Abstract
Introduction
Metabolic/bariatric surgery is the only proven treatment for type 2 diabetes mellitus (T2D) with curative intent. However, in a number of patients, the surgery is not effective or they may experience a relapse. Those patients can be offered re-do bariatric surgery (RBS).
Purpose
The study aimed to determine factors increasing the odds for T2D remission one year after RBS following primary laparoscopic sleeve gastrectomy.
Methods
A multicenter retrospective cohort study was conducted between January 2010 and January 2020, which included 12 bariatric centers in Poland. The study population was divided into groups: Group 1- patients with T2D remission after RBS (n = 28) and Group 2- patients without T2D remission after RBS (n = 49). T2D remission was defined as HBA1c < 6.0% without glucose-lowering pharmacotherapy and glycemia within normal range at time of follow-up that was completed 12 months after RBS.
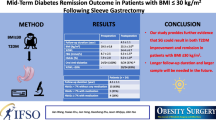
Results
Fifty seven females and 20 males were included in the study. Patients who achieved BMI < 33 kg/m2 after RBS and those with %EBMIL > 60.7% had an increased chance of T2D remission (OR = 3.39, 95%CI = 1.28–8.95, p = 0.014 and OR = 12.48, 95%CI 2.67–58.42, p = 0.001, respectively). Time interval between primary LSG and RBS was significantly shorter in Group 1 than in Group 2 [1 (1–4) vs. 3 (2–4) years, p = 0.023].
Conclusions
Shorter time interval between LSG and RBS may ease remission of T2D in case of lack of remission after primary procedure. Significant excess weight loss seems to be the most crucial factor for T2D remission.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An excessive accumulation of adipose tissue in the body adversely affects glucose metabolism. It may lead to the development of type 2 diabetes mellitus (T2D), hypertension, and dyslipidemia which are components of metabolic syndrome [1, 2]. Metabolic surgery has replaced the term ‘bariatric surgery’ because the surgical approach is not only targeted at excess weight, but also to primarily treat type 2 diabetes (T2D) and metabolic disease [3]. Metabolic/ bariatric surgery is currently the most effective and long-lasting treatment for severe obesity [4,5,6,7]. It has a proven curative effect on T2D which cannot be achieved with pharmacological therapy [4, 7, 8]. Metabolic surgery has been shown to bring complete long-term remission of T2D and can also prevent the development of T2D. Despite its efficacy, some patients will not achieve complete remission after surgery or may experience a recurrence in a long-term follow-up. In that case, a re-do bariatric surgery (RBS) can be a viable alternative to conservative management. There is a growing number of RBS performed worldwide and in some countries, it has become the third most commonly performed bariatric procedure [9, 10]. Also in Poland their number is continuously growing [11,12,13]. We still lack research on the factors that are increasing odds for T2D remission one-year after RBS, following laparoscopic sleeve gastrectomy (LSG) as the primary bariatric procedure [9, 10].
Purpose
The aim of this study is to determine which factors are increasing the odds for T2D remission one-year after RBS following primary LSG.
Materials and methods
Methods
A retrospective cohort study was conducted. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Patients with T2D undergoing RBS after LSG between January 2010 and January 2020 were included. An electronic database was created including patients from 12 Polish bariatric centers that entered voluntarily Polish Revision Obesity Surgery Study (PROSS) (ClinicalTrials.gov Identifier: NCT05108532). Inclusion criteria were as follow:
-
age ≥ 18 years
-
presence of T2D before RBS
-
complete 1-year follow-up with assessment of type 2 diabetes mellitus remission.
Patients with incomplete data were excluded from the study. Each participating bariatric center provided specific data, which were processed and used in the overall analysis.
T2D remission definition was based on guidelines of American Diabetes Association (ADA), that is HBA1c < 6.0% without glucose-lowering pharmacotherapy and fasting glycemia within normal range [14, 15].
Re-do bariatric surgery was defined as revision of a bariatric procedure due to inadequate weight loss or postoperative weight regain; inadequate improvement or frank recurrence of a weight-related comorbidity such as type 2 diabetes; or complications related to the primary bariatric surgery [16].
