop likely is associated with abnormal activities only in specific pathways. The next step in dystonia research is to identify the optimal parameters for balancing the alterations of DBS effects and pathomechanisms leading to standard physiological motor control.
Outlook
More knowledge on the pathophysiology of specific dystonia subtypes is necessary to find biomarkers for developing adaptive closed-looped DBS systems. With the help of translational research on animal models, we can overcome the lack of insufficient data from human patients with dystonia. We may obtain a detailed view of the pathophysiological and therapeutic (by DBS) mechanisms. Several in vivo, in vitro, and in silico methods help clarify the processes in the motor circuitry. Using microelectrode arrays (MEAs), simultaneous high-density recordings of the different nuclei in the cortico-basal ganglia-thalamo-cortical and cerebellar-thalamo-cortical network facilitate the investigation of network communication. Moreover, the MEA system enables defined local stimulation of specific parts in the network and the recording of spatio-temporal patterns in parallel that may be altered in dystonic tissue in our expectations. The MEA system also opens a new window for analysing synaptic plasticity (LTP and LTD) with a more significant number of recordings in parallel across a large area of the motor circuitry.
Translational research in animal models enables better access to tissue, which can be quantified for changes in cellular, molecular and transmitter levels affected by DBS. With the liquid chromatography-tandem mass spectrometry, e.g. microdialysates from different time points of the DBS were analysed to quantify the transmitter level [50]. Regional metabolic changes after DBS, already described for dystonia [80], are characterised by the positron emission tomography with the radiopharmaceutical glucose analogue (18)F-fluorodeoxyglucose. The investigation of specific local abnormalities, like the hypothesised striatal abnormal cholinergic tone, requires the individual pharmacological manipulation of these neurons for optogenetic experiments. In previous studies, the optogenetic activation of CSI [91] and striatopallidal MSN [98] in the DYT1 mouse model supports the detailed investigation of the already mentioned hypothesis of abnormal activity of CSI and imbalance between the direct and indirect pathway, respectively. The precise spatial and temporal selectivity of optogenetics that allows for stimulation of either afferent fibres or cell bodies makes it a powerful tool for studying the mechanisms of DBS [93].
For understanding and clarifying the complexity of the movement circuitry in detail, in silico modelling seems to be an additional option besides the experiments [103, 107]. The effects of variable DBS parameters can be modelled and tested in animal experiments in case of promising results.
Data availability
Not applicable.
References
Abudukeyoumu N, Hernandez-Flores T, Garcia-Munoz M, Arbuthnott GW (2019) Cholinergic modulation of striatal microcircuits. Eur J Neurosci 49:604–622. https://doi.org/10.1111/ejn.13949
Albanese A, Bhatia K, Bressman SB, DeLong MR, Fahn S, Fung VSC, Hallett M, Jankovic J, Jinnah HA, Klein C, Lang AE, Mink JW, Teller JK (2013) Phenomenology and classification of dystonia: a consensus update. Mov Disord 28:863–873. https://doi.org/10.1002/mds.25475
Asanuma K, Ma Y, Okulski J, Dhawan V, Chaly T, Carbon M, Bressman SB, Eidelberg D (2005) Decreased striatal D2 receptor binding in non-manifesting carriers of the DYT1 dystonia mutation. Neurol 64:347–349. https://doi.org/10.1212/01.WNL.0000149764.34953.BF
Ashkan K, Rogers P, Bergman H, Ughratdar I (2017) Insights into the mechanisms of deep brain stimulation. Nat Rev Neurol 13:548–554. https://doi.org/10.1038/nrneurol.2017.105
Assous M (2021) Striatal cholinergic transmission. focus on nicotinic receptors’ influence in striatal circuits. Eur J Neurosci 53(8):2421–2442. https://doi.org/10.1111/ejn.15135
Assous M, Tepper JM (2019) Excitatory extrinsic afferents to striatal interneurons and interactions with striatal microcircuitry. Eur J Neurosci 49:593–603. https://doi.org/10.1111/ejn.13881
Avchalumov Y, Sander SE, Richter F, Porath K, Hamann M, Bode C, Kirschstein T, Köhling R, Richter A (2014) Role of striatal NMDA receptor subunits in a model of paroxysmal dystonia. Exp Neurol 261:677–684. https://doi.org/10.1016/j.expneurol.2014.08.012
