Abstract
Introduction
Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) are the two most performed techniques in bariatric surgery. The aim of this study is to compare two surgical procedures in terms of weight loss and the development of comorbidities such as type II diabetes mellitus T2D, arterial hypertension, sleep apnea (OSAS), and gastroesophageal reflux disease (GERD).
Methods
Data from the German Bariatric Surgery Registry (GBSR) from 2005 to 2021 were used. 1,392 RYGB and 1,132 SG primary surgery patients were included. Minimum age 18 years; five-year follow-up data available. Tests were performed with a 5% significance level.
Results
Loss of follow-up 95.41% within five years. Five years after surgery, the RYGB showed significant advantages in terms of excess weight loss (%EWL 64.2% vs. 56.9%) and remission rates of the studied comorbidities: hypertension (54.4% vs. 47.8%), OSAS (64.5% vs. 50.1%), and GERD (86.1% vs. 66.9%). Compared to the pre-test, individuals diagnosed with insulin-dependent T2D showed significant improvements with RYGB over a five-year period (remission rate: 75% vs. 63%). In contrast, non-insulin-dependent T2D showed no significant difference between the two approaches (p = 0.125).
Conclusion
Both surgical procedures resulted in significant weight loss and improved comorbidities. However, the improvement in comorbidities was significantly greater in patients who underwent RYGB than in those who underwent SG, suggesting that the RYGB technique is preferable.
Nevertheless, RYGB requires a high degree of surgical skill. Therefore, acquiring expertise in the technical facets of the surgery is essential to achieving favorable outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe obesity is associated with a variety of chronic conditions that compromise overall health and increase the risk of death in obese individuals [1, 2]. An increase in BMI significantly increases the likelihood of developing obesity-related conditions such as arterial hypertension aHTN, diabetes mellitus type 2 (T2D), and apnea (OSAS) [3, 4]. Most non-surgical treatments have shown limited effectiveness in reducing weight and managing obesity-related comorbidities [5]. Clinical studies have consistently shown that bariatric surgery is an effective method for weight loss and management of obesity-related comorbidities [6]. Bariatric surgery is a growing surgical field focused on the treatment of obesity due to the rapid increase in weight worldwide [7].
Surgical techniques have historically been classified as malabsorptive, restrictive, or mixed. However, the efficacy of different bariatric surgical approaches in terms of weight loss, comorbidity reduction, and perioperative outcomes varies widely. Sleeve gastrectomy (SG) and Roux-Y gastric bypass (RYGB) have long been recognized as standard bariatric surgical procedures [8].
RYGB and SG each have their own advantages and disadvantages. SG has experienced a rapid rise as a bariatric surgical procedure for patients with obesity due to its technical simplicity [9]. However, when it comes to treating obesity-related conditions, bariatric surgery has shown more favorable results when using techniques like RYGB as opposed to SG [10].
The objectives of this study are to compare the efficacy of SG and RYGB in achieving remission of obesity-related comorbidities, to identify any perioperative complications that may be associated with both procedures, and to provide an update on weight status five years after surgery. By comparing the results of our study with those of international randomized trials, we hope to provide an overview of the current status and outcomes of both procedures in Germany and draw comparisons between the outcomes in Germany and those of international randomized trials.
Material and methods
Data collection and study design
The study was conducted in accordance with the principles specified in the Declaration of Helsinki, which governs biomedical research. All participants completed an informed consent form before data were entered into the registry. Patients were included in the study if they consented to follow-up.
Data were collected online for the purpose of quality assurance research. The research involved entering the relevant data into a specially designed database. StatConsult performed the data analysis using export data from 04/2021, which were reviewed, and plausibility checked by the study director.
The current retrospective multicenter analysis of the German Bariatric Surgery Registry (GBSR) database, which was compiled prospectively between January 2005 and April 2021, used the following inclusion criteria (Fig. 1):
-
Minimum age 18 years.
-
RYGB or SG is acceptable as the primary surgical procedure.
-
A valid five-year follow-up (1,643–2,008 days after surgery) is required.
Selection of the appropriate surgical procedure was influenced by individual patient characteristics and physician indications. Data collected included:
-
Population statistics, weight data, comorbidities, and ASA classification.