The study population was divided into two groups: Group 1 – patients with T2D remission after RBS and Group 2 – patients without T2D remission.
Each patient was qualified for surgical treatment in accordance with The Polish Guidelines for Metabolic and Bariatric Surgery [17]. All surgical procedures were performed laparoscopically in all centers [18,19,20].
Perioperative morbidity of re-do bariatric surgery was defined as any deviation from the standard perioperative course after RBS that required additional management within 30 days after the procedure (early morbidity), while postoperative morbidity was defined as morbidity that occurred over 30 days after RBS within the first year after RBS (late morbidity) [21]. Insufficient weight loss at participating centers was defined as achieving less than 50% EBMIL at 12 months after primary bariatric surgery. Weight regain is defined as progressive weight regain that occurs after achievement of an initial successful weight loss (defined as EBMIL > 50%) [22].
The study was designed and described according to the STROBE guidelines for observational studies [23]. The work has been reported in line with the STROCSS criteria [21].
Surgical technique
Types of RBS in our study included: re-sleeve gastrectomy (re-SG), revisional single anastomosis sleeve ileal bypass (SASI), revisional Roux-en-Y gastric bypass (RYGB) and revisional one-anastomosis gastric bypass (OAGB).
Re-SG began with mobilization of entire sleeve from the adhesions after primary SG. A 35 F gastric tube was guided along the lesser curvature of the stomach and passed distal to the pylorus. Stapling and division was done starting 6 cm proximal to the pylorus i.e. opposite to the incisura angularis of stomach. It was done with either 4.1 or 4.2 mm cartridges (length 60 mm) depending on the thickness of stomach assessed by operator. Staple line ended at the level of left crus of diaphragm. Staple line was not routinely oversewn, treated more likely as hemostatic measure if needed.
In case of SASI, the ileocecal region was identified and a 300 cm ileal loop was measured proximally. When the pylorus and ileal loop were positioned properly a linear 45-mm stapler was used to create a sleeve ileal side-to-side anastomosis, 6 cm proximally from the pylorus. The stapler defect was closed with a running suture.
During conversion from SG to RYGB, the sleeve was typically divided just distal to the left gastric artery. Gastric pouch was created with use of linear staplers (60 mm in length). Gastric tube was 35 F for calibration. Excess gastric tissue was excised if gastric sleeve was dilated. The gastric pouch was a standard 50 ml volume. The biliopancreatic limb was 100 cm, and the Roux limb was measured for 200 cm. Gastrojejunostomy and jejunojejunostomy were performed with a linear stapled technique and wall defects were closed with running sutures. The Roux limb were ante-colic in our practice. Mesenteric defects were not routinely closed. Decision was based on operator’s practice.
During OAGB the gastric pouch was calibrated (35 F) and crafted using a linear stapler. Gastric transection was performed at the incisura angularis of the lesser curvature. In case of gastric dilatation, the excision of the excess gastric tissue was performed due to the absence of vascularization on the large curvature. The jejunal loop was lifted in an antecolic position. The length of bilopancreatic limb was 150 cm from the ligament of Treitz. Posterolateral gastrojejunostomy was performed with a linear stapler followed by continuous sewing of the staple aperture.
Statistical analysis
Calculations were performed using STATISTICA 13.3 PL software (Tibco, CA, USA). Continuous values were presented as means with standard deviations, or medians with interquartile ranges when appropriate. Qualitative variables were compared using the Pearson χ-square with or without Yates’ correction. All available variables were analyzed in logistic regression models. P-values ≤ 0.05 were considered statistically significant.
Results
Patients flow through the study is shown in Fig. 1. As presented in Fig. 1, 28% of 132 (37) had T2D remission after primary bariatric surgery. After RBS the T2D recurrence was observed in 1 patient, 19/37 sustained remission, while 17/37 patients were lost to follow-up. 57 females and 20 males were included in the study. Mean age was 51.0 ± 9.9 years. 28 patients (36.4%) had remission of T2D after RBS and were included in group 1, while 49 patients did not have remission of T2D and were analyzed in group 2.
