Abstract
Introduction
Meta-analysis aimed to quantify the relationship between intraductal papillary mucinous neoplasm (IPMN) and increased incidence of extra-pancreatic malignancy (EPM) previously reported in qualitative observational cohort studies.
Methods
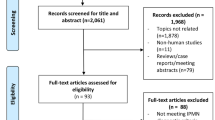
Study protocol was registered with PROSPERO (CRD42020169614) and conducted to the Meta-analysis Of Observational Studies in Epidemiology and systematic review reported with Preferred Reporting Items for Systematic Reviews and Meta-Analyses, Assessing the Methodological Quality of Systematic Reviews guidelines.
Results
Sixteen studies (total of 8240 patients) were included in the pooled, and 7399 patients in the subgroup meta-analyses. The odds ratio (OR) for any EPM in the presence of IPMN was 57.9 (95% confidence interval 40.5–82.7), fixed effects, I2 = 59% (p < 0.0014). Subgroup analysis for any gastrointestinal EPM (i.e. oesophagus, stomach, colon and rectum) in the presence of an IPMN estimated an overall OR of 12.9 (95% confidence interval 8.8–19.0), fixed effects, I2 = 64% (p < 0.0004).
Conclusion
Patients with an IPMN are categorically at increased risk for a higher incidence of EPM and particularly the odds of a gastrointestinal malignancy are also increased in comparison with the general population. We advocate that patients presenting with an IPMN should be considered for gastrointestinal screening including colonoscopy, upper gastrointestinal endoscopy or computed tomography.




Similar content being viewed by others
References
Itai Y et al (1986) “Ductectatic” mucinous cystadenoma and cystadenocarcinoma of the pancreas. Radiology 161(3):697–700
van Huijgevoort NCM et al (2019) Diagnosis and management of pancreatic cystic neoplasms: current evidence and guidelines. Nat Rev Gastroenterol Hepatol 16(11):676–689
Scholten L et al (2018) Pancreatic cystic neoplasms: different types, different management, new guidelines. Visc Med 34(3):173–177
Sugiyama M, Atomi Y (1999) Extrapancreatic neoplasms occur with unusual frequency in patients with intraductal papillary mucinous tumors of the pancreas. Am J Gastroenterol 94(2):470–473
Benarroch-Gampel J, Riall TS (2010) Extrapancreatic malignancies and intraductal papillary mucinous neoplasms of the pancreas. World J Gastrointest Surg 2(10):363–367
Bouquot M et al (2018) Pancreatectomy for pancreatic incidentaloma: what are the risks? Pancreatology 18(1):114–121
Baiocchi GL et al (2015) Increased risk of second malignancy in pancreatic intraductal papillary mucinous tumors: review of the literature. World J Gastroenterol 21(23):7313–7319
Stroup DF et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama 283(15):2008–2012
Moher D et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1):1
Ferlay J et al (2019) Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 144(8):1941–1953
Bray F et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Ferlay J et al (2018) Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer 103:356–387
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2020) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Egger M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Kamisawa T et al (2005) Malignancies associated with intraductal papillary mucinous neoplasm of the pancreas. World J Gastroenterol 11(36):5688–5690
Choi MG et al (2006) High incidence of extrapancreatic neoplasms in patients with intraductal papillary mucinous neoplasms. Arch Surg 141(1):51–56
Baumgaertner I et al (2008) Prevalence of extrapancreatic cancers in patients with histologically proven intraductal papillary mucinous neoplasms of the pancreas: a case-control study. Am J Gastroenterol 103(11):2878–2882
Ishida M et al (2008) Synchronous and metachronous extrapancreatic malignant neoplasms in patients with intraductal papillary-mucinous neoplasm of the pancreas. Pancreatology 8(6):577–582
Yoon WJ et al (2008) Extrapancreatic malignancies in patients with intraductal papillary mucinous neoplasm of the pancreas: prevalence, associated factors, and comparison with patients with other pancreatic cystic neoplasms. Ann Surg Oncol 15(11):3193–3198
Reid-Lombardo KM et al (2010) Frequency of extrapancreatic neoplasms in intraductal papillary mucinous neoplasm of the pancreas: implications for management. Ann Surg 251(1):64–69
Kawakubo K et al (2011) Incidence of extrapancreatic malignancies in patients with intraductal papillary mucinous neoplasms of the pancreas. Gut 60(9):1249–1253
Lubezky N et al (2012) Intraductal papillary mucinous neoplasm of the pancreas: associated cancers, family history, genetic predisposition? Surgery 151(1):70–75
Larghi A et al (2013) Prevalence and risk factors of extrapancreatic malignancies in a large cohort of patients with intraductal papillary mucinous neoplasm (IPMN) of the pancreas. Ann Oncol 24(7):1907–1911
Malleo G et al (2015) Observational study of the incidence of pancreatic and extrapancreatic malignancies during surveillance of patients with branch-duct intraductal papillary mucinous neoplasm. Ann Surg 261(5):984–990
Marchegiani G et al (2015) Association between pancreatic intraductal papillary mucinous neoplasms and extrapancreatic malignancies. Clin Gastroenterol Hepatol 13(6):1162–1169
Kato T et al (2016) Malignant, but not benign, intraductal papillary mucinous neoplasm preferentially associates with prior extrapancreatic malignancies. Oncol Rep 35(6):3236–3240
Roch AM et al (2016) Intraductal papillary mucinous neoplasm of the pancreas, one manifestation of a more systemic disease? Am J Surg 211(3):512–518
Panic N et al (2018) Prevalence of extrapancreatic malignancies among patients with intraductal papillary mucinous neoplasms of the pancreas. Pancreas 47(6):721–724
Huang X et al (2019) Increased risk of second primary cancers following diagnosis of malignant intraductal papillary mucinous neoplasms of the pancreas: a population-based study. Front Oncol 9:610
Riall TS et al (2007) Incidence of additional primary cancers in patients with invasive intraductal papillary mucinous neoplasms and sporadic pancreatic adenocarcinomas. J Am Coll Surg 204(5):803–13
Pugliese L et al (2015) Increased incidence of extrapancreatic neoplasms in patients with IPMN: Fact or fiction? A critical systematic review. Pancreatology 15(3):209–216
Oh SJ et al (2009) Extrapancreatic tumors in intraductal papillary mucinous neoplasm of the pancreas. Korean J Gastroenterol 54(3):162–166
Zhang J, Yu KF (1998) What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280(19):1690–1691
Cairns SR et al (2010) Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002). Gut 59(5):666–689
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval.
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable as there were no human participants.
Research involving human participants and/or animals
None.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Provenance and peer review not commissioned, externally peer-reviewed.
Rights and permissions
About this article
Cite this article
Kumar, R., Fraser, R. & Garcea, G. A meta-analysis: incidental intraductal papillary mucinous neoplasm and extra-pancreatic malignancy. Langenbecks Arch Surg 407, 451–458 (2022). https://doi.org/10.1007/s00423-021-02355-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02355-x