Abstract
Background
Transanal total mesorectal excision (TaTME) appeared to be a challenging alternative to Laparoscopic Total Mesorectal Excision (LaTME) for low and middle rectal cancer. However, evidence remains low on the possible benefits of TaTME. The aim of this study was to perform a meta-analysis of comparative studies between TaTME and LaTME.
Methods
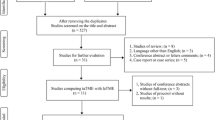
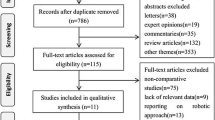
A systematic review and meta-analysis based on Preferred Reporting Items for Systematic reviews and Meta-analysis (PRISMA) guidelines was conducted on Medline, Embase, and Cochrane database. The following outcomes were assessed: conversion, operative time, morbidity, length of stay, readmission rate, and pathological and oncological results.
Results
After review of 756 identified records, 14 studies were included (case-matched control n = 10, prospective cohort n = 3, retrospective study n = 1) comparing 495 TaTME and 547 LaTME. No randomized trial was available. Following criteria were significantly improved after TaTME vs. LaTME: readmission’s rate (9% after TaTME vs. 18% after LaTME, OR 0.44, 95%CI 0.26–0.74, p = 0.002), length of stay (OR − 2.17, 95%CI − 3.68 to − 0.66, p = 0.005), overall morbidity (34 vs. 41%, OR 0.65, 95%CI 0.46-0.91, p = 0.001), major morbidity (8.7 vs. 14%, OR 0.53, 95%CI 0.34–0.83, p = 0.005), anastomotic leak (6.4 vs. 11.6%, OR 0.53, 95%CI 0.31–0.93, p = 0.03), and circumferential resection margin (CRM) involvement (4 vs. 8.8%, OR 0.48, 95%CI 0.27–0.86, p = 0.01). No significant differences were observed between TaTME and LaTME regarding conversion’s rate (3.2 vs. 8.8%, p = 0.09), operative time (OR − 10.73, p = 0.26), intraoperative complications (8.1 vs. 6.3%, p = 0.48), minor morbidity (27.9 vs. 29.6%, p = 0.27), positive distal resection margin (1.4 vs. 1.4%, p = 0.93), complete TME (75 vs. 75%, p = 0.74), harvested lymph nodes (OR 0.38, p = 0.44), and local recurrence rate (3.5 vs. 2.2%, p = 0.64).
Conclusion
This meta-analysis based on nonrandomized studies suggests that TaTME seems better than LaTME in terms of overall and major morbidities, anastomotic leak, readmission rate, CRM involvement, and length of stay. These results need to be confirmed by randomized controlled trial.








Similar content being viewed by others
References
Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RGS, Barzi A, Jemal A (2017) Colorectal cancer statistics, 2017. CA Cancer J Clin 67:177–193
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery—the clue to pelvic recurrence? Br J Surg 69:613–616
Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP, Abbott CR, Scott N, Finan PJ, Johnston D, Quirke P (2002) Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg 235:449–457
Martling A, Singnomklao T, Holm T, Rutqvist LE, Cedermark B (2004) Prognostic significance of both surgical and pathological assessment of curative resection for rectal cancer. Br J Surg 91:1040–1045
Van der Pas MHGM, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WCJ, Bonjer HJ (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218
Stevenson ARL, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Davies L, Wilson K, Hague W, Simes J (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314:1356–1363
Williams NS (2010) The rectal “no man’s land” and sphincter preservation during rectal excision. Br J Surg 97:1749–1751
Targarona EM, Balague C, Pernas JC, Martinez C, Berindoague R, Gich I, Trias M (2008) Can we predict immediate outcome after laparoscopic rectal surgery? Multivariate analysis of clinical, anatomic, and pathologic features after 3-dimensional reconstruction of the pelvic anatomy. Ann Surg 247:642–649
Sylla P, Rattner DW, Delgado S, Lacy AM (2010) NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc 24:1205–1210
Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J et al (2017) Transanal total mesorectal excision: international registry results of the first 720 cases. Ann Surg 266:111–117
Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J, Moran B, Hanna GB, Mortensen NJ, Tekkis PP (2018) Incidence and risk factors for anastomotic failure in 1594 patients treated by transanal total mesorectal excision. Ann Surg 269(4):700–711