Table 1 demonstrates general characteristics of the study groups prior to the LSG. Patients did not differ in terms of gender (p = 0.351), age (p = 0.358), maximal preoperative BMI (p = 0.312). 75% of patients in group 1 were treated with oral anti-diabetic medications, as compared to 63.4% in Group 2 (p = 0.793). Insulin injections were administered in 27.8% of patients from Group 1 and 26.5% of Group 2 (p = 0.558).
Table 2 shows weight loss outcomes after the primary bariatric procedure and reasons for revisional procedure. Median lowest BMI after primary LSG in Group 1 was 36.4 (34.0–42.1) kg/m2, while in Group 2 – 37.0 (32.8–39.9), (p = 0.941). Maximal BMI loss (p = 0.412) and %EBMIL (p = 0.388) did not significantly differ between groups. Time interval between primary LSG and RBS was significantly shorter in Group 1 than in Group 2 [1 (1–4) year vs. 3 (2–4) years, p = 0.023]. The most common reason for RBS in Group 1 was insufficient weight loss (< 50% EWL) or failure of remission of obesity related co-morbidities—15 patients (53.5%). While in the Group 2 it was weight regain (return to the original body weight after an initial successful weight loss)- 29 patients (59.2%). No significant differences in distributions were observed. Majority of patients in both groups had RBS performed in the same center as primary procedure (75% vs. 79.6%, p = 0.640). What is important, the median pre-RBS BMI was comparable in both groups, Group 1 – 42.1 (36.8–45.4) kg/m2 vs. Group 2 – 42.2 (37.0–46.6), p = 0.687, Table 2.
Table 3 presents 1-year follow-up results after RBS. There was 1 (3.6%)re-SG in Group 1, while 8 (16.3%) in Group 2. 1 SASIwas performed in first group (3.6%), while 3 (6.1%) in the second. RYGB was done in 4 (14.3%) in Group 1, while in 15 (30.6%) in Group 2. The most commonly performed procedure in both groups was OAGB, Group 1—22 (78.6%) cases, Group 2—23 (46.9%) cases.
Group 1 had significantly lower median BMI after RBS than Group 2 – 31.4 (28.1–36.4) vs. 35.5 (31.9–37.5) kg/m2, p = 0.024. Similarly, median %EBMIL – 73.8% (65.2%-83.5%) vs. 62.7% (50.2%-73.4%), p = 0.001, and median %EBMIL from BMI before RBS –53.7% (39.3%-71.3%) vs. 35.4% (20.9–56.3%), p = 0.022. Remission of hypertension was significantly more often observed in Group 1 than 2 (36.4% vs. 10.0%, p = 0.044). Perioperative and postoperative morbidity of RBS did not significantly differ between groups (p = 0.552). Changes in BMI in patients in both groups are presented in Fig. 2.
Morbidity of RBS one year after procedures did not differ groups significantly, 4 (14.3%) cases in Group 1 and 11 (22.5%) in Group 2 (p = 0.552). Morbidity in Group 1 included – 1 case of anemia and nutrition deficiencies; 2 cases of gastrointestinal leakage; 1 case of persistent vomiting and GERD. Morbidity in Group 2 was: 2 cases of renal failure requiring dialysis; 3 cases of anemia; 1 case of small intestine perforation,; 2 cases of severe GERD with esophagitis; 1 case of dysphagia; 1 case of surgical site infection and 1 case of Petersen's space hernia.
Table 4 shows results of univariate logistic regression model of all available factors potentially influencing remission of T2D after RBS. BMI after RBS and %EBMIL had significant influence on OR of T2D remission. Due to the fact that these variables are related, a multivariate regression was not possible. Next, the ROC curve analyses were performed. Significant cut-off point for BMI was set at 33 kg/m2 (AUC 0.66, 95%CI 0.53–0.78, p = 0.017), while for %EBMIL at 60.7% (AUC 0.72, 95%CI 0.61–0.84, p < 0.001). BMI after RBS lower than 33 kg/m2 resulted in 3.39 times higher odds ratio for T2D remission (95%CI 1.28–8.95, p = 0.014). %EBMIL greater than 60.7% resulted in 12.48 times higher OR for T2D remission (95%CI 2.67–58.42, p = 0.001).
