Abstract
Introduction
Bariatric surgery is an effective method of treating obesity, with gastric bypass and sleeve gastrectomy being the most common techniques used worldwide. Despite the technical challenges in these methods, little is known about the effects of summer closure on the incidence of serious postoperative complications in surgeries performed shortly after summer vacation. This has therefore been studied in our large cohort.
Materials and methods
A retrospective cohort study based on data from the Scandinavian Obesity Surgery Registry was conducted. Patients who underwent a primary gastric bypass or sleeve gastrectomy operation between 2010 and 2019 were included. The rate of serious complications within 30 days after surgery for patients who underwent surgery the first month after summer closure was compared to those who underwent surgery during the rest of the year using the χ2 test and adjusted logistic regression.
Results
The study included 42,404 patients, 36,094 of whom underwent gastric bypass and 6310 of whom received sleeve gastrectomy. Summer closure was associated with an increased risk for serious postoperative complications in gastric bypass surgery (adjusted odds ratio (adj-OR) = 1.17; 95% confidence interval (CI): 1.01–1.36). No statistically significant association was seen for sleeve gastrectomy (adj-OR = 1.17; 95% CI: 0.72–1.91), nor in overall complication rate.
Conclusions
Summer closure increases the risk of serious postoperative complications in gastric bypass surgery. No statistically significant association was found for sleeve gastrectomy surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery is currently the most effective treatment for obesity, resulting in long-term weight reduction and the resolution of metabolic comorbidities for many patients [1, 2], with Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) being the most common types of bariatric surgical procedures performed worldwide [3].
As with any type of surgery, bariatric surgery entails a risk of postoperative complications. Although the introduction of the laparoscopic technique has reduced the overall complication rate, the patient is still at risk of serious adverse postoperative events such as leakage, bleeding, or small bowel obstruction [4,5,6].
Several studies have investigated whether there is an association between the day, week, or season of surgery and outcomes. In a large cohort of patients, the mortality rate after surgery starting in the afternoon was higher than that after surgery starting in the morning, regardless of the surgical discipline and the urgency of the performed surgery. No difference in mortality between weekends and weekdays was found [7]. For bariatric surgery, seasonality in complications with an increased risk of sepsis and deep vein thrombosis (DVT) in the colder season compared to the summer season has been reported [8]. Higher complication rates during the first weeks when restarting bariatric surgery after summer vacation have been observed as a personal experience, but to the best of our knowledge, the effect of summer closure of bariatric surgery centers on postoperative adverse events has not been studied previously.
Therefore, the aim of this study was to investigate whether there is an increased risk of serious postoperative complications within the 30-day postoperative period in patients who underwent RYGB or SG surgery during the start-up after summer closure.
Material and methods
This was a retrospective cohort study based on prospectively collected data extracted from the Scandinavian Obesity Surgery Registry (SOReg). The SOReg, established in 2007, is a national research and quality registry, where individual data for patients undergoing bariatric surgery are continuously collected as part of clinical practice [9]. All Swedish centers for bariatric surgery use the registry and a recent audit showed that it covers > 97% of all bariatric procedures in Sweden [10]. The SOReg contains patient demographic data, information on comorbid diseases (sleep apnea, hypertension, diabetes, dyslipidemia, dyspepsia, and depression), and perioperative and postoperative data [10]. Comorbidities are defined as a specified condition requiring pharmacological treatment or treatment with positive airway pressure (sleep apnea) [9]
During the study period, the majority of bariatric surgical procedures were performed within the public healthcare system, financed by public means. The majority of operations were performed by specialists in bariatric surgery or specialists in upper GI surgery under direct supervision of a bariatric surgeon. Most healthcare providers working in the publicly funded healthcare sector go on vacation for at least 4 weeks during summer.
Patients who underwent primary laparoscopic RYGB or SG surgery between 2010 and 2019 were eligible for inclusion in the study. For each facility having entered data in SOReg, it was investigated whether there was a gap of at least four consecutive weeks with no registered elective bariatric surgical procedure during the summer months of June through August. If a gap was not found, all patients who underwent surgery at that facility that year were excluded from the study. Patients who underwent surgery during the first 4 weeks after summer closure were compared to those who underwent surgery during the rest of the year.
