Abstract
Purpose
Our goal was to assess the outcomes of rectal wall suture during the early and late periods after transanal endoscopic microsurgery (TEM) and long-term bowel function.
Methods
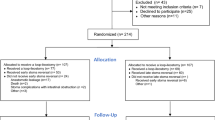
Patients who underwent TEM for rectal neoplasms from May 2017 to March 2021 were prospectively included. A total of 70 patients were enrolled. Seven to 10 days after TEM, clinical data were recorded, and digital rectal examination and rigid proctoscopy were performed. After at least 6 months, bowel function was evaluated using low anterior resection syndrome (LARS) and Wexner questionnaires.
Results
Forty-five men with an average age of 67 ± 10.1 (40–85) were included. TEM sutures were recorded as intact in 48/70 (68%) and as dehiscent in 22/70 (32%). It did not have any significant clinical manifestation and was not related with longer postoperative stay or incidence of postoperative complications. Eight of 22 (36.4%) patients with suture dehiscence had per rectal bleeding or febrile temperature without any need for intervention or treatment. The only risk factor for wound dehiscence was a posteriorly located defect. In late postoperative period, there was no difference between groups in LARS or Wexner questionnaire (p value 0.72 and 0.85, respectively).
Conclusions
Our study suggests that 1/3 of the patients’ rectal wall defect after TEM will undergo dehiscence in early postoperative period and will not transfer to clinically significant manifestation (without a need of hospitalization or prolonging it). In late postoperative period, there is no difference in bowel function.


Similar content being viewed by others
References
https://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf. Accessed on 4th January, 2022
Bosch S, Teerenstra S, De Wilt JW, Cunningham C, Nagtegaal I (2013) Predicting lymph node metastasis in pT1 colorectal cancer: a systematic review of risk factors providing rationale for therapy decisions. Endoscopy 45(10):827–834
Monson JRT, Weiser MR, Buie WD, Chang GJ, Rafferty JF (2013) Practice parameters for the management of rectal cancer (revised). Dis Colon Rectum 56(5):535–550
Menahem B, Alves A, Morello R, Lubrano J (2017) Should the rectal defect be closed following transanal local excision of rectal tumors? A systematic review and meta-analysis. Tech Coloproctol 21(12):929–936
Brown C, Raval MJ, Phang PT, Karimuddin AA (2017) The surgical defect after transanal endoscopic microsurgery: open versus closed management. Surg Endosc 31(3):1078–1082
Noura S, Ohue M, Miyoshi N, Yasui M (2016) Significance of defect closure following transanal local full-thickness excision of rectal malignant tumors. Mol Clin Oncol 5(4):449–454
Ramirez JM, Aguilella V, Arribas D, Martinez M (2002) Transanal full-thickness excision of rectal tumours: should the defect be sutured? a randomized controlled trial. Colorectal Dis 4(1):51–55
Samalavicius NE, Dulskas A, Lasinskas M, Smailyte G (2016) Validity and reliability of a Lithuanian version of low anterior resection syndrome score. Tech Coloproctol 20(4):215–220
Clancy C, Burke JP, Albert MR, O’Connell PR, Winter DC (2015) Transanal endoscopic microsurgery versus standard transanal excision for the removal of rectal neoplasms: a systematic review and meta-analysis. Dis Colon Rectum 58(2):254–261
Martin-Perez B, Andrade-Ribeiro GD, Hunter L, Atallah S (2014) A systematic review of transanal minimally invasive surgery (TAMIS) from 2010 to 2013. Tech Coloproctol 18(9):775–788
Kumar AS, Coralic J, Kelleher DC, Sidani S, Kolli K, Smith LE (2013) Complications of transanal endoscopic microsurgery are rare and minor: a single institution’s analysis and comparison to existing data. Dis Colon Rectum 56(3):295–300
Marques CFS, Nahas CSR, Ribeiro U, Bustamante LA, Pinto RA, Mory EK et al (2016) Postoperative complications in the treatment of rectal neoplasia by transanal endoscopic microsurgery: a prospective study of risk factors and time course. Int J Colorectal Dis 31(4):833–841
Restivo A, Zorcolo L, D’Alia G, Cocco F, Cossu A, Scintu F et al (2016) Risk of complications and long-term functional alterations after local excision of rectal tumors with transanal endoscopic microsurgery (TEM). Int J Colorectal Dis 31(2):257–266
Kreissler-Haag D, Schuld J, Lindemann W, König J, Hildebrandt U, Schilling M (2008) Complications after transanal endoscopic microsurgical resection correlate with location of rectal neoplasms. Surg Endosc Other Interv Tech 22(3):612–616
Bignell MB, Ramwell A, Evans JR, Dastur N, Simson JNL. Complications of transanal endoscopic microsugery (TEMS). A Prospective Audit. Color Dis. 2009;99–103.