Table 5 set together rates of T2D remission after separately presented RBS depending of year, when RBS were performed.
Discussion
There is a scarcity of research analyzing the factors that are increasing odds for T2D remission after RBS following insufficient metabolic outcome of primary LSG. Our retrospective cohort study aimed to analyze factors significantly increasing odds for T2D remission after RBS following primary LSG. The first finding was that time interval between primary LSG and RBS was significantly shorter in group with remission of T2D than in the group without remission. Median time interval was 1 (1–4) year in the group with remission vs. 3 (2–4) years in group without remission. Moreover, out of all factors potentially contributing to remission of T2D the only and significant was weight loss. BMI after RBS lower than 33 kg/m2 resulted in 3.39 times higher odds ratio for T2D remission, while %EBMIL greater than 60.7% resulted in 12.48 times higher OR for T2D remission.
In the STAMPEDE trial, one of the largest trials which enrolled 150 patients, the complete diabetes remission (glycated hemoglobin [HbA1c] < 6.0% without any medication) was observed in 42% patients one year after laparoscopic Roux-en-Y gastric bypass (LRYGB) and 27% after LSG [24]. At 3 years, 35% of LRYGB and 20% of LSG patients maintained diabetes remission [22].
21 LRYGB and 13 LSG patients that initially achieved remission after one year, 38% and 46% of them had recurrence of the disease after 3 years, despite only mild weight regain. Similar numbers were observed in patients flow through our study. Out of 132 patients after LSG with T2D initially, 28% had diabetes remission after primary bariatric surgery (PBS). After re-do surgery T2D recurrence was observed in 1 patient, other 19 sustained remission, and 17 patients were lost to follow-up.
However, based on recent published works, LSG does not appear to be significantly inferior to LRYGB at medium-term follow-up. This is reflected in some guidelines that are equating LSG and LRYGB in terms of metabolic outcomes [23, 24].
In our study, we analyzed 77 patients without remission of T2D after primary bariatric surgery. 36.4% of patients achieved remission after RBS at one-year follow-up. T2D remission rates after RBS performed after LSG varies between 11 and 67% [25,26,27,28,29,30,31,32]. In 7 studies that reported conversion of LSG to LRYGB 37 patients (18%) had residual diabetes prior to conversion. Reoperation added 9–26% of decrease in BMI, and improved T2D in 62% of patients [25,26,27,28,29,30,31,32]. Another 3 papers reported conversion to duodenal switch that added 26–30% BMI loss of pre-revision BMI, and 79% of the 17 patients had improvement of their T2D [27, 33, 34].
Indications for re-do surgery after LSG include predominantly weight regain, insufficient weight loss or control of obesity-related comorbidities, sleeve stenosis, and gastroesophageal reflux disease. Regardless of chosen option, the time for RBS seems significant. Shorter time intervals between primary and re-do surgery were observed more often in patients with remission of T2D after RBS in our cohort. However, that was insignificant factor for OR of DM2 remission in univariate logistic regression model. We did not found rationale for performing RBS earlier, but data in literature suggest strongly, that duration of T2D is the most probable, independent preoperative predictor of early diabetes relapse either no remission in patients with T2D undergoing metabolic surgery [35].
RBS options are re-sleeve gastrectomy or conversion to either LRYGB, SADI, SASI, OAGB or duodenal switch. Regretfully we failed to find literature providing comparison of those approaches and results in T2D remission after re-do surgeries. Similarly, factors that promote remission of T2D. Neverthless, the literature shows that even modest weight loss of 5–10% can significantly improve metabolic profile [35,36,37,38]. Meta-analysis on converting SG, laparoscopic adjustable gastric banding, and vertical banding gastroplasty to OAGB provided data on the effects of conversion on T2D with a range of remission up to 65–78% during the first 5 years [39]. Meta-analysis by Jie et al. investigated revisions after vertical banded gastroplasty in 462 (29.0%) patients, adjustable gastric banding in 434 (27.2%) patients, and SG in 432 (27.1%) patients [40]. Ninety-two percent of patients achieved improvement of T2D following revisional surgery. In subgroup analysis by type of RBS, similar rates of improvement were seen after rSG (98%) and RYGB (94%). For remission rates however, RYGB (62%) performed significantly better than r-SG (33%). Many postulate that the malabsorptive function of duodenal exclusion and benefits of gut hormones changes in small intestine bypasses are reason for that those should be chosen for RBS [41]. Another single center studies provide remission rates of T2D after RBS of SG as follows: 100% SASI, 85–100% after revisional OAGB, 60% after revisional RYGB, 88% after SADI [42,43,44,45]. Still, we lack firm evidence for procedure of choice in case of SG cases that need RBS for curative effect on T2D, what causes, that further research in this field is needed.