Avchalumov Y, Volkmann CE, Rückborn K, Hamann M, Kirschstein T, Richter A, Köhling R (2013) Persistent changes of corticostriatal plasticity in dtsz mutant hamsters after age-dependent remission of dystonia. Neurosci 250:60–69. https://doi.org/10.1016/j.neuroscience.2013.06.048
Balint B, Mencacci NE, Valente EM, Pisani A, Rothwell J, Jankovic J, Vidailhet M, Bhatia KP (2018) Dystonia. Nat Rev Dis Prim 4:25. https://doi.org/10.1038/s41572-018-0023-6
Benabid AL, Koudsie A, Benazzouz A, Vercueil L, Fraix V, Chabardes S, Lebas JF, Pollak P (2001) Deep brain stimulation of the corpus luysi (subthalamic nucleus) and other targets in Parkinson’s disease. Extension to new indications such as dystonia and epilepsy. J Neurol 248(Suppl):III37–III47. https://doi.org/10.1007/pl00007825
Bennay M, Gernert M, Richter A (2001) Spontaneous remission of paroxysmal dystonia coincides with normalization of entopeduncular activity in dt(SZ) mutants. J Neurosci 21:RC153
Bennett BD, Wilson CJ (1999) Spontaneous activity of neostriatal cholinergic interneurons in vitro. J Neurosci 19:5586–5596
Bode C, Richter F, Spröte C, Brigadski T, Bauer A, Fietz S, Fritschy J-M, Richter A (2017) Altered postnatal maturation of striatal GABAergic interneurons in a phenotypic animal model of dystonia. Exp Neurol 287:44–53. https://doi.org/10.1016/j.expneurol.2016.10.013
Bonsi P, Cuomo D, Martella G, Madeo G, Schirinzi T, Puglisi F, Ponterio G, Pisani A (2011) Centrality of striatal cholinergic transmission in basal ganglia function. Front Neuroanat 5:6. https://doi.org/10.3389/fnana.2011.00006
Bonsi P, Ponterio G, Vanni V, Tassone A, Sciamanna G, Migliarini S, Martella G, Meringolo M, Dehay B, Doudnikoff E, Zachariou V, Goodchild RE, Mercuri NB, D’Amelio M, Pasqualetti M, Bezard E, Pisani A (2019) RGS9-2 rescues dopamine D2 receptor levels and signaling in DYT1 dystonia mouse models. EMBO Mol Med 11:e9283. https://doi.org/10.15252/emmm.201809283
Brüggemann N, Kühn A, Schneider SA, Kamm C, Wolters A, Krause P, Moro E, Steigerwald F, Wittstock M, Tronnier V, Lozano AM, Hamani C, Poon Y-Y, Zittel S, Wächter T, Deuschl G, Krüger R, Kupsch A, Münchau A et al (2015) Short- and long-term outcome of chronic pallidal neurostimulation in monogenic isolated dystonia. Neurol 84:895–903. https://doi.org/10.1212/WNL.0000000000001312
Brunori G, Pelletier OB, Stauffer AM, Robishaw JD (2021) Selective manipulation of G-protein γ7 subunit in mice provides new insights into striatal control of motor behavior. J Neurosci 41:9065–9081. https://doi.org/10.1523/JNEUROSCI.1211-21.2021
Carbon M, Niethammer M, Peng S, Raymond D, Dhawan V, Chaly T, Ma Y, Bressman S, Eidelberg D (2009) Abnormal striatal and thalamic dopamine neurotransmission: genotype-related features of dystonia. Neurol 72:2097–2103. https://doi.org/10.1212/WNL.0b013e3181aa538f
Castela I, Casado-Polanco R, Rubio YV-W, da Silva JA, Marquez R, Pro B, Moratalla R, Redgrave P, Costa RM, Obeso J, Hernandez LF (2023) Selective activation of striatal indirect pathway suppresses levodopa induced-dyskinesias. Neurobiol Dis 176:105930. https://doi.org/10.1016/j.nbd.2022.105930
Chen W, de Hemptinne C, Miller AM, Leibbrand M, Little SJ, Lim DA, Larson PS, Starr PA (2020) Prefrontal-subthalamic hyperdirect pathway modulates movement inhibition in humans. Neuron 106:579–588.e3. https://doi.org/10.1016/j.neuron.2020.02.012
Cruz BF, Guiomar G, Soares S, Motiwala A, Machens CK, Paton JJ (2022) Action suppression reveals opponent parallel control via striatal circuits. Nature 607:521–526. https://doi.org/10.1038/s41586-022-04894-9
Cury RG, Kalia SK, Shah BB, Jimenez-Shahed J, Prashanth LK, Moro E (2018) Surgical treatment of dystonia. Expert Rev Neurother 18:477–492. https://doi.org/10.1080/14737175.2018.1478288
David HN, Ansseau M, Abraini JH (2005) Dopamine-glutamate reciprocal modulation of release and motor responses in the rat caudate-putamen and nucleus accumbens of “intact” animals. Brain Res Brain Res Rev 50:336–360. https://doi.org/10.1016/j.brainresrev.2005.09.002
Deffains M, Bergman H (2015) Striatal cholinergic interneurons and cortico-striatal synaptic plasticity in health and disease. Mov Disord 30:1014–1025. https://doi.org/10.1002/mds.26300