Morino M, Allaix ME, Famiglietti F, Caldart M, Arezzo A (2013) Does peritoneal perforation affect short- and long-term outcomes after transanal endoscopic microsurgery? Surg Endosc 27(1):181–188
Lee L, Althoff A, Edwards K, Albert MR, Atallah SB, Hunter IA et al (2018) Outcomes of closed versus open defects after local excision of rectal neoplasms: a multi-institutional matched analysis. Dis Colon Rectum 61(2):172–178
Hahnloser D, Cantero R, Salgado G, Dindo D, Rega D, Delrio P (2015) Transanal minimal invasive surgery for rectal lesions: should the defect be closed? Color Dis 17(5):397–402
Benson AB, Venook AP, Al-Hawary MM, Cederquist L, Chen YJ, Ciombor KK, et al. Rectal cancer, version 2.2018 clinical practice guidelines in Oncology. JNCCN J Natl Compr Cancer Netw. 2018;16(7):874–901.
Van Heinsbergen M, Leijtens JW, Slooter GD, Janssen-Heijnen ML, Konsten JL (2020) Quality of life and bowel dysfunction after transanal endoscopic microsurgery for rectal cancer: one third of patients experience major low anterior resection syndrome. Dig Surg 37(1):39–46
Jones HJS, Al-Najami I, Cunningham C. Quality of life after rectal-preserving treatment of rectal cancer. Eur J Surg Oncol [Internet]. 2020;46(11):2050–6. Available from: https://doi.org/10.1016/j.ejso.2020.07.018
Jakubauskas M, Jotautas V, Poskus E, Mikalauskas S, Valeikaite-Tauginiene G, Strupas K et al (2018) Fecal incontinence after transanal endoscopic microsurgery. Int J Colorectal Dis 33(4):467–472
Acknowledgements
This research was funded by the European Social Fund under the No 09.3.3-LMT-K-712 “Development of Competences of Scientists, other Researchers and Students through Practical Research Activities” measure.
Author information
Authors and Affiliations
Contributions
NES, VP, PK, and AD contributed to this work, satisfying the following four criteria of the guidelines of the International Committee of Medical Journal Editors (ICMJE): substantial contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Informed consent
Informed consent was obtained from the patient.
Conflict of interest
The authors declare no competing interest.
Research involving human participants and/or animals
All procedures involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This article does not contain any studies using animals.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Part of the material was presented as an e-poster at ASCRS conference in Cleveland, USA, June 4, 2019, and as a poster at ESCP conference in Vienna, Austria, September 25, 2019.
What does this paper add to the literature?
Thirty-two percent of rectal wounds after suturing using TEM will dehisce without any clinical manifestation. There is no difference in bowel function in long postoperative period. This might show that leaving the wound open is safe and reasonable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dulskas, A., Petrauskas, V., Kavaliauskas, P. et al. Short-term clinical and functional results of rectal wall suture defect after transanal endoscopic microsurgery—a prospective cohort study. Langenbecks Arch Surg 407, 2035–2040 (2022). https://doi.org/10.1007/s00423-022-02476-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02476-x