Limitations
Study has limitations typical for a multicenter retrospective cohort studies. Another limitation is the definition for T2D remission that may vary between guidelines of bariatric and/or diabetologists associations and may cause difficulties to compare our results with other studies. Changes in overall treatment and procedure selection during 10-years study period in 12 centers are inevitably adding bias to study results. Also, the loss to follow-up at one-year in study group (18 patients) seems to be high. Variability of revisional procedures is adding bias, thus, the interpretation of the results must be done very carefully. Regretfully, the duration of T2D and its complications were not recorded in registry and registered follow-up in the participating centers that was accessible for investigation was 12 months after RBS.
Conclusions
Shorter time interval between LSG and RBS is associated with increased odds for remission of T2D after revisional procedure. Significant loss of excess weight seems to be the most crucial factor for T2D remission.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Després J-P, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444:881–887. https://doi.org/10.1038/nature05488
Engin A (2017) The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol 960:1–17. https://doi.org/10.1007/978-3-319-48382-5_1
Wilson R, Aminian A, Tahrani AA (2021) Metabolic surgery: a clinical update. Diabetes Obes Metab 23(Suppl 1):63–83. https://doi.org/10.1111/dom.14235
Schauer PR, Burguera B, Ikramuddin S et al (2004) Effect of laparoscopic Roux-en-Y gastric bypass on type 2 diabetes mellitus. Nutr Clin Pract 19:60–61. https://doi.org/10.1177/011542650401900160
Adams TD, Davidson LE, Litwin SE et al (2017) Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med 377:1143–1155. https://doi.org/10.1056/NEJMoa1700459
Gloy VL, Briel M, Bhatt DL et al (2013) Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ 347:f5934. https://doi.org/10.1136/bmj.f5934
Aleassa EM, Hassan M, Hayes K et al (2019) Effect of revisional bariatric surgery on type 2 diabetes mellitus. Surg Endosc 33:2642–2648. https://doi.org/10.1007/s00464-018-6541-1
Affinati AH, Esfandiari NH, Oral EA, Kraftson AT (2019) Bariatric surgery in the treatment of type 2 diabetes. Curr Diab Rep 19:156. https://doi.org/10.1007/s11892-019-1269-4
Clapp B, Harper B, Dodoo C et al (2020) Trends in revisional bariatric surgery using the MBSAQIP database 2015–2017. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 16:908–915. https://doi.org/10.1016/j.soard.2020.03.002
Małczak P, Pisarska-Adamczyk M, Zarzycki P et al (2021) Hiatal Hernia repair during laparoscopic sleeve gastrectomy: systematic review and meta-analysis on gastroesophageal reflux disease symptoms changes. Pol Przegl Chir 93:1–5. https://doi.org/10.5604/01.3001.0014.9356
Migaczewski M, Czerwińska A, Rubinkiewicz M et al (2021) The prevalence of, and risk factors for, Barrett’s oesophagus after sleeve gastrectomy. Videosurgery Other Miniinvasive Tech 16:710–714. https://doi.org/10.5114/wiitm.2021.107776
Nurczyk K, Chan C-E, Skoczylas T, Wallner G (2021) Follow-up after bariatric surgery: are we effective enough? Videosurgery Other Miniinvasive Tech i inne Tech małoinwazyjne. https://doi.org/10.5114/wiitm.2021.110411
Major P, Wysocki M, Dworak J et al (2017) Are bariatric operations performed by residents safe and efficient? Surg Obes Relat Dis 13:614–621. https://doi.org/10.1016/j.soard.2016.11.017
Buse JB, Caprio S, Cefalu WT et al (2009) How do we define cure of diabetes? Diabetes Care 32:2133–2135. https://doi.org/10.2337/dc09-9036
Draznin B, Aroda VR, Bakris G et al (2022) 16. Diabetes care in the hospital: standards of medical care in diabetes-2022. Diabetes Care 45:S244–S253. https://doi.org/10.2337/dc22-S016
