Abstract
Purpose
Preoperative pain is known as one of the most powerful risk factors for chronic postoperative inguinal pain (CPIP), while its pathogenesis has not been fully elucidated. The aim of the present study was to evaluate patients with preoperative pain from the pathological perspective and discuss the potential pathogenesis of CPIP in those patients.
Methods
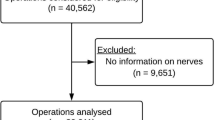
This was a single-institutional retrospective study. The study population was inguinal hernia patients with preoperative pain who underwent open anterior hernia repair for primary inguinal hernia with pragmatic ilioinguinal neurectomy during surgery between March 2021 and March 2023. The primary and secondary outcomes were proportion of collagen deposition and mucus accumulation within ilioinguinal nerve in those patients, respectively, which were evaluated histologically using Image J software.
Results
Forty patients were evaluated. Median value of proportion of intraneural collagen deposition was 38.3% (27.7–95.9). These values were positively correlated with the duration of pain (r2=0.468, P<0.001). Median value of proportion of mucus accumulation in ilioinguinal nerve was 50.1% (0–82.0). These values had no correlation with any clinicopathological variables.
Conclusions
In the present study population, all patients with preoperative pain had intraneural fibrosis within ilioinguinal nerve, and its degree had a positive correlation with the pain duration.




Similar content being viewed by others
Data Availability
All data in the present study are fully available without restriction. The data underlying the findings of this study are either available in the manuscript or upon request from the corresponding author, Masato Narita.
References
Lundstrom KJ, Holmberg H, Montgomery A, Nordin P (2018) Patient-reported rates of chronic pain and recurrence after groin hernia repair. Br J Surg 105(1):106–112
Bullen NL, Massey LH, Antoniou SA, Smart NJ, Fortelny RH (2019) Open versus laparoscopic mesh repair of primary unilateral uncomplicated inguinal hernia: a systematic review with meta-analysis and trial sequential analysis. Hernia 23(3):461–472
Patterson TJ, Beck J, Currie PJ, Spence RAJ, Spence G (2019) Meta-analysis of patient-reported outcomes after laparoscopic versus open inguinal hernia repair. Br J Surg 106(7):824–836
Niebuhr H, Wegner F, Hukauf M, Lechner M, Fortelny R, Bittner R et al (2018) What are the influencing factors for chronic pain following TAPP inguinal hernia repair: an analysis of 20,004 patients from the Herniamed Registry. Surg Endosc 32(4):1971–1983
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–165
Wright R, Born DE, D'Souza N, Hurd L, Gill R, Wright D (2017) Why do inguinal hernia patients have pain? Histology points to compression neuropathy. Am J Surg 213(5):975–982
Wright R, Born DE, D'Souza N, Hurd L, Gill R, Wright D (2017) Pain and compression neuropathy in primary inguinal hernia. Hernia 21(5):715–722
Wright R, Salisbury T, Landes J (2019) Groin anatomy, preoperative pain, and compression neuropathy in primary inguinal hernia: what really matters. Am J Surg 217(5):873–877
Narita M, Moriyoshi K, Goto K, Yamaoka R, Yamaguchi T (2021) A pathological perspective to painful inguinal hernia: report of two cases. Int J Surg Case Rep 86:106389
Moriyama M, Narita M (2023) Moriyoshi K (2023) Who is a candidate for open anterior hernia repair in the era of laparoscopic surgery? Asian J Endosc Surg. 16(4):827–828
Shouldice EB (2003) The Shouldice repair for groin hernias. Surg Clin North Am 83(5):1163–87, vii
Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH et al (2007) The European hernia society groin hernia classification: simple and easy to remember. Hernia 11(2):113–116
Ushiki T, Ide C (1986) Three-dimensional architecture of the endoneurium with special reference to the collagen fibril arrangement in relation to nerve fibers. Arch Histol Jpn 49(5):553–563
Mackinnon SE, Dellon AL, Hudson AR, Hunter DA (1986) Chronic human nerve compression--a histological assessment. Neuropathol Appl Neurobiol 12(6):547–565
Bhatia M, Thomson L (2020) Morton's neuroma - current concepts review. J Clin Orthop Trauma 11(3):406–409
Wynn TA (2004) Fibrotic disease and the T(H)1/T(H)2 paradigm. Nat Rev Immunol 4(8):583–594
Rockey DC, Bell PD, Hill JA (2015) Fibrosis--a common pathway to organ injury and failure. N Engl J Med. 372(12):1138–1149
Kockerling F, Bittner R, Kofler M, Mayer F, Adolf D, Kuthe A et al (2019) Lichtenstein versus total extraperitoneal patch plasty versus transabdominal patch plasty technique for primary unilateral inguinal hernia repair: a registry-based, propensity score-matched comparison of 57,906 Patients. Ann Surg 269(2):351–357
Hurel R, Bouazzi L, Barbe C, Kianmanesh R, Romain B, Gillion JF et al (2023) Lichtenstein versus TIPP versus TAPP versus TEP for primary inguinal hernia, a matched propensity score study on the French Club Hernie Registry. Hernia 27(5):1165–1177
Cirocchi R, Sutera M, Fedeli P, Anania G, Covarelli P, Suadoni F et al (2021) Ilioinguinal Nerve Neurectomy Is Better Than Preservation In Lichtenstein Hernia Repair: A Systematic Literature Review And Meta-Analysis. World J Surg 45(6):1750–1760
Charalambous MP, Charalambous CP (2018) Incidence of chronic groin pain following open mesh inguinal hernia repair, and effect of elective division of the ilioinguinal nerve: meta-analysis of randomized controlled trials. Hernia 22(3):401–409
Author information
Authors and Affiliations
Contributions
MN, R.Y., MM, KD, MF, HK, and TS collected and analyzed the data. MN wrote the main manuscript. KM performed pathological assessment and prepared figures. HN, GN, YN, and HH made a critical appraisal and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Narita, M., Moriyoshi, K., Yamaoka, R. et al. Intraneural fibrosis within ilioinguinal nerve in inguinal hernia patients with preoperative pain: it’s the sign of irreversible nerve injury, isn’t it?. Langenbecks Arch Surg 408, 431 (2023). https://doi.org/10.1007/s00423-023-03158-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03158-y