Outcomes
The primary outcome was serious complications within 30 days of surgery. Secondary outcomes were duration of surgery, duration of postoperative hospital stay, readmission, and the occurrence of specified postoperative complications (leak, bleeding, abscess, small bowel obstruction, DVT, pulmonary complication, cardiovascular complication, wound complication, stricture, marginal ulcer, urinary tract infection).
Definitions
Postoperative complications were graded according to the Clavien-Dindo classification system [11]. A complication graded as Clavien-Dindo score ≥ 3b, i.e., a complication requiring intervention under general anesthesia, resulting in single or multiorgan failure, or death, was considered a serious postoperative complication [11]. Annual surgical volume at each center was classified as low-volume (< 100 bariatric surgical operations/year), mid-volume (100–249 operations/year), and high-volume (≥ 250 operations/year) [12].
Statistical analysis
Baseline characteristics were presented as means ± standard deviations or numbers (percentages) as appropriate with comparison across groups using the χ2 test for categorical variables and the t test of means for continuous variables. Outcomes were analyzed with stratification by surgical method. The χ2 test and adjusted logistic regression (adjusted for sex, age, BMI, comorbidities, concurrent surgery, and year of surgery) were performed for the primary outcome and all binary secondary outcomes. The duration of surgery was analyzed using unadjusted and adjusted linear regression (adjusted for sex, age, BMI, comorbidities, concurrent surgery, and year of surgery). Due to a nonnormal distribution, the duration of postoperative hospital stay was analyzed with the Mann–Whitney U test, and the effect size was calculated with eta squared. A value of p < 0.05 was considered to represent statistical significance. Relative risks (RRs), odds ratios (ORs), and beta values were calculated with a 95% confidence interval (CI). The analyses were considered exploratory and as such no adjustment for multiple comparisons was performed. Missing data was handled by listwise deletion. A post hoc sensitivity analysis was performed including patients lost to follow-up. In this analysis, logistic regression was run twice, once with a configuration assuming that all patients lost to follow-up had a serious complication and once assuming no patient had a serious complication. A further post hoc sensitivity analysis compared the first 4 weeks after summer with the remaining part of the year for patients operated at centers not closing during summer. IBM SPSS Statistics version 22 was used for all statistical analyses.
Results
During the study period, 61,786 patients were identified from the SOReg. Of these, 17,683 did not meet the inclusion criteria because the surgery center did not close during summer that year, and an additional 1699 (3.9%) patients were lost to follow-up at 30 days. Of the 42,404 remaining patients, 36,094 underwent RYGB surgery and 6310 underwent SG. Concerning hospital volume, 21%, 46%, and 33% of the operations were performed at low-, mid-, and high-volume centers.
In the RYGB group, 74.9% of patients were women and the mean age at surgery was 41.0 ± 11.3 years. Patients operated on after summer closure were more often women, who had slightly lower BMIs and less often had concurrent surgery. The corresponding figures for the SG group were 78.4% female patients and a mean age of 41.1 ± 11.1 years with statistically significant differences only in the concurrent surgery variable (Table 1).
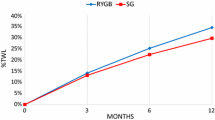
Postoperative complications occurred within 30 days of RYGB surgery in 469 (8.6%) patients during the start-up period after summer closure and in 2533 (8.3%) patients in the control group with 218 (4.0%) versus 1047 (3.4%) fulfilling the criteria for a serious postoperative complication. In the SG group, the overall complication rate was 61 (6.7%) in the group treated after summer closure and 305 (5.7%) in the reference group. The corresponding number of serious postoperative complications were 20 (2.2%) compared to 98 (1.8%) (Tables 2 and 3).
There was a significant increased risk of serious complications (RR = 1.17; 95% CI 1.01–1.35; p = 0.034) for patients who underwent RYGB surgery after summer closure, with similar results after adjustment for age, sex, BMI, comorbidities, and year of surgery (adj-OR = 1.17; 95% CI: 1.01–1.36; p = 0.034). The same tendency was seen irrespective of hospital volume. No difference in the risk for serious complications was seen after SG (RR = 1.21; 95% CI 0.75–1.94; p = 0.436; adj-OR = 1.17; 95% CI: 0.72–1.91; p = 0.519). However, there was an increased risk of deep venous thrombosis (DVT) in the summer closure group after SG surgery (adj-OR = 6.90; 95% CI 1.10–43.29; p = 0.039).