-
Long-term follow-up data, including weight development, BMI reduction, %EWL, development of T2D, aHTN, OSAS, and GERD.
-
Patients were considered to be completely cured of reflux at follow-up examinations if the symptoms and medication treatment of reflux were no longer present after surgery. Some clinics added pH monitoring and endoscopy; however, this was not a universal practice and not a standard procedure to rule out reflux disease after bariatric surgery.
-
The development of DM, aHTN, and OSAS was compared with the original preoperative data based on medication and symptom development after surgery. Different categories were analyzed for all comorbidities compared: Worsening, improvement, new development, no change or complete remission of comorbidities.
Statistical analysis
Statistical analyses were performed using SAS 9.4 at a 5% significance level, with a p-value of less than or equal to 0.05 indicating a statistically significant difference.
Descriptive and univariate/unadjusted analyses:
Analysis included examination of mean, standard deviation, and number of patients for quasi-continuous variables and root-transformed data. The mean values of the original and transformed data differ. Continuous variables are reported as minimum, lower quartile, median, upper quartile, and maximum and a paired t-test is used for comparison.
Unadjusted analyses are used to analyze the effect of a single variable on a target parameter, with a focus on comparing surgical procedures. The chi-squared test is used for categorical outcome variables, and the Satterthwaite robust t-test is used for continuous outcome variables. Significant deviations from the normal distribution require a root function transformation to approximate the distribution.
Results
The study included a total of 73,445 patients. Of these, 54,984 patients underwent either RYGB or SG. Of the 2,524 patients who were followed up for five years, 55.2% (n = 1,392) underwent RYGB, whereas 44.8% (n = 1,132) underwent SG. The majority of both procedures were performed using laparoscopic techniques (> 97%), and SG had a significantly shorter operating time. Postoperative and total hospital stay did not show a significant advantage for either group.
The study found a significant gender distribution among the 2,524 patients, with a higher proportion of females (75.2%) than males (24.8%). Among the SG group, 357 (31.5%) patients were male and 775 (68.5%) were female. In the RYGB cohort, 19.3% were male and 80.7% were female (p < 0.001).
Of the total of 2,339 patients, 92.7% had a documented comorbidity at the time of surgery (Fig. 2). According to the study, there was considerable variation in patients’ comorbidities. Cardiovascular disease and degenerative skeletal disease were more common in SG patients, whereas smoking, varicosis, T2D, insulin-dependent diabetes mellitus (IDDM), GERD, and non-alcoholic steatohepatitis (NASH) were more common in RYGB patients (p < 5% overall). Table 1 and Fig. 2 provide a brief summary of the comorbidities identified preoperatively and assessed during the follow-up period.
Distribution of comorbidities at the time of surgery. OCVD = other cardiovascular disease, DSD = degenerative skeletal disease, DSPD = degenerative spinal disease, NASH = nonalcoholic steatohepatitis, RID = rheumatoid inflammatory disease, PCOS = polycystic ovary syndrome, CID = chronic inflammatory bowel disease.
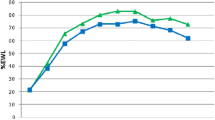
The analysis showed no significant difference in age distribution between the SG and RYGB groups. Patients treated with SG had a higher level of morbidity and a higher body mass index (BMI). During the first five years after surgery, the mean BMI decreased from 50.4 kg/m2 to 36.1 kg/m2 (SG) and from 47.9 kg/m2 to 33.6 kg/m2 (RYGB) with no statistically significant difference between the two groups. However, RYGB resulted in a significantly higher %EWL (p < 0.001) (Tables 1 and 2).
Five years after surgery, both SG and RYGB showed improvements in the recorded comorbidities with complete and partial remissions. Table 3 shows a summary of the change in comorbidities in each group.
When examining the progression of comorbidities from the time of surgery to five years postoperatively, RYGB showed a significant advantage in aHTN, OSAS, and GERD (Table 3). In addition, RYGB showed a significant advantage in IDDM when comparing the situation five years after surgery with the most recent examination (Table 4).
Regarding postoperative de-novo of comorbidities, IDDM, NIDDM, aHTN, and OSAS did not differ between the two surgical procedures. However, there was a significant difference in de-novo postoperative GERD, which was almost three times more frequent after SG, but also occurred in 10% after RYGB (Table 4).