Mirkin K, Alli VV, Rogers AM (2021) Revisional bariatric surgery. Surg Clin North Am 101:213–222. https://doi.org/10.1016/j.suc.2020.12.008
Budzyński A, Major P, Głuszek S et al (2016) Polskie rekomendacje w zakresie chirurgii bariatrycznej i metabolicznej. Med Prakt – Chir 6:13–25
Malczak P, Pisarska M, Piotr M et al (2017) Enhanced recovery after bariatric surgery: systematic review and meta-analysis. Obes Surg 27:226–235. https://doi.org/10.1007/s11695-016-2438-z
Sinha A, Jayaraman L, Punhani D, Chowbey P (2017) Enhanced recovery after bariatric surgery in the severely obese, morbidly obese, super-morbidly obese and super-super morbidly obese using evidence-based clinical pathways: a comparative study. Obes Surg 27:560–568. https://doi.org/10.1007/s11695-016-2366-y
Szeliga J, Wyleżoł M, Major P et al (2020) Metabolic and bariatric surgery chapter of the association of polish surgeons. Bariatric and metabolic surgery care standards. Videosurg Miniinvasive Tech 15:391–394. https://doi.org/10.5114/wiitm.2020.97935
Brethauer SA, Kim J, el Chaar M et al (2015) Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 11:489–506. https://doi.org/10.1016/j.soard.2015.02.003
Nedelcu M, Khwaja HA, Rogula TG (2016) Weight regain after bariatric surgery-how should it be defined? Surg Obes Relat Dis Off J Am Soc Bariatr Surg 12:1129–1130. https://doi.org/10.1016/j.soard.2016.04.028
von Elm E, Altman DG, Egger M et al (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int J Surg. https://doi.org/10.1016/j.ijsu.2014.07.013
Schauer PR, Bhatt DL, Kirwan JP et al (2014) Bariatric surgery versus intensive medical therapy for diabetes–3-year outcomes. N Engl J Med 370:2002–2013. https://doi.org/10.1056/NEJMoa1401329
Salminen P, Helmiö M, Ovaska J et al (2018) Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: The SLEEVEPASS randomized clinical trial. JAMA 319:241–254. https://doi.org/10.1001/jama.2017.20313
Schauer PR, Bhatt DL, Kirwan JP et al (2017) Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med 376:641–651. https://doi.org/10.1056/NEJMoa1600869
van Rutte PWJ, Smulders JF, de Zoete JP, Nienhuijs SW (2012) Indications and short-term outcomes of revisional surgery after failed or complicated sleeve gastrectomy. Obes Surg 22:1903–1908. https://doi.org/10.1007/s11695-012-0774-1
Gautier T, Sarcher T, Contival N et al (2013) Indications and mid-term results of conversion from sleeve gastrectomy to Roux-en-Y gastric bypass. Obes Surg 23:212–215. https://doi.org/10.1007/s11695-012-0782-1
Carmeli I, Golomb I, Sadot E et al (2015) Laparoscopic conversion of sleeve gastrectomy to a biliopancreatic diversion with duodenal switch or a Roux-en-Y gastric bypass due to weight loss failure: our algorithm. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 11:79–85. https://doi.org/10.1016/j.soard.2014.04.012
Pok E-H, Lee W-J, Ser K-H et al (2016) Laparoscopic sleeve gastrectomy in Asia: long term outcome and revisional surgery. Asian J Surg 39:21–28. https://doi.org/10.1016/j.asjsur.2015.03.006
Poghosyan T, Lazzati A, Moszkowicz D et al (2016) Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass: an audit of 34 patients. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 12:1646–1651. https://doi.org/10.1016/j.soard.2016.02.039
Stenard F, Iannelli A (2015) Laparoscopic sleeve gastrectomy and gastroesophageal reflux. World J Gastroenterol 21:10348–10357
Iannelli A, Debs T, Martini F et al (2016) Laparoscopic conversion of sleeve gastrectomy to Roux-en-Y gastric bypass: indications and preliminary results. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 12:1533–1538. https://doi.org/10.1016/j.soard.2016.04.008
