Abstract
Background
Despite its profound impact on the oncologic outcomes of rectal cancer, the most optimal surgical approach to total mesorectal excision (TME) has not been identified yet. All previous meta-analyses on this subject have been based on observational studies. This meta-analysis was conducted to assess the surgical and oncologic outcomes of laparoscopic TME (LaTME) compared to trans-anal TME (TaTME), utilizing only randomized controlled trials.
Design
Systematic review and meta-analysis of randomized controlled trials.
Methods
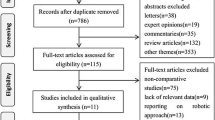
We searched electronic databases (MEDLINE, Cochrane CENTRAL, Clinicaltials.gov) from 2010 onwards, for all published clinical trials comparing TaTME to LaTME. Results are presented as risk ratios, with 95% CI, and pooled using the random effects model.
Results
A total of 1691 patients, from 6 eligible randomized controlled trials, were included for analysis. Analyzed data showed no significant difference in morbidity (RR: 0.85, p = 0.15), mortality (RR: 0.50, p = 0.44), conversion to open (RR: 0.40, p = 0.07), or anastomotic leakage (RR: 0.73, p = 0.10) between TaTME and LaTME. There was also no difference in the rate of positive distal resection margin (DRM) (RR: 0.55, p = 0.10) or positive circumferential resection margin (CRM) (RR: 0.67, p = 0.30). Patients undergoing TaTME were more likely to have a complete TME (RR: 1.06, p = 0.002) and shorter hospital stays (RR: − 0.97, p < 0.00001).
Conclusions
Patients undergoing TaTME for rectal cancer were more likely to have a complete TME when compared to LaTME, though this did not translate into improved distal or circumferential resection margin. Additionally, TaTME and LaTME had similar surgical outcomes except for shorter length of stay with TaTME.




Similar content being viewed by others
Data availability
The data used for the analysis was extracted from publicly available studies cited in the manuscript. All data analyses supporting the findings of this study are available within the paper and the supplementary information.
References
Results of treatment of carcinoma of the colon and rectum - PubMed. [cited 2023 Sep 15]. Available from: https://pubmed.ncbi.nlm.nih.gov/5120472/
Suwanabol PA, Maykel JA (2017) Laparoscopy, endoscopy, and minimally invasive colorectal surgery: transanal total mesorectal excision: a novel approach to rectal surgery. Clin Colon Rectal Surg 30(2):120–129. https://doi.org/10.1055/s-0036-1597314
Van Gijn W, Marijnen CAM, Nagtegaal ID, Kranenbarg EMK, Putter H, Wiggers T et al (2011) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 12(6):575–582. https://pubmed.ncbi.nlm.nih.gov/21596621/
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355. https://pubmed.ncbi.nlm.nih.gov/26441179/
Sylla P, Rattner DW, Delgado S, Lacy AM (2010) Notes transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc 4(5):1205–1210. https://pubmed.ncbi.nlm.nih.gov/20186432/
Zhang X, Gao Y, Dai XL, Zhang HT, Shang ZJ, Cai XY et al (2019) Short- and long-term outcomes of transanal versus laparoscopic total mesorectal excision for mid-to-low rectal cancer: a meta-analysis. SurgEndosc 33(3):972–985. https://pubmed.ncbi.nlm.nih.gov/30374790/
Lei PR, Ruan Y, Yang X, Fang J, Chen T (2018) Trans-anal or trans-abdominal total mesorectal excision? A systematic review and meta-analysis of recent comparative studies on perioperative outcomes and pathological result.Int J Surg 60:113–119.https://pubmed.ncbi.nlm.nih.gov/30415089/
Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J et al (2019) Incidence and risk factors for anastomotic failure in 1594 patients treated by transanal total mesorectal excision: results from the international TaTME registry. Ann Surg 269(4):700–711. https://pubmed.ncbi.nlm.nih.gov/29315090/