Detante O, Vercueil L, Thobois S, Broussolle E, Costes N, Lavenne F, Chabardes S, Lebars D, Vidailhet M, Benabid A-L, Pollak P (2004) Globus pallidus internus stimulation in primary generalized dystonia: a H215O PET study. Brain 127:1899–1908. https://doi.org/10.1093/brain/awh213
Ding J, Peterson JD, Surmeier DJ (2008) Corticostriatal and thalamostriatal synapses have distinctive properties. J Neurosci 28:6483–6492. https://doi.org/10.1523/JNEUROSCI.0435-08.2008
Ding JB, Guzman JN, Peterson JD, Goldberg JA, Surmeier DJ (2010) Thalamic gating of corticostriatal signaling by cholinergic interneurons. Neuron 67:294–307. https://doi.org/10.1016/j.neuron.2010.06.017
Dorst MC, Tokarska A, Zhou M, Lee K, Stagkourakis S, Broberger C, Masmanidis S, Silberberg G (2020) Polysynaptic inhibition between striatal cholinergic interneurons shapes their network activity patterns in a dopamine-dependent manner. Nat Commun 11:5113. https://doi.org/10.1038/s41467-020-18882-y
Dostrovsky JO, Lozano AM (2002) Mechanisms of deep brain stimulation. Mov Disord 17:S63–S68. https://doi.org/10.1002/mds.10143
Dressler D, Altenmüller E, Giess R, Krauss JK, Adib Saberi F (2022) The epidemiology of dystonia: the Hannover epidemiology study. J Neurol 269:6483–6493. https://doi.org/10.1007/s00415-022-11310-9
English DF, Ibanez-Sandoval O, Stark E, Tecuapetla F, Buzsáki G, Deisseroth K, Tepper JM, Koos T (2011) GABAergic circuits mediate the reinforcement-related signals of striatal cholinergic interneurons. Nat Neurosci 15:123–130. https://doi.org/10.1038/nn.2984
Eskow Jaunarajs KL, Bonsi P, Chesselet MF, Standaert DG, Pisani A (2015) Striatal cholinergic dysfunction as a unifying theme in the pathophysiology of dystonia. Prog Neurobiol 127:91–107. https://doi.org/10.1016/j.pneurobio.2015.02.002
Fan H, Zheng Z, Yin Z, Zhang J, Lu G (2021) Deep brain stimulation treating dystonia: a systematic review of targets, body distributions and etiology classifications. Front Hum Neurosci 15:757579. https://doi.org/10.3389/fnhum.2021.757579
Flagmeyer I, Haas HL, Stevens DR (1997) Adenosine A1 receptor-mediated depression of corticostriatal and thalamostriatal glutamatergic synaptic potentials in vitro. Brain Res 778:178–185. https://doi.org/10.1016/S0006-8993(97)01060-3
Franz D, Heerdegen M, Santana Kragelund F, Lüttig A, Perl S, Richter A, Köhling R (2023) P-68 Deep brain stimulation alters synaptic tone on ventroanterior-ventrolateral thalamic neurons in dystonic dtsz mutant hamsters. Clin Neurophysiol 148:e39–e40. https://doi.org/10.1016/j.clinph.2023.02.085
Gernert M, Bennay M, Fedrowitz M, Rehders JH, Richter A (2002) Altered discharge pattern of basal ganglia output neurons in an animal model of idiopathic dystonia. J Neurosci 22:7244–7253
Gernert M, Hamann M, Bennay M, Löscher W, Richter A (2000) Deficit of striatal parvalbumin-reactive GABAergic interneurons and decreased basal ganglia output in a genetic rodent model of idiopathic paroxysmal dystonia. J Neurosci 20:7052–7058
Gernert M, Richter A, Rundfeldt C, Löscher W (1998) Quantitative EEG analysis of depth electrode recordings from several brain regions of mutant hamsters with paroxysmal dystonia discloses frequency changes in the basal ganglia. Mov Disord 13:509–521. https://doi.org/10.1002/mds.870130322
Gittis AH, Nelson AB, Thwin MT, Palop JJ, Kreitzer AC (2010) Distinct roles of GABAergic interneurons in the regulation of striatal output pathways. J Neurosci 30:2223–2234. https://doi.org/10.1523/JNEUROSCI.4870-09.2010
Goldberg JA, Ding JB, Surmeier DJ (2012) Muscarinic modulation of striatal function and circuitry. In: Handbook of Experimental Pharmacology, pp 223–241. https://doi.org/10.1007/978-3-642-23274-9_10
Goldberg JA, Reynolds JNJ (2011) Spontaneous firing and evoked pauses in the tonically active cholinergic interneurons of the striatum. Neurosci 198:27–43. https://doi.org/10.1016/j.neuroscience.2011.08.067
Grill WM, Snyder AN, Miocinovic S (2004) Deep brain stimulation creates an informational lesion of the stimulated nucleus. Neuroreport 15:1137–1140. https://doi.org/10.1097/00001756-200405190-00011
Grundmann K, Glöckle N, Martella G, Sciamanna G, Hauser T-K, Yu L, Castaneda S, Pichler B, Fehrenbacher B, Schaller M, Nuscher B, Haass C, Hettich J, Yue Z, Nguyen HP, Pisani A, Riess O, Ott T (2012) Generation of a novel rodent model for DYT1 dystonia. Neurobiol Dis 47:61–74. https://doi.org/10.1016/j.nbd.2012.03.024