Tuech JJ, Karoui M, Lelong B, De Chaisemartin C, Bridoux V, Manceau G, Delpero JR, Hanoun L, Michot F (2015) A step toward notes total mesorectal excision for rectal cancer endoscopic transanal proctectomy. Ann Surg 261:228–233
De Lacy FB, van Laarhoven JJEM, Pena R, Arroyave MC, Bravo R, Cuatrecasas M, Lacy AM (2018) Transanal total mesorectal excision: pathological results of 186 patients with mid and low rectal cancer. Surg Endosc 32:2442–2447
Lacy AM, Tasende MM, Delgado S, Fernandez-Hevia M, Jimenez M, De Lacy B, Castells A, Bravo R, Wexner SD, Heald RJ (2015) Transanal total mesorectal excision for rectal cancer: outcomes after 140 patients. J Am Coll Surg 221:415–423
Mege D, Hain E, Lakkis Z, Maggiori L, la Prost À Denise J, Panis Y (2018) Is trans-anal total mesorectal excision really safe and better than laparoscopic total mesorectal excision with a perineal approach first in patients with low rectal cancer? A learning curve with case-matched study in 68 patients. Color Dis 20:O143–O151
Lelong B, de Chaisemartin C, Meillat H, Cournier S, Boher JM, Genre D, Karoui M, Tuech JJ, Delpero JR (2017) A multicentre randomised controlled trial to evaluate the efficacy, morbidity and functional outcome of endoscopic transanal proctectomy versus laparoscopic proctectomy for low-lying rectal cancer (ETAP-GRECCAR 11 TRIAL): rationale and design. BMC Cancer 17:1–8
Deijen CL, Velthuis S, Tsai A, Mavroveli S, de Lange-de Klerk ESM, Sietses C, Tuynman JB, Lacy AM, Hanna GB, Bonjer HJ (2016) COLOR III: a multicentre randomised clinical trial comparing transanal TME versus laparoscopic TME for mid and low rectal cancer. Surg Endosc 30:3210–3215
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 62:1006–1012
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Quirke P, Steele R, Monson J, Grieve R, Khanna S, Couture J, O’Callaghan C, Myint AS, Bessell E, Thompson LC, Parmar M, Stephens RJ, Sebag-Montefiore D (2009) Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR20 and NCIC-CTG CO16 randomised clinical trial. Lancet 373:821–828
Rhodes KM, Mawdsley D, Turner RM, Jones HE, Savović J, Higgins JPT (2018) Label-invariant models for the analysis of meta-epidemiological data. Stat Med 37:60–70
Persiani R, Biondi A, Pennestrì F, Fico V, De Simone V, Tirelli F, Santullo F, D’Ugo D (2018) Transanal total mesorectal excision vs laparoscopic total mesorectal excision in the treatment of low and middle rectal cancer: a propensity score matching analysis. Dis Colon Rectum 61:809–816
Lelong B, Meillat H, Zemmour C, Poizat F, Ewald J, Mege D, Lelong JC, Delpero JR, de Chaisemartin C (2017) Short- and mid-term outcomes after endoscopic transanal or laparoscopic transabdominal total mesorectal excision for low rectal cancer: a single institutional case-control study. J Am Coll Surg 224:917–925
Chang T-C, Kiu K-T (2017) Transanal total mesorectal excision in lower rectal cancer: comparison of short-term outcomes with conventional laparoscopic total mesorectal excision. J Laparoendosc Adv Surg Tech 28:365–369
Marks JH, Montenegro GA, Salem JF, Shields MV (2016) Transanal TATA/TME : a case-matched study of taTME versus laparoscopic TME surgery for rectal cancer. Tech Coloproctol 20:467–473
Perdawood SK, Al Khefagie GAA (2016) Transanal vs laparoscopic total mesorectal excision for rectal cancer: initial experience from Denmark. Colorectal Dis 18:51–58
De’ Angelis N, Portigliotti L, Azoulay D, Brunetti F (2015) Transanal total mesorectal excision for rectal cancer: a single center experience and systematic review of the literature. Langenbeck’s Arch Surg 400:945–959
Fernández-Hevia M, Delgado S, Castells A, Tasende M, Momblan D, Del Gobbo GD, DeLacy B, Balust J, Lacy AM (2015) Transanal total mesorectal excision in rectal cancer short-term outcomes in comparison with laparoscopic surgery. Ann Surg 261:221–227
Velthuis S, Nieuwenhuis DH, Ruijter TEG, Cuesta MA (2014) Transanal versus traditional laparoscopic total mesorectal excision for rectal carcinoma. Surg Endosc 28:3494–3499
Chen C-C, Lai Y-L, Jiang J-K, Chu C-H, Huang I-P, Chen W-S, Cheng AY-M, Yang S-H (2016) Transanal total mesorectal excision versus laparoscopic surgery for rectal cancer receiving neoadjuvant chemoradiation: a matched case-control study. Ann Surg Oncol 23:1169–1176
Chouillard E, Regnier A, Vitte RL, Bonnet BV, Greco V, Chahine E, Daher R, Biagini J (2016) Transanal NOTES total mesorectal excision (TME) in patients with rectal cancer: is anatomy better preserved? Tech Coloproctol 20:537–544