Discussion
Bariatric and metabolic surgery has been empirically shown to be more effective in achieving weight loss than non-surgical approaches [18, 19]. Patients who underwent bariatric surgery experienced a significant weight loss, with a mean reduction of 26 kg, according to a meta-analysis [20]. This finding contrasts with the results of non-surgical treatments. However, a comprehensive risk assessment is essential, especially for elderly and critically ill patients [21].
The present analysis analyzes patients who were enrolled in the registry study after undergoing primary SG or RYGB, with a follow-up period of five years.
The patient’s condition and the surgical center’s expertise together determined the surgical indication and procedure selection.
Particularly in regions such as the Middle East and the United States, where chronic obesity is widespread, the current prevalence of SG is approximately 70% [11]. This pattern is also observed in Germany and Europe [12]. In an international comparison, our data suggest that the indication for surgery in Germany is relatively late and occurs only in the transition from obesity to superobesity (BMI > 50 kg/m2). The mean BMI in this study was 49 kg/m2.
Due to a lack of follow-up, the study was able to evaluate only 2,524 of the 54,984 patients for whom data were available at five years postoperatively. The decrease in follow-up rates (95.41%) over a 5-year period is due to the patients’ commitment to attending follow-up sessions rather than being influenced by the treating clinics. The substantial loss to follow-up rate implies that long-term outcomes may exceed those of the “lost” residual population; therefore, a thorough critical evaluation of the long-term data is imperative.
The analysis yielded notable results due to the variation within each category and the gender disparities in the distribution of bariatric surgery.
We believe that the consistent use of SG in male patients results in a higher preoperative BMI compared to female patients. Other studies that have examined patients with preoperative elevated BMIs have reached the same conclusion: SG was used at a higher rate compared to RYGB [13, 14].
Regarding the reduction in BMI, the %EWL, and weight loss after both procedures, three studies [15,16,17] demonstrated a greater reduction in BMI after RYGB, while two studies [18, 19] found no significant difference (Table 5). Eight studies [15,16,17,18,19,20,21,22] used %EWL as a measure of weight loss after both procedures. Three studies [15, 16, 20] reported a significantly higher %EWL five years after RYGB (Table 6). Our research findings indicate that RYGB demonstrated a statistically significant superiority in terms of %EWL. However, there were no significant differences seen in weight loss or change in BMI between the two procedures (Tables 2, 5, and 6). Based on the development of BMI, weight and %EWL and the preoperative values, the statement about %EWL development in our study should be viewed skeptically due to the different initial weight of the two groups. Therefore, this progress should not be the only consideration when deciding on surgical procedures; other demographic and patient-specific factors should also be taken into account. In addition, the initial BMI and perioperative conditions of the patients may have influenced the choice of procedure but not the postoperative course. In our opinion, the surgical procedure has a greater impact on weight loss, %EWL, and BMI decrease, as indicated in the literature and our study results, rather than the initial preoperative weight and BMI values, despite statistical significance.
In the current study, more than 90% of patients had preoperative comorbidities. However, the follow-up period was only five years and focused on T2D, aHTN, OSAS, and GERD.
According to the available studies, there were no significant changes between the two groups five years after surgery, even though both surgeries improve T2D [15,16,17]. Perrone et al. [22] found a significant difference in T2D remission rate at five years in favor of RYGB. 9,710 patients with T2D were followed for five years in a large American registry study [23]. The study reported first-year remission rates for RYGB (59.2%) and SG (55.7%). There were significant differences between the two groups at the five-year mark: remission rates increased to 86.1% after RYGB and 83.5% after SG. When comparing the preoperative and five-year follow-up status for remission of IDDM and NIDDM, our results did not show a statistically significant difference. There was a significant difference in the remission of IDDM in favor of the RYGB group five years after surgery compared to the previous controls during follow-up (p = 0.003), but not in the remission of NIDDM (p = 0.125). Therefore, the results of the literature and our registry study support the hypothesis that malabsorptive bariatric procedures (RYGB, BPD/DS) are more effective than restrictive procedures (SG, gastric banding) in terms of T2D remission.