Casillas RA, Um SS, Zelada Getty JL et al (2016) Revision of primary sleeve gastrectomy to Roux-en-Y gastric bypass: indications and outcomes from a high-volume center. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 12:1817–1825. https://doi.org/10.1016/j.soard.2016.09.038
Nautiyal HK, Guan W, Lin S, Liang H (2020) Preoperative predictors of early relapse/no-remission of type-2 diabetes after metabolic surgery in Chinese patients. Clin Obes 10:e12350. https://doi.org/10.1111/cob.12350
Dapri G, Cadière GB, Himpens J (2011) Superobese and super-superobese patients: 2-step laparoscopic duodenal switch. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 7:703–708. https://doi.org/10.1016/j.soard.2011.09.007
Iannelli A, Schneck A-S, Topart P et al (2013) Laparoscopic sleeve gastrectomy followed by duodenal switch in selected patients versus single-stage duodenal switch for superobesity: case-control study. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 9:531–538. https://doi.org/10.1016/j.soard.2012.02.003
Wing RR (2010) Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med 170:1566–1575. https://doi.org/10.1001/archinternmed.2010.334
Kermansaravi M, Shahmiri SS, DavarpanahJazi AH et al (2021) One Anastomosis/Mini-Gastric Bypass (OAGB/MGB) as revisional surgery following primary restrictive bariatric procedures: a systematic review and meta-analysis. Obes Surg 31:370–383. https://doi.org/10.1007/s11695-020-05079-x
Koh ZJ, Chew CAZ, Zhang JJY et al (2020) Metabolic outcomes after revisional bariatric surgery: a systematic review and meta-analysis. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 16:1442–1454. https://doi.org/10.1016/j.soard.2020.05.029
Gagner M (2020) Hypoabsorptive surgery is the best revisional strategy for metabolic and diabetes outcomes. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 16:1454–1455
Sewefy AM, Atyia AM, Kayed TH, Hamza HM (2022) Single-anastomosis sleeve Jejunal (SAS-J) bypass as revisional surgery after primary restrictive bariatric procedures. Obes Surg 32:2807–2813. https://doi.org/10.1007/s11695-022-06123-8
Osorio J, Lazzara C, Admella V et al (2021) Revisional laparoscopic SADI-S vs. duodenal switch following failed primary sleeve gastrectomy: a single-center comparison of 101 consecutive cases. Obes Surg 31:3667–3674. https://doi.org/10.1007/s11695-021-05469-9
Chiappetta S, Stier C, Scheffel O et al (2019) Mini/One anastomosis gastric bypass versus Roux-en-Y gastric bypass as a second step procedure after sleeve gastrectomy-a retrospective cohort study. Obes Surg 29:819–827. https://doi.org/10.1007/s11695-018-03629-y
Musella M, Bruni V, Greco F et al (2019) Conversion from laparoscopic adjustable gastric banding (LAGB) and laparoscopic sleeve gastrectomy (LSG) to one anastomosis gastric bypass (OAGB): preliminary data from a multicenter retrospective study. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 15:1332–1339. https://doi.org/10.1016/j.soard.2019.05.026
Acknowledgements
We thank to all PROSS- Collaborative Study Group members (Piotr Major1, Michał Pędziwiatr1, Justyna Rymarowicz1, Piotr Zarzycki1, Tomasz Stefura1, Karol Ciszek1, Piotr Myśliwiec2, Hady Razak Hady2, Paulina Głuszyńska2, Monika Proczko-Stepaniak3, Michał Szymański3, Maciej Walędziak4, Michał Janik4, Andrzej Kwiatkowski4, Magdalena Materlak4, Katarzyna Bartosiak4, Łukasz Czyżykowski4, Maciej Mawlichanów4, Piotr Kowalewski4, Jacek Szeliga5, Wojciech Kupczyk5, Natalia Dowgiałło-Gornowicz6, Paweł Lech6, Anna Harań6, Grzegorz Kowalski7, Rafał Mulek8, Michał Kreft8, Michał Wysocki9, Michał Orłowski10 Paula Franczak10, Artur Binda11, Wiesław Tarnowski11, Paweł Jaworski11, Katarzyna Bartosiak4, Mateusz Kamiński12, Maciej Pastuszka13, Wojciech Lisik14, Paweł Szymański15, Bartosz Katkowski15, Michał Leśniak15) for their contribution to this article.
