Abstract
Background
Intraductal papillary mucinous neoplasm (IPMN) is a cystic tumor of the pancreas arising from abnormal papillary proliferation of ductal epithelial cells, and is a precancerous lesion of pancreatic malignancy. This study aimed to evaluate associations between acute pancreatitis (AP) and histologic subtypes of IPMN.
Methods
In the clinical study, patients with IPMN confirmed by surgical resection specimens at our institute between 2009 and 2021 were eligible for inclusion. Associations and predictive accuracy of AP on the presence of HGD were determined by logistic regressions. In addition, a systematic review and meta-analysis was conducted through literatures upon search in PubMed, Embase, CENTRAL, China National Knowledge Infrastructure (CKNI), and Wanfang database, up to June, 2023. Pooled effects of the associations between AP and HGD and intestinal epithelial subtype subtype, shown as odds ratios (ORs) with 95% confidence intervals (CIs), were calculated using random effects model.
Results
The retrospective cohort study included 47 patients (32 males, 15 females) diagnosed with IPMN at our center between 2009 and 2021, including 11 cases with AP (median 62 years) and 36 cases (median 64.5 years) without. Accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of AP in predicting HGD were 78.7%, 57.1%, 82.5%, 36.4%, and 91.7%, respectively. Univariate logistic regression analysis showed that AP group had greater odds of presence of HGD (OR: 6.29,95% CI: 1.14–34.57) than non-AP group. Meta-analysis of five case-control studies in the literature included 930 patients and showed that AP-IPMN patients had higher odds for HGD (OR: 2.13, 95% CI 1.38–3.29) and intestinal epithelial subtype (OR: 5.38, 95% CI: 3.50–8.27) compared to non-AP IPMN.
Conclusions
AP is predictive of malignancy in patients with IPMN.
Similar content being viewed by others
Background
IPMN is a cystic tumor of the pancreas characterized by abnormal papillary growth of ductal epithelial cells and mucus production [1]. It is considered a precursor to pancreatic malignancy. It is often asymptomatic, although some cases may present with symptoms such as abdominal pain, weight loss, steatorrhea, new-onset diabetes, pancreatitis, or obstructive jaundice [1].
The incidence and diagnosis of IPMN have been increasing over the past three decades, particularly among older adults, partly due to advancements in imaging technology [2]. IPMN can be classified into different types based on the location of the lesion, namely main duct, branch duct, and mixed type [3]. According to the 2010 WHO classification criteria, IPMN can be further categorized into low-grade dysplasia (LGD), intermediate-grade dysplasia (MGD), high-grade dysplasia (HGD), and invasive carcinoma (IC) [4]. Furthermore, based on the histologic characteristics of tumor epithelial cells, IPMN can be divided into four subtypes: gastric, intestinal, pancreaticobiliary, and eosinophilic [5,6,7,8,9].
Acute pancreatitis is an inflammatory response of the pancreatic tissue caused by the activation of pancreatic enzymes, and it has been observed that AP is closely associated with pancreatic tumors [10]. A proportion of unexplained AP cases, around 9%, are caused by tumors, and some tumors present with AP as their initial manifestation [11, 12]. Studies have shown varying associations between AP and IPMN histology. For instance, Venkatesh et al. reported that 12–67% of IPMN patients experience AP, and 7–34.6% of AP cases are associated with IPMN [13]. However, the relationship between AP and specific histologic subtypes of IPMN remains uncertain. Jang et al. found that AP due to IPMN is more frequent in the competent and mixed subtypes, while Hata et al. reported that most AP cases associated with IPMN are from the intestinal subtype [14, 15]. Other studies have explored the association between AP and the degree of histologic heterogeneity in IPMN, yielding conflicting results [16,17,18,19,20,21].
There is a lack of comprehensive studies on the clinical characteristics of IPMN patients in China. Therefore, our study aimed to fill this gap by conducting a cohort study to investigate the associations between AP and malignant IPMN histology in a single center in southern China, with a systematic review and meta-analysis. By clarifying the relationship between AP and specific histologic subtypes of IPMN, we hope to provide insights for improving these conditions’ understanding, diagnosis, and management.
Methods
Clinical study
Study design and sample
Patients with IPMN were confirmed by surgical resection specimens at our hospital between January 2009 and January 2021. Patients with AP induced by gallstones, hyperlipidemia, autoimmunity, pancreas malformation, iatrogenesis, or alcohol abuse were excluded. All data, including demographic, clinical, and histological characteristics, were collected from medical records.
Indications for surgery were: IPMN diagnosed by image (CT or MRI) and met one or more of the following: (1) main pancreatic duct (MPD) dilation ≥ 10 mm; (2) combined with obstructive jaundice; (3) enhanced wall nodules ≥ 5 mm; 4). complicated with acute or chronic pancreatitis; 5) cachexia without known causes; and 6) upper abdominal pain that cannot be relieved by active medical treatment and without other known causes.
