Abstract
Purpose
The purpose of the study was to evaluate the usefulness of the triggering receptor expressed on myeloid cell 1 (TREM-1) protein as a marker for serious infectious complications during laparoscopic colorectal surgery.
Methods
Sixty-four patients with colon or rectal cancer, who underwent an elective laparoscopic colorectal cancer surgery from November 2018 to February 2020, were included in the analysis. Blood samples of the TREM-1 protein testing were collected four times from each patient: before and on three following postoperative days (PODs). Patients were divided into two groups according to the presence of infectious complications. Subsequently, patients with infectious complications (group 1) were matched 1:1 with patients without complications (group 2). The case-matched analysis was done by selecting patients from the control group by age, ASA scale, cancer stage, and type of surgery.
Results
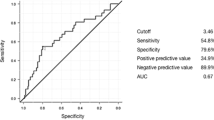
There was no significant difference in demographic and operative characteristics between the two groups. The median length of hospital stay was longer in group 1 than in group 2 (11 days vs. 5 days, p < 0.001). Preoperative measurements of TREM-1 protein did not differ between the two groups. There were no significant differences in the measurements on the first and third postoperative days. However, the median TREM-1 measurement was higher in group 1 on the second postoperative day (542 pg/ml vs. 399 pg/ml; p = 0.040). The difference was more apparent when only severe postoperative complications were considered. When compared to the group without any complications, the median TREM-1 level was significantly higher in the group with severe infection complications in POD 1, POD 2, and POD 3 (p < 0.05). The receiver operating characteristic (ROC) curve demonstrated that TREM-1 readings in POD 2 had a sensitivity of 83% and a specificity of 84% for the presence of severe infection complications at a value of 579.3 pg/ml (AUC 0.8, 95%CI 0.65–0.96).
Conclusion
TREM-1 measurements might become a helpful predictive marker in the early diagnosis of serious infectious complications in patients following laparoscopic colorectal surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of minimally invasive surgical techniques and tailored adjuvant treatment has contributed to a remarkable reduction in morbidity and mortality of patients with colorectal cancer [1]. In particular, the implementation of the Enhanced Recovery After Surgery (ERAS) guidelines has undeniably contributed to improving perioperative outcomes for these patients and reducing the length of hospital stay after surgery [2]. However, the significantly reduced length of stay (LOS), and, therefore, shorter time for close monitoring of the patient, is challenging, as some of the complications develop later than the typical LOS. The symptoms of postoperative infections usually become apparent 4–6 days after surgery [3]. Many studies indicate that infectious complications after colorectal resection still represent a substantial burden. They complicate up to 30% of procedures, contribute greatly to the need for readmission, and have an adverse effect on cancer-specific survival, and their inadequate treatment may promptly lead to sepsis and death [4,5,6].
Many attempts have been made to find markers that would help to identify patients at particular risk of developing an infection, in order to detect it as soon as possible and implement appropriate treatment. Well-known markers such as C-reactive protein (CRP), interleukin 6, or procalcitonin have been investigated as tools to predict the occurrence of postoperative infectious complications [7, 8]. However, none of them is fully reliable, mainly due to their late rise after surgery [3].
The TREM-1 (triggering receptor expressed on myeloid cell 1) glycoprotein, which belongs to the immunoglobulin superfamily, is a receptor involved in the activation of monocytes and neutrophils during the inflammatory process. There are many reports indicating that the soluble form of this receptor is a reliable diagnostic marker of infection and inflammatory response induced by trauma [9, 10]. TREM-1 has been described as a means to assess the risk of the occurrence of infections in some surgical conditions, but no one has studied its application in predicting complications in patients who underwent elective laparoscopic resection of colorectal cancer [11, 12]. Therefore, we set out to investigate the potential use of soluble TREM-1 (sTREM-1) to predict serious infectious complications in patients undergoing laparoscopic colorectal surgery.
Materials and methods
Patients with colon or rectal cancer, who underwent elective laparoscopic colorectal cancer surgery between November 2018 and February 2020, were included in the study. Blood samples for the TREM-1 protein assay were collected from each patient four times: preoperatively and on three following postoperative days (PODs). Clinical data and demographic information of patients (age, sex, comorbidities, ASA (American Society of Anaesthesiologists) physical status) were prospectively collected on the database. After the surgery, the database was supplemented with data related to the procedure (type of surgery, operative time, intraoperative blood loss) and treatment results (complications, length of hospital stay (LOS)).