12nd Department of General Surgery, Jagiellonian University Medical College, Cracow, Poland
21 Department of General and Endocrinological Surgery, Medical University of Bialystok, Bialystok, Poland
3Department of General, Endocrine and Transplant Surgery, Medical University of Gdansk, Gdansk, Poland
4Department of General, Oncological, Metabolic and Thoracic Surgery, Military Institute of Medicine, Warsaw, Poland
5Department of General, Gastroenterological, and Oncological Surgery, Collegium Medicum Nicolaus Copernicus University, Torun, Poland
6Department of General, Minimally Invasive and Elderly Surgery, University of Warmia and Mazury in Olsztyn, Poland
7Surgery Clinic Mazan, Katowice, Poland
8Department of general and endoscopic surgery, EuroMediCare Specialist Hospital and Clinic in Wroclaw, Poland
9Department of General Surgery and Surgical Oncology, Ludwik Rydygier Memorial Hospital, Cracow, Poland
10Department of General and Oncological Surgery, Ceynowa Hospital, Poland
11Centre of Postgraduate Medical Education. Orlowski Hospital, Poland
12Department of General, Transplant, Gastroenterological and Oncological Surgery, Medical University of Lodz, Poland
13Department of General and Minimally Invasive Surgery, Łęczna, Poland
14Department of General and Transplantation Surgery, Medical University of Warsaw, Warsaw, Poland
15Department of General and Vascular Surgery, Polanica Zdrój, Poland
Author information
Authors and Affiliations
Consortia
Contributions
Michał Wysocki: study design, data collections, data analysis, writing, final approval of manuscript, Karol Ciszek: data collections, data analysis, writing, final approval of manuscript, Justyna Rymarowicz: data collections, data analysis, writing, final approval of manuscript, Piotr Zarzycki: data collections, data analysis, writing, final approval of manuscript, Maciej Walędziak: data collections, data analysis, writing, final approval of manuscript, Katarzyna Bartosiak: data collections, data analysis, writing, final approval of manuscript, Paweł Jaworski: data collections, data analysis, writing, final approval of manuscript, Wojciech Kupczyk: data collections, data analysis, writing, final approval of manuscript, Jacek Szeliga: data collections, data analysis, writing, final approval of manuscript, Wiesław Tarnowski: data collections, data analysis, writing, final approval of manuscript, Magdalena Pisarska-Adamczyk: data collections, data analysis, writing, final approval of manuscript, Piotr Małczak: data collections, data analysis, writing, final approval of manuscript, Michał Pędziwiatr: data collections, data analysis, writing, final approval of manuscript, Piotr Major: study design, data collections, data analysis, writing, final approval of manuscript.
Corresponding author
Ethics declarations
Ethics statement
All procedures performed in the study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments. Informed consent for surgical treatment was obtained from all individual participants included in the study. The study was approved by the Bioethics Committee of the Regional Chamber of Physicians.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wysocki, M., Ciszek, K., Rymarowicz, J. et al. The analysis of factors increasing the odds for type 2 diabetes mellitus remission following re-do bariatric surgery after laparoscopic sleeve gastrectomy- cohort study. Langenbecks Arch Surg 408, 371 (2023). https://doi.org/10.1007/s00423-023-03102-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03102-0