Larsen SG, Pfeffer F, Kørner H (2019) Norwegian moratorium on transanal total mesorectal excision. Br J Surg 106(9):1120–1121. https://pubmed.ncbi.nlm.nih.gov/31304578/
Alimova I, Chernyshov S, Nagudov M, Rybakov E (2021) Comparison of oncological and functional outcomes and quality of life after transanal or laparoscopic total mesorectal excision for rectal cancer: a systematic review and meta-analysis. Tech Coloproctol 25:901–913. https://doi.org/10.1007/s10151-021-02420-z
Moon JY, Lee MR, Ha GW (2022) Long-term oncologic outcomes of transanal TME compared with transabdominal TME for rectal cancer: a systematic review and meta-analysis. Surg Endosc 36(5):3122–3135. https://pubmed.ncbi.nlm.nih.gov/34169371/
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 29:372
RoB 2 (2023) A revised Cochrane risk-of-bias tool for randomized trials | Cochrane Bias. https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials
RevMan | Cochrane training. [cited 2023 Jun 12]. Available from: https://training.cochrane.org/online-learning/core-software/revman
Pontallier A, Denost Q, Van Geluwe B, Adam JP, Celerier B, Rullier E (2016) Potential sexual function improvement by using transanal mesorectal approach for laparoscopic low rectal cancer excision. Surg Endosc 30(11):4924–4933. https://link.springer.com/article/10.1007/s00464-016-4833-x
Serra-Aracil X, Zarate A, Bargalló J, Gonzalez A, Serracant A, Roura J et al (2023) Transanal versus laparoscopic total mesorectal excision for mid and low rectal cancer (Ta-LaTME study): multicentre, randomized, open-label trial. Br J Surg. 110(2):150–8. https://doi.org/10.1093/bjs/znac324
Denost Q, Adam JP, Rullier A, Buscail E, Laurent C, Rullier E (2014) Perineal transanal approach: a new standard for laparoscopic sphincter-saving resection in low rectal cancer, a randomized trial. Ann Surg 260(6):993–999. https://pubmed.ncbi.nlm.nih.gov/24950270/
Liu H, Zeng Z, Zhang H, Wu M, Ma D, Wang Q et al (2023) Morbidity, mortality, and pathologic outcomes of transanal versus laparoscopic total mesorectal excision for rectal cancer short-term outcomes from a multicenter randomized controlled trial. Ann Surg 277(1):1–6. https://pubmed.ncbi.nlm.nih.gov/35815886/
Zeng Z, Luo S, Chen J, Cai Y, Zhang X, Kang L (2020) Comparison of pathological outcomes after transanal versus laparoscopic total mesorectal excision: a prospective study using Sdata from randomized control trial. Surg Endosc 34(9):3956–3962. https://link.springer.com/article/10.1007/s00464-019-07167-1
Ren J, Liu S, Luo H, Wang B, Wu F (2021) Comparison of short-term efficacy of transanal total mesorectal excision and laparoscopic total mesorectal excision in low rectal cancer. Asian J Surg 44(1):181–185
Li L, Wang T, Hu D, Wu D, Bi L, Luo Y et al (2022) Pathologic outcomes of transanal versus laparoscopic total mesorectal excision for rectal cancer: a meta-analysis of 26 studies. Int J Colorectal Dis 37(5):1063–1071. https://pubmed.ncbi.nlm.nih.gov/35411470/
Aubert M, Mege D, Panis Y (2020) Total mesorectal excision for low and middle rectal cancer: laparoscopic versus transanal approach—a meta-analysis. Surg Endosc 34(9):3908–3919. https://link.springer.com/article/10.1007/s00464-019-07160-8
Hajibandeh S, Hajibandeh S, Eltair M, George AT, Thumbe V, Torrance AW et al (2020) Meta-analysis of transanal total mesorectal excision versus laparoscopic total mesorectal excision in management of rectal cancer. Int J Colorectal Dis 35(4):575–593. https://pubmed.ncbi.nlm.nih.gov/32124047/
