Abstract
Purpose
To the best of our knowledge, no studies have compared the short-term outcomes between colo-colonic extracorporeal triangular anastomosis (TA) and functional end-to-end anastomosis (FEEA), with a focus on laparoscopic-assisted surgery for left-sided colon cancer. Therefore, this study compared the short-term outcomes of these anastomoses using propensity score matching analysis.
Methods
This retrospective study included 129 patients with stage I–IV left-sided colon cancer who underwent laparoscopic-assisted surgery with colo-colonic extracorporeal TA (n = 75) or FEEA (n = 54) between May 2009 and March 2021. After propensity score matching, 84 patients (TA, n = 42; FEEA, n = 42) were included in the analysis. The primary endpoint was the complication rate for all grades, and the secondary endpoints were the rates of Clavien − Dindo grade ≥ 3 complications and anastomotic leakage.
Results
In the matched cohort, there were no significant differences in the complication rates for all grades (35.7% vs. 26.2%, p = 0.479), Clavien − Dindo grade ≥ 3 complications (11.9% vs. 11.9%, p = 1), and anastomotic leakage (0% vs. 4.8%, p = 0.494) between the TA and FEEA groups. In the univariate logistic regression analysis, TA did not increase the frequency of complications for any grades compared with FEEA (odds ratio: 1.570, 95% confidence interval: 0.616–3.980, p = 0.347).
Conclusion
Extracorporeal TA demonstrated equivalent short-term outcomes compared with FEEA in cases of laparoscopic-assisted surgery for left-sided colon cancer. TA can be an alternative anastomosis technique in cases wherein FEEA is difficult to perform.


Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available on request from the corresponding author.
Code availability
Not applicable
References
Steichen FM (1968) The use of staplers in anatomical side-to-side and functional end-to-end enteroanastomoses. Surg. 64:948–953
Kyzer S, Gordon PH (1992) The stapled functional end-to-end anastomosis following colonic resection. Int J Colorectal Dis 7:125–131. https://doi.org/10.1007/BF00360351
Fingerhut A, Elhadad A, Hay JM, Lacaine F, Flamant Y (1994) Infraperitoneal colorectal anastomosis: hand-sewn versus circular staples. A controlled clinical trial. French Associations for surgical Research. Surgery 116:484–490
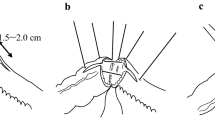
Venkatesh KS, Morrison N, Larson DM, Ramanujam P (1993) Triangulating stapling technique: an alternative approach to colorectal anastomosis. Dis Colon Rectum 36:73–76. https://doi.org/10.1007/BF02050306
Toh Y, Sakaguchi Y, Ikeda O, Adachi E, Ohgaki K, Yamashita Y, Oki E, Minami K, Okamura T (2009) The triangulating stapling technique for cervical esophagogastric anastomosis after esophagectomy. Surg Today 39:201–206. https://doi.org/10.1007/s00595-008-3827-2
Omori T, Masuzawa T, Akamatsu H, Nishida T (2014) A simple and safe method for Billroth I reconstruction in single-incision laparoscopic gastrectomy using a novel intracorporeal triangular anastomotic technique. J Gastrointest Surg 18:613–616. https://doi.org/10.1007/s11605-013-2419-7
Fukunaga Y, Higashino M, Tanimura S, Osugi H (2007) Triangulating stapling technique for reconstruction after colectomy. Hepatogastroenterology 54:414–417
Yoshimatsu K, Ishibashi K, Yokomizo H, Umehara A, Yoshida K, Fujimoto T, Watanabe K, Ogawa K (2007) Triangulating anastomosis using a linear cutter in a colectomy. Hepatogastroenterology 54:1988–1990
Japanese Society for Cancer of the Colon and Rectum (2019) Japanese classification of colorectal, appendiceal, and anal carcinoma: the 3D english edition [Secondary Publication]. J Anus Rectum Colon, English ed. 3:175–195. https://doi.org/10.23922/jarc.2019-018.
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y, Laurberg S, den Dulk M, van de Velde C, Büchler MW (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the international study group of rectal cancer surgery 147:339–351. https://doi.org/10.1016/j.surg.2009.10.012
Rubin D, Rosenbaum P (1985) Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat 39:33–38
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Kosuge M, Eto K, Hashizume R, Takeda M, Tomori K, Neki K, Mitsumori N, Yanaga K (2017) Which is the safer anastomotic method for colon surgery? - ten-year results. In Vivo 31:683–687. https://doi.org/10.21873/invivo.11113
Sameshima S, Koketsu S, Yoneyama S, Miyato H, Kaji T, Sawada T (2009) Outcome of functional end-to-end anastomosis following right hemicolectomy. Int Surg 94:249–253
Fukunaga Y, Higashino M, Tanimura S, Nishiguchi Y, Kishida S, Nishikawa M, Ogata A, Osugi H (2003) A novel laparoscopic technique for stapled colon and rectal anastomosis. Tech Coloproctol 7:192–197. https://doi.org/10.1007/s10151-003-0034-4
Tsuji T, Ojima T, Nakamori M, Nakamura M, Katsuda M, Hayata K, Kitadani J, Maruoka S, Shimokawa T, Yamaue H (2019) Triangulating stapling vs functional end-to-end stapling for cervical esophagogastric anastomosis after esophagectomy for thoracic esophageal cancer: study protocol for a randomized controlled trial. Trials 20:83. https://doi.org/10.1186/s13063-019-3201-2
Austin PC (2018) Assessing the performance of the generalized propensity score for estimating the effect of quantitative or continuous exposures on binary outcomes. Stat Med 37:1874–1894. https://doi.org/10.1002/sim.7615
Baek S, Park SH, Won E, Park YR, Kim HJ (2015) Propensity score matching: a conceptual review for radiology researchers. Korean J Radiol 16:286–296. https://doi.org/10.3348/kjr.2015.16.2.286
Author information
Authors and Affiliations
Contributions
KS, KI, HK, MK, MU, YT, DY, AS, KI, and KN contributed to the study concept and design. KS, KI, HK, MK, MU, YT, DY, AS, and KI performed the operations. HK and KN supervised the study. KS, KI, HK, MK, MU, YT, DY, AS, KI, and KN participated in the interpretation of the results and writing of the report. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Human Research Ethics Committee of Hakodate Municipal Hospital (Hakodate, Hokkaido, Japan; reference no. 2021–43).
Consent to participate
Informed consent was obtained in the form of opt-out.
Consent for publication
Informed consent was obtained in the form of opt-out.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sato, K., Imaizumi, K., Kasajima, H. et al. Short-term outcomes of extracorporeal colo-colonic triangular anastomosis versus functional end-to-end anastomosis in laparoscopic-assisted surgery for left-sided colon cancer: a propensity score matching analysis. Langenbecks Arch Surg 407, 747–757 (2022). https://doi.org/10.1007/s00423-021-02403-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02403-6