We defined infectious complications as clinical signs of inflammation in different organs with elevated classical inflammatory parameters from blood samples. We included infectious complications involving all organs, resulting directly from surgical site complications, as well as those related to a general complication of hospitalization such as pneumonia. Complications were graded according to the five-grade Clavien-Dindo (CD) classification. We also divided complications into mild (CD 1–2) and severe (CD 3–5).
Patients with infectious complications who formed group 1 were matched 1:1 with patients without complications (group 2). Case-matched analysis was performed by selecting patients for the control group from the group of patients paired by age, ASA scale, stage of cancer, and type of surgery. Since 2012, in our department, the perioperative care of all patients is carried out based on the ERAS protocol, and the laparoscopic approach has been the gold standard in colorectal surgery at our center.
Inclusion and exclusion criteria
We included adult patients (> 18 years old) with histopathologically confirmed colorectal adenocarcinoma who underwent laparoscopic resection of the colon and/or rectum. Exclusion criteria were as follows: open or emergency surgery, multivisceral resection, stage IV cancer according to American Joint Committee on Cancer (AJCC) classification system, concomitant inflammatory bowel disease, autoimmune systemic disease, other active infection, or when conversion to open resection was necessary.
Sample size calculation
Due to the lack of previous research using the TREM-1 protein as a marker of infectious complications in surgery and the inability to predict the differences, we assumed that the 10% difference in measured sTREM-1 level represents a clinically relevant difference. Assuming the test power is 90%, we calculated that to detect this, at least 29 patients would be required in each treatment arm.
Blood samples
Blood samples were drawn four times: on the day of surgery (preoperatively) and on 3 following postoperative days (PODs). Blood was drawn at the same time in the morning, before the meal. Serum from the blood sample (1 vial of 4.9 ml) was centrifuged for 10 min at 4000 rpm and then frozen at −80 °C until all patients were included in the study. Quantikine ELISA Human TREM-1 kit from R&D systems was used. The minimal detectable dose (MDD) of human TREM-1 ranged from 2.65–15.2 pg/ml. The mean MDD was 7.69 pg/ml.
Statistical analysis
All data were analyzed with Statsoft STATISTICA v.13 (StatSoft Inc., Tulsa, OK, USA). The results were presented as mean ± standard deviation (SD) or median and interquartile range (IQR) when appropriate. Independent sample Student’s t-test was used to compare the means of two continuous normally distributed variables, the Mann-Whitney U test was used to compare the means of two continuous non-normally distributed variables, and the chi-squared test was used for categorical variables. A receiver operating characteristic (ROC) curve was applied to obtain the area under the curve (AUC) with a 95% confidence interval for AUC and determine the best cut-offs for measurements. Results were considered statistically significant when the p value was found to be less than 0.05.
Ethical approval
All procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from all participating patients before surgery. This study was approved by the local ethics review committee (approval number 1072.6120.246.2018) and was registered in the clinicaltrials.gov (NCT05933408).
Results
During the study period, a total of 136 patients with colorectal cancer were operated in our unit. Eighteen patients did not meet inclusion criteria (benign disease, primary open surgery, stage IV colorectal cancer). Out of the remaining 118 patients, 1 had multivisceral resection; 4 were converted; 2 needed ICU to stay immediately after surgery; 1 patient had concomitant inflammatory bowel disease; in 4 patients, metastases were found intraoperatively; and 2 had autoimmune systemic disease. Out of 104 patients, 32 had infectious complications and were included in group 1. Group 2 consisted of 32 patients without complications.
Sixty-four patients were included in the analysis (Fig. 1). Demographic and operative analysis of patient groups is presented in Table 1.
Of the group of 32 patients with complications, serious complications occurred in 13 of them (Table 2). The most common serious complication was anastomotic leak requiring surgery, which occurred in 7 patients. In 2 patients, the anastomotic leak was successfully treated endoscopically with endo-VAC. Other Clavien-Dindo grade 3 complications include pelvic abscess and peristomal fistula. One patient required an ICU stay due to pneumonia that occurred after reoperation caused by intestinal perforation. One patient died in the ICU due to pneumonia leading to respiratory failure.
Preoperative measurements of TREM-1 protein did not differ between groups. There were no significant differences in measurements between those groups on the first and third postoperative days. Median TREM-1 measurement was significantly higher in group 1 on the second postoperative day (542 vs. 399 pg/ml; p < 0.05), respectively. The difference was more noticeable when only severe postoperative complications were taken into consideration. Median TREM-1 level was significantly higher in the group with severe infectious complications when compared to the group without any complications in PODs 1 (p < 0.05), 2 (p < 0.05), and 3 (p < 0.05). Details of the biochemical analysis are provided in Table 3.
Also, the increase in sTREM values from baseline on consecutive days was significant in subsequent PODs. The differences were statistically significant on all days between the group of uncomplicated patients and those with severe infectious complications (Table 4).