Lin D, Yu Z, Chen W, Hu J, Huang X, He Z et al (2019) Transanal versus laparoscopic total mesorectal excision for mid and low rectal cancer: a meta-analysis of short-term outcomes. Wideochir Inne Tech Maloinwazyjne 14(3):353–365. https://doi.org/10.5114/wiitm.2019.82798
Zhang X, Gao Y, Dai XL, Zhang HT, Shang ZJ, Cai XY et al (2019) Short- and long-term outcomes of transanal versus laparoscopic total mesorectal excision for mid-to-low rectal cancer: a meta-analysis. Surg Endosc 33(3):972–985. https://pubmed.ncbi.nlm.nih.gov/30374790/
Lin D, Yu Z, Chen W, Hu J, Huang X, He Z et al (2019) Transanal versus laparoscopic total mesorectal excision for mid and low rectal cancer: a meta-analysis of short-term outcomes. Wideochir Inne Tech Maloinwazyjne 14(3):353–365. https://doi.org/10.5114/wiitm.2019.82798
Detering R, Rutgers MLW, Bemelman WA, Hompes R, Tanis PJ (2021) Prognostic importance of circumferential resection margin in the era of evolving surgical and multidisciplinary treatment of rectal cancer: a systematic review and meta-analysis. Surgery 170(2):412–431
Munini M, Popeskou SG, Galetti K, Roesel R, Mongelli F, Christoforidis D (2021) Transanal (TaTME) vs. laparoscopic total mesorectal excision for mid and low rectal cancer: a propensity score-matched analysis of early and long-term outcomes. Int J Colorectal Dis 36(10):2271–2279. https://click.endnote.com/viewer?doi=10.1007%2Fs00384-021-04019-0&token=WzM0NDgxMjcsIjEwLjEwMDcvczAwMzg0LTAyMS0wNDAxOS0wIl0.q_mVZP5dedpmVARr8kvtpmJozs0
Heald RJ, Ryall RDH (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1(8496):1479–482. https://pubmed.ncbi.nlm.nih.gov/2425199/
MacFarlane JK, Ryall RDH, Heald RJ (1993) Mesorectal excision for rectal cancer. Lancet 341(8843):457–460. https://pubmed.ncbi.nlm.nih.gov/8094488/
Jiang HP, Li Y Sen, Wang B, Wang C, Liu F, Shen ZL et al (2018) Pathological outcomes of transanal versus laparoscopic total mesorectal excision for rectal cancer: a systematic review with meta-analysis. Surg Endosc 32(6):2632–2642. https://pubmed.ncbi.nlm.nih.gov/29464401/
Knol J, Keller DS (2020) Total mesorectal excision technique-past, present, and future. Clin Colon Rectal Surg 33(3):134–143. https://pubmed.ncbi.nlm.nih.gov/32351336/
Simillis C, Lal N, Thoukididou SN, Kontovounisios C, Smith JJ, Hompes R et al (2019) Open versus laparoscopic versus robotic versus transanal mesorectal excision for rectal cancer: a systematic review and network meta-analysis. Ann Surg 270(1):59–68. https://journals.lww.com/annalsofsurgery/fulltext/2019/07000/open_versus_laparoscopic_versus_robotic_versus.12.aspx
Lee L, de Lacy B, Ruiz MG, Liberman AS, Albert MR, Monson JRT et al (2019) A multicenter matched comparison of transanal and robotic total mesorectal excision for mid and low-rectal adenocarcinoma. Ann Surg 270(6):1110–1116. https://journals.lww.com/annalsofsurgery/fulltext/2019/12000/a_multicenter_matched_comparison_of_transanal_and.27.aspx
Author information
Authors and Affiliations
Contributions
MF: project lead, planning, data analysis, and manuscript writing. AH: data extraction. AA: data analysis and tables. ZZ: data extraction. MD: data analysis and tables. AT; data extraction. LF: literature review and manuscript writing. RM: literature review and manuscript writing. AF: manuscript writing. AK, MD FACS: manuscript, guidance, and consultant advisor. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Farooqi, M., Hussain, A., Ahmad, A. et al. Impact of trans-anal versus laparoscopic total mesorectal excision on the surgical and pathologic outcomes of patients with rectal cancer: meta-analysis of randomized controlled trials. Langenbecks Arch Surg 408, 413 (2023). https://doi.org/10.1007/s00423-023-03147-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03147-1