Having surgery after summer closure was associated with significantly shorter operative times for RYGB surgery (adjusted mean difference, − 2.1 min; 95% CI: − 3.0 to − 1.2; p < 0.001). There was also a shorter duration of postoperative hospital stay after both RYGB (mean ranks difference − 2.8; p = 0.05) and SG (mean rank difference − 2.0; p = 0.046) in the summer closure group. This would correspond to a measure of effect size for postoperative hospital stay of 0.02% for RYGB and 0.06% for SG.
The sensitivity analysis for RYGB patients was statistically significant regardless of whether all patients lost to follow-up were assumed to have had a serious complication or not. For SG, the analysis was still not statistically significant regardless of the configuration of missing data, that is, no serious complications or only serious complications (Supplementary Tables 1 and 2). No tendency towards increased complications was seen among patients operated after the summer period at centers not closing during summer (Supplementary Table 3).
Discussion
In the present study, we found that surgery center summer closure was associated with a higher risk of serious complications for patients who underwent laparoscopic RYGB surgery within the first month of start-up. This association remained significant when adjusting for other known risk factors.
Laparoscopic RYGB is a technically advanced procedure and it has been estimated that it takes approximately 100 operations to master the technique [13,14,15], with wide differences in technical skills between surgeons [16]. However, while many studies of the learning process have been conducted, studies regarding the decay of laparoscopic surgical skills are scarce. For laparoscopic nephrectomy and nephroureterectomy, the time interval between operations influences the outcome in low-volume hospitals. Using a shorter operative time as a measure of surgical skill, deterioration was seen after a 14-day interval between procedures [17]. Many studies investigating surgeons’ increasing proficiency have used decreasing duration of surgery as a measure thereof [13, 14, 18]. In the present study, we found that although the start-up period after summer closure was associated with a higher risk of serious postoperative complications, it was also associated with shorter operation time. Although the shorter operation time in part may be explained by the slightly higher number of concurrent operations in the control group, shorter operation times may therefore not always be proof of higher levels of skill. Sinha et al. found that for general surgery residents performing simulator training, good instrumentation and tissue handling techniques were associated with a more consistent deterioration after an interval of nonuse than the speed at which a task was completed. Adequate task performance was associated with both shorter and longer durations of task completion and the time taken to complete a task showed little association with passing or failing the task. Skills in complex tasks deteriorated more than skills in simple tasks. First-year residents were also more prone to skill decay than upper-level residents [19]. Since the decay of laparoscopic skills in experienced surgeons in high-volume surgery facilities seems almost unexplored, there is room for future research in this field. The technical skills may vary widely even for experienced surgeons and although a sensitivity analysis including hospital volume failed to show major differences in the effect of summer closure, individual surgeons may experience differences in decay from absence from surgery [16].
This study showed that in a large cohort of RYGB patients, the risk of serious complications increased by 17% after summer closure. Since this represents a small increase, starting from a low risk to begin with, having RYGB after the summer vacation may still be considered safe. Nevertheless, in continuous work to reduce complication rates and improve the quality of bariatric surgery, some possible approaches to moderate the effect of intervals of absence may be considered. First, the right type of patient should be selected for the first weeks after a period of absence when the risk of serious complications is slightly increased. Since some risk factors for postoperative complications are already known, it should be possible to select patients with fewer risk factors or to optimize these risk factors before surgery. Second, the surgeon should be teamed with an experienced assistant. Previous research has shown that less experienced first assistants in RYGB and SG surgery increase the 30-day readmission rate and the need for intensive care unit management [20]. Third, with today’s advancement in technology, a great deal of research has focused on the benefits of simulator training [21,22,23,24]. It has also been shown that such training is indeed transferable to the operating room [23, 25]. Again, most studies have been conducted on residents and non-experienced laparoscopic surgeons. Hence, it is still unclear whether experienced surgeons would benefit from such training.
In the present study, there was no statistically significant association between summer closure and an increased risk of serious postoperative complications in SG surgery. SG is often viewed as a less advanced procedure than RYGB [26], with slightly shorter learning curve [15], and skill may therefore not be as sensitive to periods of absence. Given that SG has gained ground only in recent years, it is possible that the SG population of this study was too small to attain the statistical power needed for significant results. However, the statistical analysis showed a higher risk of DVT after SG surgery in the summer closure group, which may indicate that SG is not completely insensitive to longer intervals of performed surgeries. While the relation to summer closure remains unclear, SG has been reported to induce a hypercoagulable state [27] as well as a reduced blood flow velocity [28] which may in part explain why an increased risk for this particular complication was seen after SG but not after RYGB, despite the higher overall complication rates after RYGB.