In the case of aHTN, Salminen et al. [19] found that the remission rate after RYGB was significantly higher than after SG. Other studies [15,16,17,18, 21, 22] have found only a trend towards a benefit for RYGB compared to SG, but no significant benefit was observed. Our GBSR study showed remarkable remission rates for aHTN five years after the above surgical procedures (Table 7). In contrast to the remission rate of 47.8% for SG, RYGB resulted in a significantly higher remission rate of 54.4% (p = 0.024) when comparing the two surgical procedures.
Comparing the two surgical groups, slightly more than one fifth of the patients in our study had OSAS (Table 1). Both cohorts had significant remission rates. They were significantly higher after RYGB with 64.5% compared to 50.1% after SG (Table 3). The present study compared four searches [16, 18, 21, 22], all of which examined the progression of OSAS (Table 7). Remission rates were found to be predominantly high for both procedures, with no significant differences. Consistent with the results of the current study and the existing literature, both procedures induce OSAS remission. We believe that the differences between the two procedures do not only depend on the surgical approach, but also on demographic variables, postoperative weight loss, and observation schedule.
It has been observed that GERD is more common after SG than after RYGB [24]. Some surgeons even require preoperative impedance and manometry measurements. If positive results are obtained, RYGB [25] should be performed. Significant determinants associated with the development of gastroesophageal reflux disease (GERD) after SG are fundus resection, suspension apparatus modifications at the gastroesophageal junction, and the high-pressure system of the sleeve stomach [26, 27]. As a result, the incidence of de-novo GERD is high, while the remission rate of pre-existing GERD is minimal [25, 28]. In our study, 10% of cases undergoing RYGB developed de-novo GERD, compared to 29.5% in SG. Peterli et al. [18] observed comparable results in their study of de-novo GERD: 31.6% adherence to SG and 10.7% adherence to RYGB (p = 0.001).
An inherent limitation of our study is the lack of randomization. Randomization of patients is largely discouraged and often outright rejected in Germany due to strict ethical standards.
Furthermore, the study has a 95% follow-up loss rate, which is not subject to variation by the treating clinics and surgeons. Consequently, we can only characterize the outcomes of the two procedures based on the results obtained from the available data. Therefore, the conclusions drawn from the existing body of literature should be taken into account in conjunction with the recommendations of this study, and not in isolation.
Despite these limitations, our aim is to use sophisticated statistical analysis to bring existing registry data up to the standard of a randomized trial. Based on our assessment, the results of our study are comparable to those observed in international randomized trials.
Conclusion
The primary aim of this study was to ensure the quality of bariatric surgery, to evaluate the potential hazards associated with the procedure, and define patient selection criteria for both SG and RYGB through data analysis. The study revealed significant differences in the prevalence of GERD, aHTN, and OSAS among the comorbidities studied. The incidence of newly developed postoperative reflux within five years was three times higher after SG compared to RYGB. Remission of aHTN, OSAS, IDDM, and GERD was significantly greater after RYGB than after SG.
The results of the study indicate that the RYGB procedure has superior performance in several categories, suggesting its superiority over SG.
The literature indicates that SG is a reliable and widely used bariatric surgical technique known for its straightforward technical configuration and impeccable safety record. Therefore, given the advantages of RYGB over SG in the present study, it is imperative to carefully consider the merits of each bariatric procedure in order to achieve the most favorable expected outcomes from bariatric surgery. Therefore, when evaluating the acceptability of the procedure, additional factors such as patient consent, preoperative risk factors, and surgeon expertise should be considered in addition to the outcomes of the two procedures.
In addition to the specific procedure itself, bariatric surgery typically requires a comprehensive multidisciplinary therapeutic approach, including postoperative patient care.
Data availability
No datasets were generated or analysed during the current study.