Gubellini P, Salin P, Kerkerian-Le Goff L, Baunez C (2009) Deep brain stimulation in neurological diseases and experimental models: from molecule to complex behavior. Prog Neurobiol 89:79–123. https://doi.org/10.1016/j.pneurobio.2009.06.003
Haber SN, Calzavara R (2009) The cortico-basal ganglia integrative network: the role of the thalamus. Brain Res Bull 78:69–74. https://doi.org/10.1016/j.brainresbull.2008.09.013
Hallett M (2011) Neurophysiology of dystonia: the role of inhibition. Neurobiol Dis 42:177–184. https://doi.org/10.1016/j.nbd.2010.08.025
Hamann M, Plank J, Richter F, Bode C, Smiljanic S, Creed M, Nobrega JN, Richter A (2017) Alterations of M1 and M4 acetylcholine receptors in the genetically dystonic (dt(sz)) hamster and moderate antidystonic efficacy of M1 and M4 anticholinergics. Neurosci 357:84–98. https://doi.org/10.1016/j.neuroscience.2017.05.051
Hamann M, Richter A (2004) Striatal increase of extracellular dopamine levels during dystonic episodes in a genetic model of paroxysmal dyskinesia. Neurobiol Dis 16:78–84. https://doi.org/10.1016/j.nbd.2004.01.005
Heerdegen M, Zwar M, Franz D, Hörnschemeyer J, Neubert V, Plocksties F, Niemann C, Timmermann D, Bahls C, van Rienen U, Paap M, Perl S, Lüttig A, Richter A, Köhling R (2021) Mechanisms of pallidal deep brain stimulation: alteration of cortico-striatal synaptic communication in a dystonia animal model. Neurobiol Dis 154:105341. https://doi.org/10.1016/j.nbd.2021.105341
Helmschrodt C, Becker S, Perl S, Schulz A, Richter A (2020) Development of a fast liquid chromatography-tandem mass spectrometry method for simultaneous quantification of neurotransmitters in murine microdialysate. Anal Bioanal Chem 412:7777–7787. https://doi.org/10.1007/s00216-020-02906-z
Hernández-Flores T, Hernández-González O, Pérez-Ramírez MB, Lara-González E, Arias-García MA, Duhne M, Pérez-Burgos A, Prieto GA, Figueroa A, Galarraga E, Bargas J (2015) Modulation of direct pathway striatal projection neurons by muscarinic M4-type receptors. Neuropharmacol 89:232–244. https://doi.org/10.1016/j.neuropharm.2014.09.028
Holsheimer J, Demeulemeester H, Nuttin B, De Sutter P (2000) Identification of the target neuronal elements in electrical deep brain stimulation. Eur J Neurosci 12:4573–4577. https://doi.org/10.1046/j.1460-9568.2000.01306.x
Holsheimer J, Dijkstra EA, Demeulemeester H, Nuttin B (2000) Chronaxie calculated from current-duration and voltage-duration data. J Neurosci Methods 97:45–50. https://doi.org/10.1016/s0165-0270(00)00163-1
Imbriani P, Ponterio G, Tassone A, Sciamanna G, El Atiallah I, Bonsi P, Pisani A (2020) Models of dystonia: an update. J Neurosci Methods 339:108728. https://doi.org/10.1016/j.jneumeth.2020.108728
Isaias IU, Alterman RL, Tagliati M (2008) Outcome predictors of pallidal stimulation in patients with primary dystonia: the role of disease duration. Brain 131:1895–1902. https://doi.org/10.1093/brain/awn120
Jinnah HA, Neychev V, Hess EJ (2017) The anatomical basis for dystonia: the motor network model. Tremor Other Hyperkinet Mov (N Y) 7:506. https://doi.org/10.7916/D8V69X3S
Klein C (2014) Genetics in dystonia. Parkinsonism Relat Disord 20(Suppl 1):S137–S142. https://doi.org/10.1016/S1353-8020(13)70033-6
Knorr S, Rauschenberger L, Pasos UR, Friedrich MU, Peach RL, Grundmann-Hauser K, Ott T, O’Leary A, Reif A, Tovote P, Volkmann J, Ip CW (2021) The evolution of dystonia-like movements in TOR1A rats after transient nerve injury is accompanied by dopaminergic dysregulation and abnormal oscillatory activity of a central motor network. Neurobiol Dis 154:105337. https://doi.org/10.1016/j.nbd.2021.105337
Köhling R, Koch U-R, Hamann M, Richter A (2004) Increased excitability in cortico-striatal synaptic pathway in a model of paroxysmal dystonia. Neurobiol Dis 16:236–245. https://doi.org/10.1016/j.nbd.2004.01.012
Krack P, Martinez-Fernandez R, Del Alamo M, Obeso JA (2017) Current applications and limitations of surgical treatments for movement disorders. Mov Disord 32:36–52. https://doi.org/10.1002/mds.26890
Krack P, Vercueil L (2001) Review of the functional surgical treatment of dystonia. Eur J Neurol 8:389–399. https://doi.org/10.1046/j.1468-1331.2001.00231.x