In addition to surgical factors, several important perioperative factors involving the process from preparation before surgery, through perioperative care to the early postoperative period, may also be influenced by summer closure. In Sweden, the adherence to fast-track protocols, such as that presented by the ERAS Society [29], is generally high, but summer closure could at least in theory influence adherence from patients as well as caregivers.
Despite the strengths of nearly complete national coverage, the results of this study must be viewed in light of its limitations. This was a retrospective cohort study based on registry data. Consequently, there may be variables of relevance that were not adequately recorded. One such variable is smoking, which was not a compulsory parameter in SOReg from the beginning. With our low prevalence of smoking (12%) [30], it is unlikely that the number of smokers differed enough between groups to confound the results. Socioeconomic status and surgeons’ experience have also been demonstrated to be relevant variables [15, 31]. Although it is also unlikely that these variables would differ throughout the year, adjusting for smoking, socioeconomic status, and surgeons’ experience as confounders would have been desirable. In the patient selection process, 1699 patients were excluded from the study due to a lack of 30-day follow-up. A comparison of baseline data of patients lost to follow-up and patients included in the study showed similar compositions of age, sex, and BMI in all groups. For both RYGB and SG patients, all comorbidities except depression were slightly less common among patients lost to follow-up. Despite these differences, the total study data loss was < 5%. The robustness of the results was nonetheless tested in a sensitivity analysis. This analysis did not change the statistical significance of the results. Furthermore, despite the lack of seasonal effect for patients operated at centers not closing during summer, we cannot totally exclude a seasonal effect. Finally, the Swedish healthcare system differs from that in other parts of the world, which may limit generalizability. However, the effects of closing during a period of at least 4 weeks are likely to be similar in other healthcare systems.
In conclusion, the results of this study indicate that having RYGB surgery during the start-up period after summer vacation is associated with an increased risk of serious postoperative complications compared to the corresponding risk posed by having this surgery during the rest of the year. No increased risk was found for SG surgery, or for overall complications in either procedure. More research is needed regarding the skill deterioration rate in experienced bariatric surgeons and whether they would benefit from preoperative simulator training after a period of absence. Such training might not completely counteract the effect of longer absences in bariatric surgery, but along with optimizing patient-specific risk factors and teaming up the surgeon with an experienced assistant, it may mitigate the effect of summer closure.
References
Peterli R, Wölnerhanssen BK, Peters T et al (2018) Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA 319(3):255–265
Sjöström L (2013) Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med 273(3):219–234
Angrisani L, Santonicola A, Iovino P et al (2018) IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg 28(12):3783–3794
Weller WE, Rosati C (2008) Comparing outcomes of laparoscopic versus open bariatric surgery. Ann Surg 248(1):10–15
Stenberg E, Szabo E, Agren G et al (2014) Early complications after laparoscopic gastric bypass surgery: results from the Scandinavian Obesity Surgery Registry. Ann Surg 260(6):1040–1047
Stroh C, Köckerling F, Volker L et al (2016) Results of more than 11,800 sleeve gastrectomies: data analysis of the German Bariatric Surgery Registry. Ann Surg 263(5):949–955
Kork F, Spies C, Conrad T et al (2018) Associations of postoperative mortality with the time of day, week and year. Anaesthesia 73(6):711–718
Hu Q, Shi L, Chen L et al (2018) Seasonality in the adverse outcomes in weight loss surgeries. Surg Obes Relat Dis 14(3):291–296
Hedenbro JL, Naslund E, Boman L et al (2015) Formation of the Scandinavian Obesity Surgery Registry. SOReg Obes Surg 25(10):1893–1900
Sundbom M, Näslund I, Näslund E, Ottosson J (2021) High acquisition rate and internal validity in the Scandinavian Obesity Surgery Registry. Surg Obes Relat Dis 17(3):606–614
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Birkmeyer NJ, Dimick JB, Share D et al (2010) Hospital complication rates with bariatric surgery in Michigan. JAMA 304(4):435–442