Perdawood SK, Thinggaard BS, Bjoern MX (2017) Effect of transanal total mesorectal excision for rectal cancer: comparison of short-term outcomes with laparoscopic and open surgeries. Surg Endosc 32:2312–2321
Rasulov AO, Mamedli ZZ, Gordeyev SS, Kozlov NA, Dzhumabaev HE (2016) Short-term outcomes after transanal and laparoscopic total mesorectal excision for rectal cancer. Tech Coloproctol 20:227–234
Veltcamp Helbach M, Koedam TWA, Knol JJ, Diederik A, Spaargaren GJ, Bonjer HJ, Tuynman JB, Sietses C (2018) Residual mesorectum on postoperative magnetic resonance imaging following transanal total mesorectal excision (TaTME) and laparoscopic total mesorectal excision (LapTME) in rectal cancer. Surg Endosc 33(1):94–102
Veltcamp Helbach M, Koedam TWA, Knol JJ, Velthuis S, Bonjer HJ, Tuynman JB, Sietses C (2018) Quality of life after rectal cancer surgery: differences between laparoscopic and transanal total mesorectal excision. Surg Endosc 33(1):79–87
Perdawood SK, Warnecke M, Bjoern MX, Eiholm S (2018) The pattern of defects in mesorectal specimens: is there a difference between transanal and laparoscopic approaches? Scand J Surg 108(1):49–54
Koedam TWA, Veltcamp Helbach M, Penna M, Wijsmuller A, Doornebosch P, van Westreenen HL, Hompes R, Bonjer HJ, Sietses C, de Graaf E, Tuynman JB (2018) Short-term outcomes of transanal completion total mesorectal excision (cTaTME) for rectal cancer: a case-matched analysis. Surg Endosc 33(1):103–109
Edge SB, Compton CC (2010) The american joint committee on cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474
Rouanet P, Mourregot A, Azar CC, Carrere S, Gutowski M, Quenet F, Saint-Aubert B, Colombo PE (2013) Transanal endoscopic proctectomy: an innovative procedure for difficult resection of rectal tumors in men with narrow pelvis. Dis Colon Rectum 56:408–415
Atallah SB, DuBose AC, Burke JP, Nassif G, DeBeche-Adams T, Frering T, Albert MR, Monson JRT (2017) Uptake of transanal total mesorectal excision in North America: initial assessment of a structured training program and the experience of delegate surgeons. Dis Colon Rectum 60:1023–1031
Koedam TW, van Ramshorst GH, Deijen CL, Elfrink AK, Meijerink WJ, Bonjer HJ, Sietses C, Tuynman JB (2017) Transanal total mesorectal excision (TaTME) for rectal cancer: effects on patient-reported quality of life and functional outcome. Tech Coloproctol 21:25–33
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AMH, Heath RM, Brown JM (2005) Short-term endpoints of conventional versus laparoscopic- assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726
Jiang H-P, Li Y-S, Wang B, Wang C, Liu F, Shen Z-L, Ye Y-J, Wang S (2018) Pathological outcomes of transanal versus laparoscopic total mesorectal excision for rectal cancer: a systematic review with meta-analysis. Surg Endosc 32:2632–2642
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MHGM, de Lange-de Klerk ESM, Lacy AM, Bemelman WA, Andersson J, Angenete E, Rosenberg J, Fuerst A, Haglind E (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, Choi HS, Kim DW, Chang HJ, Kim DY, Jung KH, Kim TY, Kang GH, Chie EK, Kim SY, Sohn DK, Kim DH, Kim JS, Lee HS, Kim JH, Oh JH (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Dumont F, Goéré D, Honoré C, Elias D (2012) Transanal endoscopic total mesorectal excision combined with single-port laparoscopy. Dis Colon Rectum 55:996–1001
Ma B, Gao P, Song Y, Zhang C, Zhang C, Wang L, Liu H, Wang Z (2016) Transanal total mesorectal excision (taTME) for rectal cancer: a systematic review and meta-analysis of oncological and perioperative outcomes compared with laparoscopic total mesorectal excision. BMC Cancer 16:380
Xu W, Xu Z, Cheng H, Ying J, Cheng F, Xu W, Cao J, Luo J (2016) Comparison of short-term clinical outcomes between transanal and laparoscopic total mesorectal excision for the treatment of mid and low rectal cancer: a meta-analysis. Eur J Surg Oncol 42:1841–1850
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs Aubert, Mege, and Panis have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aubert, M., Mege, D. & Panis, Y. Total mesorectal excision for low and middle rectal cancer: laparoscopic versus transanal approach—a meta-analysis. Surg Endosc 34, 3908–3919 (2020). https://doi.org/10.1007/s00464-019-07160-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07160-8