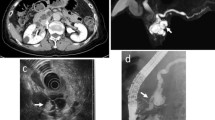
All IPMN diagnoses were histologically confirmed as cystic or solid lesions or pancreatic duct dilatation. On the other hand, the diagnosis of AP, according to the revised Atlanta Classification, [22] requires two of the following findings: (1) typical abdominal pain of AP; (2) serum lipase activity (and/or amylase activity) at least three times higher than the upper limit of normal value; (3) characteristics of AP on computer tomography (CT), magnetic resonance imaging (MRI), or sonographic findings.
The outcomes of interest were the predictive performance of AP on HGD, as well as the association between AP-IPMN (versus non-AP-IPMN) and the presence of HGD.
Ethics considerations
The study protocol was approved by the Institutional Review Board of Sun Yat-Sen Memorial Hospital (approval number: SYSEC-KY-KS-2021-017), and informed consent of included patients was waived due to the study’s retrospective nature.
Systematic review and Meta-analysis
Search strategy and selection criteria
This systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [23]. PubMed, Embase, CENTRAL, CKNI, and Wanfang databases were searched, up to June 1, 2023. The search terms and the combinations were: (“IPMN” OR “intraductal papillary mucinous neoplasm” OR “IPMT” OR “intraductal papillary mucinous tumor” OR “IPMA” OR “intraductal papillary mucinous adenoma” OR “IPMC” OR “intraductal papillary mucinous carcinoma”) AND (“pancreatitis” OR “acute pancreatitis” OR “AP”). No filters were applied in the search.
Inclusion and exclusion criteria
The inclusion criteira of this systematic review and meta-analysis was performed in accordance with the PECO criteria (participants, exposure, comparison, and outcomes). P: patients with IPMN confirmed by histopathology or image, E: AP group; C: non-AP group; O: presence of HGD or intestinal epithelial subtype. There was no language restriction for the study eligibility.
Exclusion criteria were: reviews / case reports / meeting abstracts; non-human studies, studies without outcomes of interest; patients not meeting IPMN or AP diagnostic criteria; and patients’ AP was due to other causes such as gallstones, alcohol, high triglycerides, autoimmune diseases, metabolic diseases, or pancreas anatomical abnormalities.
Data extraction
Two investigators independently searched the literature, screened and evaluated the included studies, and extracted relevant data. In disagreements, the third author and the two investigators discussed and agreed through consultation. Extraction of the study data included authors, year of publication, study site, study type, sample size, age, sex, presence of pancreatitis (number of episodes, severity, etiology), IPMN characteristics (location, typing, degree of histiocytic heterogeneity, epithelial cell subtype), treatment method, follow-up, and prognosis.
Quality Assessment
The Newcastle-Ottawa Scale (NOS) was used to assess the quality of the studies included [24]. The NOS scale assigns a maximum of nine points to each study, with four points awarded for acceptable participant selection, two points awarded for participant comparability based on design and analysis, and three points awarded for adequate outcome ascertainment. Studies with five or more points were considered high quality. Two independent reviewers conducted the quality assessment. A third reviewer was consulted if uncertainties existed.
Statistical analysis
For clinical data analysis, categorical data are presented as n (%) and analyzed using Fisher’s exact test. Continuous data are presented as the median (Q1-Q3) and analyzed by the Wilcoxon rank sum test. Univariate and multivariate logistic regression models were used to estimate odds ratios (ORs) and 95% confidence intervals (CIs). All statistical tests were two-sided with a significance level of 0.05. Data management and statistical analyses were conducted using SAS version 9.4 software (SAS Institute, Inc.).
The χ2 test for homogeneity was performed for meta-analysis, and heterogeneity between studies was assessed using Cochran Q and I2 statistics. A random-effects model was used if the I2 statistic was more than 50%. When a few studies were included in the meta-analysis, the statistical power of the heterogeneity test was low [25] and a random effects model was used [26]. Pooled effects were calculated and shown as ORs and 95% CIs, with bilateral p-values < 0.05 considered statistically significant. The meta-analysis used Review Manager (version 5.3, Cochrane Collaboration).
Results
Clinical study
A total of 47 patients with IPMN were included in this study, 11 with AP-IPMN and 36 with non-AP IPMN. In the non-AP group, 25 patients were symptomatic, in which 8 had obstructive jaundice, 1 had calchexia, and 16 had abdominal pain not relieved by active medical treatment.
Baseline characteristics are shown in Table 1. The median age was 62.0 (Q1-Q3: 52.0–72.0) for the AP-IPMN group and 64.5 (Q1-Q3: 57.5–69.5) for the non-AP IPMN group. No significant differences were found in family history and laboratory values between the two groups. However, smoking (p = 0.033) and hypertension (p = 0.039) were more prevalent in the non-AP than AP group.