Krauss JK, Lipsman N, Aziz T, Boutet A, Brown P, Chang JW, Davidson B, Grill WM, Hariz MI, Horn A, Schulder M, Mammis A, Tass PA, Volkmann J, Lozano AM (2021) Technology of deep brain stimulation: current status and future directions. Nat Rev Neurol 17:75–87. https://doi.org/10.1038/s41582-020-00426-z
Krauss JK, Yianni J, Loher TJ, Aziz TZ (2004) Deep brain stimulation for dystonia. J Clin Neurophysiol 21:18–30. https://doi.org/10.1097/00004691-200401000-00004
Lacey CJ, Bolam JP, Magill PJ (2007) Novel and distinct operational principles of intralaminar thalamic neurons and their striatal projections. J Neurosci 27:4374–4384. https://doi.org/10.1523/JNEUROSCI.5519-06.2007
Lange F, Roothans J, Wichmann T, Gelbrich G, Röser C, Volkmann J, Reich M (2021) DIPS (Dystonia Image-based Programming of Stimulation: a prospective, randomized, double-blind crossover trial). Neurol Res Pract 3:65. https://doi.org/10.1186/s42466-021-00165-6
Lehéricy S, Tijssen MAJ, Vidailhet M, Kaji R, Meunier S (2013) The anatomical basis of dystonia: current view using neuroimaging. Mov Disord 28:944–957. https://doi.org/10.1002/mds.25527
Lempka SF, Johnson MD, Miocinovic S, Vitek JL, McIntyre CC (2010) Current-controlled deep brain stimulation reduces in vivo voltage fluctuations observed during voltage-controlled stimulation. Clin Neurophysiol 121:2128–2133. https://doi.org/10.1016/j.clinph.2010.04.026
Lempka SF, Miocinovic S, Johnson MD, Vitek JL, McIntyre CC (2009) In vivo impedance spectroscopy of deep brain stimulation electrodes. J Neural Eng 6:046001. https://doi.org/10.1088/1741-2560/6/4/046001
Lerner TN, Kreitzer AC (2011) Neuromodulatory control of striatal plasticity and behavior. Curr Opin Neurobiol 21:322–327. https://doi.org/10.1016/j.conb.2011.01.005
Lofredi R, Kühn AA (2022) Brain oscillatory dysfunctions in dystonia. Handb Clin Neurol 184:249–257. https://doi.org/10.1016/B978-0-12-819410-2.00026-6
Lozano AM, Lipsman N, Bergman H, Brown P, Chabardes S, Chang JW, Matthews K, McIntyre CC, Schlaepfer TE, Schulder M, Temel Y, Volkmann J, Krauss JK (2019) Deep brain stimulation: current challenges and future directions. Nat Rev Neurol 15:148–160. https://doi.org/10.1038/s41582-018-0128-2
Martella G, Tassone A, Sciamanna G, Platania P, Cuomo D, Viscomi MT, Bonsi P, Cacci E, Biagioni S, Usiello A, Bernardi G, Sharma N, Standaert DG, Pisani A (2009) Impairment of bidirectional synaptic plasticity in the striatum of a mouse model of DYT1 dystonia: role of endogenous acetylcholine. Brain 132:2336–2349. https://doi.org/10.1093/brain/awp194
Mazere J, Dilharreguy B, Catheline G, Vidailhet M, Deffains M, Vimont D, Ribot B, Barse E, Cif L, Mazoyer B, Langbour N, Pisani A, Allard M, Lamare F, Guehl D, Fernandez P, Burbaud P (2021) Striatal and cerebellar vesicular acetylcholine transporter expression is disrupted in human DYT1 dystonia. Brain 144:909–923. https://doi.org/10.1093/brain/awaa465
McIntyre CC, Grill WM, Sherman DL, Thakor NV (2004) Cellular effects of deep brain stimulation: model-based analysis of activation and inhibition. J Neurophysiol 91:1457–1469. https://doi.org/10.1152/jn.00989.2003
McIntyre CC, Hahn PJ (2010) Network perspectives on the mechanisms of deep brain stimulation. Neurobiol Dis 38:329–337. https://doi.org/10.1016/j.nbd.2009.09.022
Moss J, Bolam JP (2008) A dopaminergic axon lattice in the striatum and its relationship with cortical and thalamic terminals. J Neurosci 28:11221–11230. https://doi.org/10.1523/JNEUROSCI.2780-08.2008
Mundinger F (1977) Neue stereotaktisch-funktionelle Behandlungsmethode des Torticollis spasmodicus mit Hirnstimulatoren. Med Klin 72(46):1982–1986
Nair AG, Castro LRV, El Khoury M, Gorgievski V, Giros B, Tzavara ET, Hellgren-Kotaleski J, Vincent P (2019) The high efficacy of muscarinic M4 receptor in D1 medium spiny neurons reverses striatal hyperdopaminergia. Neuropharmacol 146:74–83. https://doi.org/10.1016/j.neuropharm.2018.11.029
Neumann W-J, Horn A, Ewert S, Huebl J, Brücke C, Slentz C, Schneider G-H, Kühn AA (2017) A localized pallidal physiomarker in cervical dystonia. Ann Neurol 82:912–924. https://doi.org/10.1002/ana.25095
Nobrega JN, Richter A, Tozman N, Jiwa D, Löscher W (1996) Quantitative autoradiography reveals regionally selective changes in dopamine D1 and D2 receptor binding in the genetically dystonic hamster. Neurosci 71:927–937. https://doi.org/10.1016/0306-4522(95)00511-0