References
Al-Goblan AS, Al-Alfi MA, Khan MZ (2014) Mechanism linking diabetes mellitus and obesity. Diabetes Metab Syndr Obes 7:587–591. https://doi.org/10.2147/DMSO.S67400
Christou NV, Sampalis JS, Liberman M et al (2004) Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg 240(3):416–424. https://doi.org/10.1097/01.SLA.0000137343.63376.19
Wang Y, Shirore RM, Ramakrishnan C, Tan NC, Jafar TH (2019) Adiposity measures and pre-diabetes or diabetes in adults with hypertension in Singapore polyclinics. J Clin Hypertens 21(7):953. https://doi.org/10.1111/JCH.13587
Coroyannakis C, Khalil A (2019) Management of Hypertension in the Obese Pregnant Patient. Curr Hypertens Rep. 21(3). https://doi.org/10.1007/S11906-019-0927-X
Fischer L, Wekerle AL, Sander J et al (2017) Is there a Reason Why Obese Patients Choose Either Conservative Treatment or Surgery? Obes Surg 27(7):1684–1690. https://doi.org/10.1007/S11695-016-2534-0
Maciejewski ML, Arterburn DE, Van Scoyoc L et al (2016) Bariatric Surgery and Long-term Durability of Weight Loss. JAMA Surg 151(11):1046–1055. https://doi.org/10.1001/JAMASURG.2016.2317
Angrisani L, Santonicola A, Iovino P, Ramos A, Shikora S, Kow L (2021) Bariatric Surgery Survey 2018: Similarities and Disparities Among the 5 IFSO Chapters. Obes Surg 31(5):1937–1948. https://doi.org/10.1007/S11695-020-05207-7
English WJ, DeMaria EJ, Hutter MM et al (2020) American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis 16(4):457–463. https://doi.org/10.1016/J.SOARD.2019.12.022
Benotti P, Wood GC, Winegar DA et al (2014) Risk Factors Associated With Mortality After Roux-en-Y Gastric Bypass Surgery. Ann Surg 259(1):123. https://doi.org/10.1097/SLA.0B013E31828A0EE4
Arakawa R, Febres G, Cheng B, Krikhely A, Bessler M, Korner J (2020) Prospective study of gut hormone and metabolic changes after laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. PLoS One.;15(7). https://doi.org/10.1371/JOURNAL.PONE.0236133
Angrisani L, Santonicola A, Iovino P, Ramos A, Shikora S, Kow L (2021) Bariatric Surgery Survey 2018: Similarities and Disparities Among the 5 IFSO Chapters. Obes Surg 31(5):1937–1948. https://doi.org/10.1007/S11695-020-05207-7
Thaher O, Driouch J, Hukauf M, Glatz T, Croner RS, Stroh C (2022) Is development in bariatric surgery in Germany compatible with international standards? A review of 16 years of data. Updates Surg 74(5):1571–1579. https://doi.org/10.1007/S13304-022-01349-8
Serrano OK, Tannebaum JE, Cumella L et al (2016) Weight loss outcomes and complications from bariatric surgery in the super super obese. Surg Endosc 30(6):2505–2511. https://doi.org/10.1007/S00464-015-4509-Y
Arapis K, Macrina N, Kadouch D, Ribeiro Parenti L, Marmuse JP, Hansel B (2019) Outcomes of Roux-en-Y gastric bypass versus sleeve gastrectomy in super-super-obese patients (BMI ≥60 kg/m2): 6-year follow-up at a single university. Surg Obes Relat Dis 15(1):23–33. https://doi.org/10.1016/J.SOARD.2018.09.487
Toolabi K, Sarkardeh M, Vasigh M, Golzarand M, Vezvaei P, Kooshki J (2020) Comparison of Laparoscopic Roux-en-Y Gastric Bypass and Laparoscopic Sleeve Gastrectomy on Weight Loss, Weight Regain, and Remission of Comorbidities: A 5 Years of Follow-up Study. Obes Surg 30(2):440–445. https://doi.org/10.1007/S11695-019-04183-X
Zhang Y, Zhao H, Cao Z et al (2014) A randomized clinical trial of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy for the treatment of morbid obesity in China: a 5-year outcome. Obes Surg 24(10):1617–1624. https://doi.org/10.1007/S11695-014-1258-2
Schauer PR, Bhatt DL, Kirwan JP et al (2017) Bariatric Surgery versus Intensive Medical Therapy for Diabetes - 5-Year Outcomes. N Engl J Med 376(7):641–651. https://doi.org/10.1056/NEJMOA1600869
Peterli R, Wolnerhanssen BK, Peters T et al (2018) Effect of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Roux-en-Y Gastric Bypass on Weight Loss in Patients With Morbid Obesity: The SM-BOSS Randomized Clinical Trial. JAMA 319(3):255–265. https://doi.org/10.1001/JAMA.2017.20897