The analysis showed that measurements on POD 2 were characterized by the most favorable ratio of sensitivity to specificity. The receiver operating characteristic (ROC) curve showed that TREM-1 measurements in POD 2 had a sensitivity of 83% and a specificity of 84% for value 579.3 pg/ml (AUC 0.8, 95%CI 0.65–0.96) to predict severe infectious complications. Figure 2 shows the ROC curves.
Discussion
In our study, serum TREM-1 levels were significantly higher in POD 2 in patients who developed infectious complications after surgery than in uncomplicated cases. Furthermore, in patients with severe complications (3–5 on the Clavien-Dindo scale), the rise in sTREM-1 levels was even more pronounced and occurred in PODs 1–3. Importantly, the analysis showed that measurements on POD 2 were characterized by the most favorable ratio of sensitivity to specificity (sensitivity of 83% and specificity of 84% for value 579.3 pg/ml).
Postoperative infectious complications are still a major burden in colorectal surgery as they occur in up to one-third of patients after elective operation and are associated with decreased survival [13]. Their accurate and early prediction could limit morbidity, and possibly improve patients’ long-term outcomes. Indeed, it is particularly important in the present era of minimally invasive surgery and ERAS protocol, when the time spent in the hospital after surgery has been significantly shortened and patients are discharged before most infection complications occur [3].
Due to the shortening of the period of stay and reduction of surgical trauma, many authors have been looking for plasma inflammatory markers as preclinical rapid predictors of infectious complications. To date, the most commonly used marker for screening the development of postoperative infections is C-reactive protein (CRP). Despite the established position of CRP as a protein associated with inflammation, findings regarding its accuracy in predicting complications in colorectal surgery vary widely between studies. For example, some authors have shown that in POD 4, CRP has only 44.4% sensitivity and as much as 98.5% specificity, while others reported 94.4% sensitivity and 64.6% specificity on that day [7, 8]. In addition, CRP is a non-specific marker of inflammation, its levels always rise after the operation as a result of a surgical stress response, and only sustained increased levels of POD 3 or POD 4 have predictive value in predicting infectious complications [14]. Some authors have therefore compared the diagnostic accuracy of PCT with that of CRP in the context of elective colorectal surgery. The conclusion was that the PCT determination is associated with much higher costs, and PCT is no better than CRP in this setting due to its low specificity [7, 14]. Another cytokine produced in response to various inflammatory mediators is interleukin 6 (IL-6). While Wierdak et al. reported a remarkably high ability to predict infectious complications, especially on POD 2 (91% sensitivity and 97% specificity), other studies have not supported this finding [3, 15, 16]. The main drawbacks of the IL-6 assay are its short half-life, which results in high variability in its concentration in patients’ blood, and the profound impact of chronic inflammatory diseases on its concentration [15]. As none of the well-known inflammatory proteins, such as CRP, PCT, or IL-6, are fully sufficient to predict the early occurrence of infectious complications after colorectal surgery, research into new markers that will have better diagnostic value is still needed.
The discovery of additional pathways used by host cells to recognize bacterial components appears promising. The glycoprotein TREM-1 is a receptor involved in the activation of monocytes and neutrophils in the inflammatory process. The literature indicates that soluble TREM-1 is an effective indicator to evaluate the severity and prognosis of infectious diseases [17, 18]. In addition, the concentration of sTREM-1 predicted septic complications better than CRP or PCT [19, 20]. Gonzalez-Roldán et al. showed that there was a significant difference in sTREM-1 blood levels between healthy volunteers and patients after elective gastrointestinal surgery, as well as between the uncomplicated surgery group and patients who developed sepsis [11]. Two studies in patients undergoing cardiac surgery confirmed that high sTREM-1 plasma concentrations correlated with the risk of infectious complications [12, 21]. Interestingly, patients who later developed complications showed a remarkable rise in sTREM-1 already at the end of surgery. Similarly to our study, a significant difference between the group with infectious complications and the group without complications occurred on POD 2 [12].
To the best of our knowledge, we were the first to show that monitoring sTREM-1 is a valuable tool in the early prediction of infectious complications of elective colorectal surgery. We are aware of the limitations of this study; however, it was designed to assess the usefulness of TREM-1 as a predictor of infectious complications in elective minimally invasive colorectal cancer surgery. The study sample is relatively small, and to reliably establish cut-off values, sTREM-1 should be tested in a larger cohort of patients undergoing laparoscopic colorectal surgery. Another limitation is that we did not analyze whether sTREM-1 levels also increase in non-infectious complications, but it has been suggested that there is no significant difference in TREM-1 levels between postoperative patients who developed an infection and surgical patients who developed a non-infectious complication [22].