Paap M, Perl S, Lüttig A, Plocksties F, Niemann C, Timmermann D, Bahls C, van Rienen U, Franz D, Zwar M, Rohde M, Köhling R, Richter A (2020) Deep brain stimulation by optimized stimulators in a phenotypic model of dystonia: effects of different frequencies. Neurobiol Dis 147:105163. https://doi.org/10.1016/j.nbd.2020.105163
Pauls KAM, Bröckelmann PJ, Hammesfahr S, Becker J, Hellerbach A, Visser-Vandewalle V, Dembek TA, Meister IG, Timmermann L (2018) Dysarthria in pallidal deep brain stimulation in dystonia depends on the posterior location of active electrode contacts: a pilot study. Parkinsonism Relat Disord 47:71–75. https://doi.org/10.1016/j.parkreldis.2017.11.002
Pelosi A, Menardy F, Popa D, Girault J-A, Hervé D (2017) Heterozygous Gnal mice are a novel animal model with which to study dystonia pathophysiology. J Neurosci 37:6253–6267. https://doi.org/10.1523/JNEUROSCI.1529-16.2017
Perl S, Lüttig A, Köhling R, Richter A (2022) Deep brain stimulation in animal models of dystonia. Neurobiol Dis 175:105912. https://doi.org/10.1016/j.nbd.2022.105912
Pisani A, Bernardi G, Ding J, Surmeier DJ (2007) Re-emergence of striatal cholinergic interneurons in movement disorders. Trends Neurosci 30:545–553. https://doi.org/10.1016/j.tins.2007.07.008
Plocksties F, Kober M, Niemann C, Heller J, Fauser M, Nüssel M, Uster F, Franz D, Zwar M, Lüttig A, Kröger J, Harloff J, Schulz A, Richter A, Köhling R, Timmermann D, Storch A (2021) The software defined implantable modular platform (STELLA) for preclinical deep brain stimulation research in rodents. J Neural Eng 18:056032. https://doi.org/10.1088/1741-2552/ac23e1
Quartarone A, Hallett M (2013) Emerging concepts in the physiological basis of dystonia. Mov Disord 28:958–967. https://doi.org/10.1002/mds.25532
Rauschenberger L, Güttler C, Volkmann J, Kühn AA, Ip CW, Lofredi R (2022) A translational perspective on pathophysiological changes of oscillatory activity in dystonia and parkinsonism. Exp Neurol 355:114140. https://doi.org/10.1016/j.expneurol.2022.114140
Reynolds JNJ, Avvisati R, Dodson PD, Fisher SD, Oswald MJ, Wickens JR, Zhang Y-F (2022) Coincidence of cholinergic pauses, dopaminergic activation and depolarisation of spiny projection neurons drives synaptic plasticity in the striatum. Nat Commun 13:1296. https://doi.org/10.1038/s41467-022-28950-0
Richter A, Hamann M (2001) Effects of adenosine receptor agonists and antagonists in a genetic animal model of primary paroxysmal dystonia. Br J Pharmacol 134:343–352. https://doi.org/10.1038/sj.bjp.0704268
Richter F, Bauer A, Perl S, Schulz A, Richter A (2019) Optogenetic augmentation of the hypercholinergic endophenotype in DYT1 knock-in mice induced erratic hyperactive movements but not dystonia. EBioMedicine 41:649–658. https://doi.org/10.1016/j.ebiom.2019.02.042
Richter F, Richter A (2014) Genetic animal models of dystonia: common features and diversities. Prog Neurobiol 121:91–113. https://doi.org/10.1016/j.pneurobio.2014.07.002
Rossi MA, Calakos N, Yin HH (2015) Spotlight on movement disorders: what optogenetics has to offer. Mov Disord 30:624–631. https://doi.org/10.1002/mds.26184
Scheller U, Lofredi R, van Wijk BCM, Saryyeva A, Krauss JK, Schneider G-H, Kroneberg D, Krause P, Neumann W-J, Kühn AA (2019) Pallidal low-frequency activity in dystonia after cessation of long-term deep brain stimulation. Mov Disord 34:1734–1739. https://doi.org/10.1002/mds.27838
Schirinzi T, Sciamanna G, Mercuri NB, Pisani A (2018) Dystonia as a network disorder: a concept in evolution. Curr Opin Neurol 31:498–503. https://doi.org/10.1097/WCO.0000000000000580
Schulz JM, Reynolds JNJ (2013) Pause and rebound: sensory control of cholinergic signaling in the striatum. Trends Neurosci 36:41–50. https://doi.org/10.1016/j.tins.2012.09.006
Schuurman PR, Bosch DA, Bossuyt PM, Bonsel GJ, van Someren EJ, de Bie RM, Merkus MP, Speelman JD (2000) A comparison of continuous thalamic stimulation and thalamotomy for suppression of severe tremor. N Engl J Med 342:461–468. https://doi.org/10.1056/NEJM200002173420703
Sciamanna G, Ponterio G, Vanni V, Laricchiuta D, Martella G, Bonsi P, Meringolo M, Tassone A, Mercuri NB, Pisani A (2020) Optogenetic activation of striatopallidal neurons reveals altered HCN gating in DYT1 dystonia. Cell Rep 31:107644. https://doi.org/10.1016/j.celrep.2020.107644