Salminen P, Helmio M, Ovaska J et al (2018) Effect of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Roux-en-Y Gastric Bypass on Weight Loss at 5 Years Among Patients With Morbid Obesity: The SLEEVEPASS Randomized Clinical Trial. JAMA 319(3):241–254. https://doi.org/10.1001/JAMA.2017.20313
Ignat M, Vix M, Imad I et al (2017) Randomized trial of Roux-en-Y gastric bypass versus sleeve gastrectomy in achieving excess weight loss. Br J Surg 104(3):248–256. https://doi.org/10.1002/BJS.10400
Leyba JL, Llopis SN, Aulestia SN (2014) Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the treatment of morbid obesity. a prospective study with 5 years of follow-up. Obes Surg. 24(12):2094–2098. https://doi.org/10.1007/S11695-014-1365-0
Perrone F, Bianciardi E, Ippoliti S, Nardella J, Fabi F, Gentileschi P (2017) Long-term effects of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass for the treatment of morbid obesity: a monocentric prospective study with minimum follow-up of 5 years. Updates Surg 69(1):101–107. https://doi.org/10.1007/S13304-017-0426-Z
McTigue KM, Wellman R, Nauman E et al. (2020) Comparing the 5-Year Diabetes Outcomes of Sleeve Gastrectomy and Gastric Bypass: The National Patient-Centered Clinical Research Network (PCORNet) Bariatric Study. JAMA Surg. 155(5). https://doi.org/10.1001/JAMASURG.2020.0087
Peng B qiang, Zhang G xiang, Chen G, Cheng Z, Hu J kun, Du X (2020) Gastroesophageal reflux disease complicating laparoscopic sleeve gastrectomy: current knowledge and surgical therapies. Surg Obes Relat Dis. 16(8):1145–1155. https://doi.org/10.1016/J.SOARD.2020.04.025
Felsenreich DM, Ladinig LM, Beckerhinn P et al (2018) Update: 10 Years of Sleeve Gastrectomy-the First 103 Patients. Obes Surg 28(11):3586–3594. https://doi.org/10.1007/S11695-018-3399-1
Saber AA (2019) Gastric Migration After Bariatric Surgery. Obes Surg 29(7):2307–2308. https://doi.org/10.1007/S11695-019-03875-8/METRICS
Runkel N (2019) The Gastric Migration Crisis in Obesity Surgery. Obes Surg 29(7):2301–2302. https://doi.org/10.1007/S11695-019-03872-X
Csendes A, Orellana O, Martínez G, Burgos AM, Figueroa M, Lanzarini E (2019) Clinical, Endoscopic, and Histologic Findings at the Distal Esophagus and Stomach Before and Late (10.5 Years) After Laparoscopic Sleeve Gastrectomy: Results of a Prospective Study with 93% Follow-Up. Obes Surg. 29(12):3809–3817. https://doi.org/10.1007/S11695-019-04054-5
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Omar Thaher and Friederike Wollenhaupt study concept, literature review, preparation of data for statistical analysis, manuscript writing. Martin Hukauf preparation of data for statistical analysis and approval of statistical results and outcomes. Roland S. Croner and Christine Stroh study concept revision of manuscript, final approval of the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethical approval
For this type of retrospective study, no formal consent was required. All data were gathered and analyzed in accordance with the privacy and ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• The primary aim of this study was to ensure the quality of both SG and RYGB through data analysis.
• The incidence of newly developed postoperative reflux within five years was three times higher after SG compared to RYGB.
• The remission of hypertension, IDDM, and GERD was significantly greater after RYGB compared to SG.
• The results of this study suggest that RYGB is the preferred method over SG, as it achieved better results than SG in several areas.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thaher, O., Wollenhaupt, F., Croner, R.S. et al. Evaluation of the effect of sleeve gastrectomy versus Roux-en-Y gastric bypass in patients with morbid obesity: multicenter comparative study. Langenbecks Arch Surg 409, 156 (2024). https://doi.org/10.1007/s00423-024-03341-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-024-03341-9