Conclusion
The results of the present study indicate that sTREM-1 has the potential to be a valuable predictive marker in the early detection of severe infectious complications in patients undergoing laparoscopic colorectal surgery. In contrast to other widely used inflammatory markers, the level of sTREM-1 rises notably already on the first postoperative day in the group who have experienced serious complications. Our findings are of importance as monitoring the sTREM-1 level could identify patients who have a high risk of developing infectious complications after surgery and should stay in the hospital longer than a typical LOS lasts.
References
Ketelaers SHJ, Orsini RG, Burger JWA et al (2019) Significant improvement in postoperative and 1-year mortality after colorectal cancer surgery in recent years. Eur J Surg Oncol 45:2052–2058. https://doi.org/10.1016/J.EJSO.2019.06.017
Pisarska M, Pędziwiatr M, Małczak P et al (2016) Do we really need the full compliance with ERAS protocol in laparoscopic colorectal surgery? A prospective cohort study. Int J Surg 36:377–382. https://doi.org/10.1016/J.IJSU.2016.11.088
Wierdak M, Pisarska M, Kuśnierz-Cabala B et al (2018) Use of inflammatory markers in the early detection of infectious complications after laparoscopic colorectal cancer surgery with the ERAS protocol. Wideochir Inne Tech Maloinwazyjne 13:315–325. https://doi.org/10.5114/WIITM.2018.75846
Attiê R, Chinen LTD, Yoshioka EM et al (2014) Acute bacterial infection negatively impacts cancer specific survival of colorectal cancer patients. World J Gastroenterol 20:13930–13935. https://doi.org/10.3748/WJG.V20.I38.13930
Nowakowski M, Pisarska M, Rubinkiewicz M et al (2018) Postoperative complications are associated with worse survival after laparoscopic surgery for non-metastatic colorectal cancer - interim analysis of 3-year overall survival. Wideochir Inne Tech Maloinwazyjne 13:326–332. https://doi.org/10.5114/WIITM.2018.76179
Mehdorn M, Lübbert C, Chaberny IF et al (2021) Mechanical plus oral bowel preparation with paromomycin and metronidazole reduces infectious complications in elective colorectal surgery: a matched case-control study. Int J Colorectal Dis 36:1839–1849. https://doi.org/10.1007/S00384-021-03931-9
Amanai E, Nakai K, Saito J et al (2022) Usefulness of presepsin for the early detection of infectious complications after elective colorectal surgery, compared with C-reactive protein and procalcitonin. Sci Rep 12:3960. https://doi.org/10.1038/S41598-022-06613-W
Tatsuoka T, Okuyama T, Takeshita E et al (2021) Early detection of infectious complications using C-reactive protein and the procalcitonin levels after laparoscopic colorectal resection: a prospective cohort study. Surg Today 51:397–403. https://doi.org/10.1007/S00595-020-02111-6
Jiyong J, Tiancha H, Wei C, Huahao S (2009) Diagnostic value of the soluble triggering receptor expressed on myeloid cells-1 in bacterial infection: a meta-analysis. Intensive Care Med 35:587–595. https://doi.org/10.1007/S00134-008-1333-Z
Bingold TM, Pullmann B, Sartorius S et al (2011) Soluble triggering receptor on myeloid cells-1 is expressed in the course of non-infectious inflammation after traumatic lung contusion: a prospective cohort study. Crit Care 15:R115. https://doi.org/10.1186/CC10141
Gonzalez-Roldán N, Ferat-Osorio E, Aduna-Vicente R et al (2005) Expression of triggering receptor on myeloid cell 1 and histocompatibility complex molecules in sepsis and major abdominal surgery. World J Gastroenterol 11:7473–7479. https://doi.org/10.3748/WJG.V11.I47.7473
Stoppelkamp S, Veseli K, Stang K et al (2015) Identification of predictive early biomarkers for sterile-SIRS after cardiovascular surgery. PLoS One 10:e0135527. https://doi.org/10.1371/JOURNAL.PONE.0135527
Artinyan A, Orcutt ST, Anaya DA et al (2015) Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: a study of 12,075 patients. Ann Surg 261:497–505. https://doi.org/10.1097/SLA.0000000000000854
Cousin F, Ortega-Deballon P, Bourredjem A et al (2016) Diagnostic accuracy of procalcitonin and C-reactive protein for the early diagnosis of intra-abdominal infection after elective colorectal surgery: a meta-analysis. Ann Surg 264:252–256. https://doi.org/10.1097/SLA.0000000000001545