Sciamanna G, Tassone A, Mandolesi G, Puglisi F, Ponterio G, Martella G, Madeo G, Bernardi G, Standaert DG, Bonsi P, Pisani A (2012) Cholinergic dysfunction alters synaptic integration between thalamostriatal and corticostriatal inputs in DYT1 dystonia. J Neurosci 32:11991–12004. https://doi.org/10.1523/JNEUROSCI.0041-12.2012
Sciamanna G, Tassone A, Martella G, Mandolesi G, Puglisi F, Cuomo D, Madeo G, Ponterio G, Standaert DG, Bonsi P, Pisani A (2011) Developmental profile of the aberrant dopamine D2 receptor response in striatal cholinergic interneurons in DYT1 dystonia. PLoS One 6:e24261. https://doi.org/10.1371/journal.pone.0024261
Shen W, Plotkin JL, Francardo V, Ko WKD, Xie Z, Li Q, Fieblinger T, Wess J, Neubig RR, Lindsley CW, Conn PJ, Greengard P, Bezard E, Cenci MA, Surmeier DJ (2015) M4 muscarinic receptor signaling ameliorates striatal plasticity deficits in models of L-DOPA-induced dyskinesia. Neuron 88:762–773. https://doi.org/10.1016/j.neuron.2015.10.039
Shen W, Tian X, Day M, Ulrich S, Tkatch T, Nathanson NM, Surmeier DJ (2007) Cholinergic modulation of Kir2 channels selectively elevates dendritic excitability in striatopallidal neurons. Nat Neurosci 10:1458–1466. https://doi.org/10.1038/nn1972
Siettos C, Starke J (2016) Multiscale modeling of brain dynamics: from single neurons and networks to mathematical tools. Wiley Interdiscip Rev Syst Biol Med 8:438–458. https://doi.org/10.1002/wsbm.1348
Sieveritz B, García-Muñoz M, Arbuthnott GW (2019) Thalamic afferents to prefrontal cortices from ventral motor nuclei in decision-making. Eur J Neurosci 49:646–657. https://doi.org/10.1111/ejn.14215
Silberstein P, Kühn AA, Kupsch A, Trottenberg T, Krauss JK, Wöhrle JC, Mazzone P, Insola A, Di Lazzaro V, Oliviero A, Aziz T, Brown P (2003) Patterning of globus pallidus local field potentials differs between Parkinson’s disease and dystonia. Brain 126:2597–2608. https://doi.org/10.1093/brain/awg267
Smit M, Albanese A, Benson M, Edwards MJ, Graessner H, Hutchinson M, Jech R, Krauss JK, Morgante F, Pérez Dueñas B, Reilly RB, Tinazzi M, Contarino MF, MAJ T, Collaborative Working Group (2021) Dystonia management: what to expect from the future? The perspectives of patients and clinicians within DystoniaNet Europe. Front Neurol 12:646841. https://doi.org/10.3389/fneur.2021.646841
Spiliotis K, Starke J, Franz D, Richter A, Köhling R (2022) Deep brain stimulation for movement disorder treatment: exploring frequency-dependent efficacy in a computational network model. Biol Cybern 116:93–116. https://doi.org/10.1007/s00422-021-00909-2
Straub C, Tritsch NX, Hagan NA, Gu C, Sabatini BL (2014) Multiphasic modulation of cholinergic interneurons by nigrostriatal afferents. J Neurosci 34:8557–8569. https://doi.org/10.1523/JNEUROSCI.0589-14.2014
Surmeier DJ, Ding J, Day M, Wang Z, Shen W (2007) D1 and D2 dopamine-receptor modulation of striatal glutamatergic signaling in striatal medium spiny neurons. Trends Neurosci 30:228–235. https://doi.org/10.1016/j.tins.2007.03.008
Surmeier DJ, Shen W, Day M, Gertler T, Chan S, Tian X, Plotkin JL (2010) The role of dopamine in modulating the structure and function of striatal circuits. Prog Brain Res 183:149–167. https://doi.org/10.1016/S0079-6123(10)83008-0
Tepper JM, Koós T, Ibanez-Sandoval O, Tecuapetla F, Faust TW, Assous M (2018) Heterogeneity and diversity of striatal GABAergic interneurons: update 2018. Front Neuroanat 12:91. https://doi.org/10.3389/fnana.2018.00091
Thenganatt MA, Jankovic J (2014) Treatment of dystonia. Neurotherapeutics 11:139–152. https://doi.org/10.1007/s13311-013-0231-4
Threlfell S, Lalic T, Platt NJ, Jennings KA, Deisseroth K, Cragg SJ (2012) Striatal dopamine release is triggered by synchronized activity in cholinergic interneurons. Neuron 75:58–64. https://doi.org/10.1016/j.neuron.2012.04.038
Tisch S, Rothwell JC, Bhatia KP, Quinn N, Zrinzo L, Jahanshahi M, Ashkan K, Hariz M, Limousin P (2007) Pallidal stimulation modifies after-effects of paired associative stimulation on motor cortex excitability in primary generalised dystonia. Exp Neurol 206:80–85. https://doi.org/10.1016/j.expneurol.2007.03.027
Tisch S, Rothwell JC, Limousin P, Hariz MI, Corcos DM (2007) The physiological effects of pallidal deep brain stimulation in dystonia. IEEE Trans Neural Syst Rehabil Eng 15:166–172. https://doi.org/10.1109/TNSRE.2007.896994
