Abstract
Purpose
While its effect is controverted, multimodal pre-habilitation could be used to improve the postoperative course following colorectal cancer surgery. However, by increasing lean body mass, pre-habilitation could reduce the time needed to recover gastrointestinal (GI) functions. The aim was to assess the impact of pre-habilitation before colorectal cancer surgery on postoperative GI motility recovery.
Methods
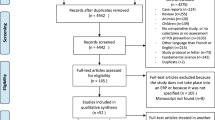
This is a matched retrospective study based on a prospective database including patients undergoing colorectal surgery without pre-habilitation (NPH) (2016–2018) and with pre-habilitation (PH group) (2018–2019). The main outcome measure was the time to GI-3 recovery (tolerance to solid food and flatus and/or stools).
Results
One hundred thirteen patients were included, 37 underwent pre-habilitation (32.7%). The patient’s age, the surgical procedure, the surgical access, the rate of synchronous metastasis, the rate of preoperative chemoradiotherapy, and the rate of stoma were more important in the PH group. Conversely, the rate of patients with an ASA score of > 2 was higher in the NPH group. By matching patients according to age, gender and surgical procedure, 84 patients were compared (61 in the NPH group and 23 in the PH group). The mean of GI-3 recovery was significantly lower in the PH group. The other endpoints were not significantly different but time to GI function recovery and medical morbidity tended to be higher in the NPH group. Compliance with the enhanced recovery program was significantly higher in the PH group.
Conclusion
Pre-habilitation before colorectal cancer surgery reduced time to GI function recovery and may increase compliance with the enhanced recovery program.

Similar content being viewed by others
Data availability
None.
References
Okugawa Y, Toiyama Y, Oki S et al (2018) Feasibility of assessing prognostic nutrition index in patients with rectal cancer who receive preoperative chemoradiotherapy. J Parenter Enteral Nutr 42:998–1007
Clark ST, Malietzis G, Grove TN et al (2020) The emerging role of sarcopenia as a prognostic indicator in patients undergoing abdominal wall hernia repairs: a systematic review of the literature. Hernia 24:1361–1370
Huang D-D, Wang S-L, Zhuang C-L et al (2015) Sarcopenia, as defined by low muscle mass, strength and physical performance, predicts complications after surgery for colorectal cancer. Colorectal Dis 17:O256-264
Schaffler-Schaden D, Mittermair C, Birsak T et al (2020) Skeletal muscle index is an independent predictor of early recurrence in non-obese colon cancer patients. Langenbecks Arch Surg 405:469–477
Dolan DR, Knight KA, Maguire S, Moug SJ (2019) The relationship between sarcopenia and survival at 1 year in patients having elective colorectal cancer surgery. Tech Coloproctol 23:877–885
Bruns ERJ, Argillander TE, Van Den Heuvel B et al (2018) Oral nutrition as a form of pre-operative enhancement in patients undergoing surgery for colorectal cancer: a systematic review. Surg Infect 19:1–10
Trépanier M, Minnella EM, Paradis T et al (2019) Improved disease-free survival after prehabilitation for colorectal cancer surgery. Ann Surg 270:493–501
Piraux E, Caty G, Reychler G (2018) Effects of preoperative combined aerobic and resistance exercise training in cancer patients undergoing tumour resection surgery: A systematic review of randomised trials. Surg Oncol 27:584–594
Gillis C, Fenton TR, Sajobi TT et al (2019) Trimodal prehabilitation for colorectal surgery attenuates post-surgical losses in lean body mass: a pooled analysis of randomized controlled trials. Clin Nutr 38:1053–1060
Carli F, Bousquet-Dion G, Awasthi R et al (2020) Effect of multimodal prehabilitation vs postoperative rehabilitation on 30-day postoperative complications for frail patients undergoing resection of colorectal cancer: a randomized clinical trial. JAMA Surg 155(3):233–242
Viannay P, Hamel JF, Bougard M, Barbieux J, Hamy A, Venara A (2021) Gastrointestinal motility has more of an impact on postoperative recovery than you might expect. J Visc Surg 158:19–26
Barbieux J, Hamy A, Talbot MF et al (2017) Does enhanced recovery reduce postoperative ileus after colorectal surgery? J Visc Surg 154(2):79–85
Ludwig K, Viscusi ER, Wolff BG, Delaney CP, Senagore A, Techner L (2010) Alvimopan for the management of postoperative ileus after bowel resection: characterization of clinical benefit by pooled responder analysis. World J Surg 34(9):2185–2190
Vather R, Trivedi S, Bissett I (2013) Defining postoperative ileus: results of a systematic review and global survey. J Gastrointest Surg 17(5):962–972
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Bergström J, Fürst P, Norée LO, Vinnars E (1974) Intracellular free amino acid concentration in human muscle tissue. J Appl Physiol 36(6):693–697
Diebel LN, Liberati DM, Hall-Zimmerman L (2011) H2 blockers decrease gut mucus production and lead to barrier dysfunction in vitro. Surgery 150(4):736–743
Lee YJ, Hussain Z, Huh CW, Lee YJ, Park H (2018) Inflammation, impaired motility, and permeability in a guinea pig model of postoperative ileus. J Neurogastroenterol Motil 24(1):147–158
Kalff JC, Schraut WH, Billiar TR, Simmons RL, Bauer AJ (2000) Role of inducible nitric oxide synthase in postoperative intestinal smooth muscle dysfunction in rodents. Gastroenterology 118(2):316–327
Slim K, Reymond T, Joris J, Paul S, Pereira B, Cotte E (2020) Intolerance to early oral feeding in enhanced recovery after colorectal surgery: an early red flag? Colorectal Dis 22(1):95–101
Gignoux B, Gosgnach M, Lanz T et al (2019) Short-term outcomes of ambulatory colectomy for 157 consecutive patients. Ann Surg 270:317–321
Collaborative EuroSurg (2020) Safety of hospital discharge before return of bowel function after elective colorectal surgery. Br J Surg 107(5):552–559
Venara A, Duchalais E, Dariel A et al (2018) Anti-inflammatory effects of enhanced recovery programs on early-stage colorectal cancer surgery. World J Surg 42(4):953–964
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation: Fabulas, Paisant, Dinomais, Venara. Data collection: Fabulas, Paisant, Casa, Mucci, Le Naoures, Data analysis: Fabulas, Perrot, Hamel, Venara. Writing — original draft preparation: Fabulas, Paisant, Perrot, Venara. Writing — review and editing: Fabulas, Paisant, Dinomais, Casa, Mucci, Le Naoures, Hamel, Perrot, Venara. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was waived by the local Ethics Committee of the University of A in view of the retrospective nature of the study and the fact that all the procedures being performed were part of routine care.
Consent to participate
Being a retrospective study, all patients were informed that their data could be used for medical research and were asked to indicate if they did not agree to such use. None of the patients indicated disagreement.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fabulas, F., Paisant, P., Dinomais, M. et al. Pre-habilitation before colorectal cancer surgery could improve postoperative gastrointestinal function recovery: a case-matched study. Langenbecks Arch Surg 407, 1595–1603 (2022). https://doi.org/10.1007/s00423-022-02487-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02487-8