Zielińska-Borkowska U, Dib N, Tarnowski W, Skirecki T (2017) Monitoring of procalcitonin but not interleukin-6 is useful for the early prediction of anastomotic leakage after colorectal surgery. Clin Chem Lab Med 55:1053–1059
Bilgin IA, Hatipoglu E, Aghayeva A et al (2017) Predicting value of serum procalcitonin, C-reactive protein, drain fluid culture, drain fluid interleukin-6, and tumor necrosis factor-α levels in anastomotic leakage after rectal resection. Surg Infect (Larchmt) 18:350–356
Wang Y, Zhang S, Li L, Xie J (2019) The usefulness of serum procalcitonin, C-reactive protein, soluble triggering receptor expressed on myeloid cells 1 and clinical pulmonary infection score for evaluation of severity and prognosis of community-acquired pneumonia in elderly patients. Arch Gerontol Geriatr 80:53–57. https://doi.org/10.1016/J.ARCHGER.2018.10.005
Liu Y, Tian L, You J, Li Y (2021) The predictive value of postoperative C-reactive protein (CRP), procalcitonin (PCT) and triggering receptor expressed on myeloid cells 1 (TREM-1) for the early detection of pulmonary infection following laparoscopic general anesthesia for cervical cancer treatment. Ann Palliat Med 10:4502–4508. https://doi.org/10.21037/APM-21-554
Su L, Feng L, Song Q et al (2013) Diagnostic value of dynamics serum sCD163, sTREM-1, PCT, and CRP in differentiating sepsis, severity assessment, and prognostic prediction. Mediators Inflamm 2013:969875. https://doi.org/10.1155/2013/969875
Zhang J, She D, Feng D et al (2011) Dynamic changes of serum soluble triggering receptor expressed on myeloid cells-1 (sTREM-1) reflect sepsis severity and can predict prognosis: a prospective study. BMC Infect Dis 11:53. https://doi.org/10.1186/1471-2334-11-53
Golovkin AS, Matveeva VG, Grigoriev EV et al (2012) sTREM-1 as a prognostic marker of postoperative complications in cardiac surgery. ISRN Inflamm 2012:1–5. https://doi.org/10.5402/2012/382862
Ferat-Osorio E, Esquivel-Callejas N, Wong-Baeza I et al (2008) The increased expression of TREM-1 on monocytes is associated with infectious and noninfectious inflammatory processes. J Surg Res 150:110–117. https://doi.org/10.1016/J.JSS.2007.12.805
Funding
This study was conducted with funding from the Jagiellonian University (K/DSC/005286).
Author information
Authors and Affiliations
Contributions
Study conception and design: Magdalena Pisarska-Adamczyk and Mateusz Wierdak. Acquisition of data: Magdalena Pisarska-Adamczyk, Anna Rzepa, Mateusz Wierdak, Michał Wysocki, Piotr Małczak, Piotr Major, and Anna Zub-Pokrowiecka. Analysis and interpretation of data: Magdalena Pisarska-Adamczyk, Mateusz Wierdak, Karolina Zawadzka, Maria Kapusta, and Beata Kuśnierz-Cabala. Drafting of manuscript: Magdalena Pisarska-Adamczyk, Mateusz Wierdak, and Karolina Zawadzka. Critical revision of manuscript: Michał Pędziwiatr, Piotr Major, and Mateusz Wierdak.
Corresponding author
Ethics declarations
Consent to participate
Authors, Magdalena Pisarska-Adamczyk MD PhD, Anna Rzepa MD, Maria Kapusta PhD, Karolina Zawadzka MD, Beata Kuśnierz-Cabala PhD, Michał Wysocki MD PhD, Piotr Małczak MD PhD, Piotr Major MD PhD, Mateusz Wierdak MD PhD, and Michał Pędziwiatr MD PhD, declare that all participants have consented to this research study.
Consent to publication
Authors, Magdalena Pisarska-Adamczyk MD PhD, Anna Rzepa MD, Maria Kapusta PhD, Karolina Zawadzka MD, Beata Kuśnierz-Cabala PhD, Michał Wysocki MD PhD, Piotr Małczak MD PhD, Piotr Major MD PhD, Mateusz Wierdak MD PhD, and Michał Pędziwiatr MD PhD, declare that we consent to the publication of our research study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pisarska-Adamczyk, M., Rzepa, A., Kapusta, M. et al. Is triggering receptor expressed on myeloid cell 1 (TREM-1) protein a new marker of serious infectious complications in colorectal surgery?: case-matched pilot study. Langenbecks Arch Surg 408, 368 (2023). https://doi.org/10.1007/s00423-023-03103-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03103-z