Søvik TT, Aasheim ET, Kristinsson J et al (2009) Establishing laparoscopic Roux-en-Y gastric bypass: perioperative outcome and characteristics of the learning curve. Obes Surg 19(2):158–165
Schauer P, Ikramuddin S, Hamad G, Gourash W (2003) The learning curve for laparoscopic Roux-en-Y gastric bypass is 100 cases. Surg Endosc 17(2):212–215
Wehrtmann FS, de la Garza JR, Kowalewski KF et al (2020) Learning curves of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy in bariatric surgery: a systematic review and introduction of a standardization. Obes Surg 30(2):640–656
Birkmeyer JD, Finks JF, O’Reilly A et al (2013) Surgical skill and complication rates after bariatric surgery. N Engl J Med 369(15):1434–1442
Sugihara T, Yasunaga H, Matsui H, Ishikawa A, Fujimura T, Fukuhara H, Fushimi K, Homma Y, Kume H (2018) A skill degradation in laparoscopic surgery after a long absence: assessment based on nephrectomy case. Mini-invasive Surg 2:11
Ballantyne GH, Ewing D, Capella RF et al (2005) The learning curve measured by operating times for laparoscopic and open gastric bypass: roles of surgeon’s experience, institutional experience, body mass index and fellowship training. Obes Surg 15(2):172–182
Sinha P, Hogle NJ, Fowler DL (2008) Do the laparoscopic skills of trainees deteriorate over time? Surg Endosc 22(9):2018–2025
Mahan ME, Parker DM, Fluck M, Gabrielsen JD, Petrick AT, Horsley RD (2019) First assistant impact on early morbidity and mortality in bariatric surgery. Surg Obes Relat Dis 15(9):1541–1547
Zendejas B, Cook DA, Bingener J et al (2011) Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair: a randomized controlled trial. Ann Surg 254(3):502–509 (discussion 509-511)
Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91(2):146–150
Palter VN, Grantcharov TP (2014) Individualized deliberate practice on a virtual reality simulator improves technical performance of surgical novices in the operating room: a randomized controlled trial. Ann Surg 259(3):443–448
Banks EH, Chudnoff S, Karmin I, Wang C, Pardanani S (2007) Does a surgical simulator improve resident operative performance of laparoscopic tubal ligation? Am J Obstet Gynecol 197(5):541.e541-545
Ahlberg G, Enochsson L, Gallagher AG et al (2007) Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg 193(6):797–804
Chung AY, Strassle PD, Schlottmann F, Patti MG, Duke MC, Farrell TM (2019) Trends in utilization and relative complication rates of bariatric procedures. J Gastrointest Surg 23(7):1362–1372
Liu C, Han Z, Zhang N et al (2020) Laparoscopic sleeve gastrectomy affects coagulation system of obese patients. Obes Surg 30(10):3989–3996
Osman AMA, Helmy AS, Mikhail S, AlAyat AA, Serour DK, Ibrahim MY (2021) Early effects of laparoscopic sleeve gastrectomy and laparoscopic one-anastomosis gastric bypass on portal venous flow: a prospective cohort study. Obes Surg 31(6):2410–2418
Stenberg E, Dos Reis Falcão LF, O’Kane M et al (2022) Guidelines for perioperative care in bariatric surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations: a 2021 update. World J Surg 46(4):729–751
Scandinativan Obesity Surgery Registry. Annual Report. Published 2020–05–10. Available at: www.ucr.uu.se/arsrapporter/arsrapporter Accessed 2021–08–11.
Stenberg E, Persson C, Näslund E et al (2019) The impact of socioeconomic factors on the early postoperative complication rate after laparoscopic gastric bypass surgery. Surg Obes Relat Dis 15(4):575–581
Funding
Open access funding provided by Örebro University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Swedish Ethical Review Authority on July 28th, 2020 (registration number 2020–02806), and follows the ethical standards of the 1964 Helsinki Declaration and its later amendments.
Consent to participate
Informed consent was obtained from all individual participants upon entry of their data into the Scandinavian Obesity Surgery Registry.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• After summer closure, gastric bypass was associated with 17% increased risk of serious complications.
• No increased risk was found in sleeve gastrectomy, nor in overall complication rate.
• Could further optimization of patient selection or surgical team be of value?
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fall, J., Sundbom, M. & Stenberg, E. The influence of summer closure on serious postoperative complications in bariatric surgery. Langenbecks Arch Surg 407, 2769–2775 (2022). https://doi.org/10.1007/s00423-022-02566-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02566-w