Tozzi A, de Iure A, Di Filippo M, Tantucci M, Costa C, Borsini F, Ghiglieri V, Giampà C, Fusco FR, Picconi B, Calabresi P (2011) The distinct role of medium spiny neurons and cholinergic interneurons in the D2/A2A receptor interaction in the striatum: implications for Parkinson’s disease. J Neurosci 31:1850–1862. https://doi.org/10.1523/JNEUROSCI.4082-10.2011
Tozzi A, Tscherter A, Belcastro V, Tantucci M, Costa C, Picconi B, Centonze D, Calabresi P, Borsini F (2007) Interaction of A2A adenosine and D2 dopamine receptors modulates corticostriatal glutamatergic transmission. Neuropharmacol 53:783–789. https://doi.org/10.1016/j.neuropharm.2007.08.006
Tsuboi T, Wong JK, Almeida L, Hess CW, Wagle Shukla A, Foote KD, Okun MS, Ramirez-Zamora A (2020) A pooled meta-analysis of GPi and STN deep brain stimulation outcomes for cervical dystonia. J Neurol 267:1278–1290. https://doi.org/10.1007/s00415-020-09703-9
Tucker HR, Mahoney E, Chhetri A, Unger K, Mamone G, Kim G, Audil A, Moolick B, Molho ES, Pilitsis JG, Shin DS (2019) Deep brain stimulation of the ventroanterior and ventrolateral thalamus improves motor function in a rat model of Parkinson’s disease. Exp Neurol 317:155–167. https://doi.org/10.1016/j.expneurol.2019.03.008
Vercueil L, Pollak P, Fraix V, Caputo E, Moro E, Benazzouz A, Xie J, Koudsie A, Benabid AL (2001) Deep brain stimulation in the treatment of severe dystonia. J Neurol 248:695–700. https://doi.org/10.1007/s004150170116
Vidailhet M, Jutras M-F, Grabli D, Roze E (2013) Deep brain stimulation for dystonia. J Neurol Neurosurg Psychiatry 84:1029–1042. https://doi.org/10.1136/jnnp-2011-301714
Vidailhet M, Vercueil L, Houeto J-L, Krystkowiak P, Lagrange C, Yelnik J, Bardinet E, Benabid A-L, Navarro S, Dormont D, Grand S, Blond S, Ardouin C, Pillon B, Dujardin K, Hahn-Barma V, Agid Y, Destée A, Pollak P, French SPIDY Study Group (2007) Bilateral, pallidal, deep-brain stimulation in primary generalised dystonia: a prospective 3 year follow-up study. Lancet Neurol 6:223–229. https://doi.org/10.1016/S1474-4422(07)70035-2
Volkmann J, Wolters A, Kupsch A, Müller J, Kühn AA, Schneider G-H, Poewe W, Hering S, Eisner W, Müller J-U, Deuschl G, Pinsker MO, Skogseid I-M, Roeste GK, Krause M, Tronnier V, Schnitzler A, Voges J, Nikkhah G et al (2012) Pallidal deep brain stimulation in patients with primary generalised or segmental dystonia: 5-year follow-up of a randomised trial. Lancet Neurol 11:1029–1038. https://doi.org/10.1016/S1474-4422(12)70257-0
Wichmann T, DeLong MR (2016) Deep brain stimulation for movement disorders of basal ganglia origin: restoring function or functionality? Neurotherapeutics 13:264–283. https://doi.org/10.1007/s13311-016-0426-6
Wichmann T, Dostrovsky JO (2011) Pathological basal ganglia activity in movement disorders. Neurosci 198:232–244. https://doi.org/10.1016/j.neuroscience.2011.06.048
Wilson BK, Hess EJ (2013) Animal models for dystonia. Mov Disord 28:982–989. https://doi.org/10.1002/mds.25526
Wree A, Schmitt O (2015) Basal ganglia. Brain Mapp An Encycl Ref 2:217–227. https://doi.org/10.1016/B978-0-12-397025-1.00215-3
Zauber SE, Watson N, Comella CL, Bakay RAE, Metman LV (2009) Stimulation-induced parkinsonism after posteroventral deep brain stimulation of the globus pallidus internus for craniocervical dystonia. J Neurosurg 110:229–233. https://doi.org/10.3171/2008.6.17621
Zhang J, Zhang K, Wang Z, Ge M, Ma Y (2006) Deep brain stimulation in the treatment of secondary dystonia. Chin Med J 119:2069–2074
Funding
Open Access funding enabled and organized by Projekt DEAL. Our work is funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) – SFB 1270/1,2 – 299150580.
Author information
Authors and Affiliations
Contributions
Denise Franz performed the literature search and drafted the work. Angelika Richter critically revised the work. Rüdiger Köhling had the idea for the article and its layout and critically revised the text.
Corresponding author
Ethics declarations
Ethics approval
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Franz, D., Richter, A. & Köhling, R. Electrophysiological insights into deep brain stimulation of the network disorder dystonia. Pflugers Arch - Eur J Physiol 475, 1133–1147 (2023). https://doi.org/10.1007/s00424-023-02845-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-023-02845-5