The clinical characteristics of patients in the AP-IPMN and non-AP-IPMN groups are shown in Table 2. Radiology findings revealed no significant differences between the two groups in terms of tumor site, tumor type, main pancreatic duct (MPD) size, cyst/mass size, presence of reinforced wall nodules, reinforced cyst wall, and calcification (all P > 0.05). In addition, no significant differences were found between the two groups regarding pathologic features in the epithelial subtype, degree of dysplasia, chronic pancreatitis, and glandular atrophy (all P > 0.05).
Tools for sensitivity, specificity, PPV, NPV, and accuracy were analyzed using MPD size, jaundice, tuberous enhancement, and AP as predictors of the degree of dysplasia and intestinal epithelial subtype (Table 3). Among patients with IPMN, patients with AP had the highest PPV (36.4%), NPV (91.7%), and accuracy (78.7%) for HGD when compared to the results of the other three tools. In addition, the sensitivity of AP in predicting HGD (57.1%) was the same as that of MPD ≥ 10 mm. The specificity of AP in predicting HGD (82.5%) was the same as the specificity for jaundice. However, AP was less predictive for invasive cancer, malignant (HGD + IC), and intestinal epithelial subtypes than MPD ≥ 10 mm or jaundice.
Association AP and the degree of dysplasia and intestinal epithelial subtype, eavluated by surgical specimens, were further analyzed (Table 4). The proportion of developing HGD was significantly higher in the AP-IPMN group (36.4%) than in the non-AP IPMN group (8.3%) (p = 0.042). Univariate logistic regression analysis showed that the risk of developing HGD was significantly higher in the AP-IPMN group than in the non-AP IPMN group (OR: 6.29; 95% CI: 1.14–34.57). However, multivariable logistic regression analysis revealed no significant associations between AP and HGD.
Perioperative outcomes in patients having IPMN with and without AP are documented in Supplementary Table 1. The median postoperative hospitalization days in the AP-IPMN group was 8.0 (Q1-Q3: 6.0–19.0), which was significantly less than the median postoperative hospitalization days in the non-AP IPMN group of 21.0 (Q1-Q3: 11.0–39.0) (p = 0.014). No significant differences were found in postoperative complications between the two groups. However, the proportion of tumor recurrence after hospital discharge was significantly higher in the AP-IPMN group (27.3%) than in the non-AP IPMN group (2.9%) (p = 0.037).
Meta-analysis
The PRISMA flow diagram of study selection process is shown in Fig. 1. Initially 2,579 records were retrieved through search, after exclusion, five articles were included in the qualitative and quantitative synthesis (Fig. 1).
The five studies included were all case-control designs, with a total of 930 patients who had histologically confirmed IPMN. Among which, 184 (19.8%) had AP and 746 (80.2%) had not. Characteristics of the two groups are shown in Table 5. The mean age at diagnosis was 66.1 years, and 54.5% were males. The follow-up duration ranged from 1 to 168 months. The NOS scale scores of the included studies, as summarized in Table 5, were 6 to 8, upon which all studies were considered high quality. Details of study quality in each domain of NOS are documented in Supplementary Table 2.
Figure 2 shows the meta-analysis of the two groups of patients with AP-IPMN and non-AP IPMN, evaluating the different degrees of dysplasia and development of the intestinal epithelial subtype in IPMN. The random effects model was applied for various degrees of dysplasia and development of intestinal epithelial subtype (high grade: I2 = 0%, P < 0.001; high grade or invasive cancer: I2 = 62%, P = 0.58; invasive cancer: I2 = 5%, P = 0.53; intestinal epithelial subtype: I2 = 0%, P < 0.001). The pooled analysis showed that patients with AP-IPMN had an increased risk of high grade compared to non-AP IPMN (OR: 2.13; 95% CI: 1.38–3.29). In addition, patients with AP-IPMN had a higher risk of developing an intestinal epithelial subtype than non-AP IPMN patients (OR: 5.38; 95% CI: 3.50–8.27).
Discussion
The present study investigated IPMN, the most common cystic tumor of the pancreas, [24] in patients with AP, finding that patients with AP IPMN had a higher risk of HGD and the intestinal type of IPMN than patients with non-AP IPMN. AP effectively predicted highly differentiated heterogeneity with satisfactory sensitivity, specificity, positive and negative predictive values, and high accuracy.
A review of the included studies showed that the risk of malignancy in IPMN patients with a history of pancreatitis was significantly higher than in those without a history of pancreatitis [17,18,19, 25]. However, Roch et al. [26] did not find associations between AP history and malignancy in IPMN patients. Differences between populations in the included studies may have contributed to the inconsistent findings.
The results of the meta-analysis in the present study showed that AP is associated with highly heterogeneous IPMN and intestinal IPMN. The mechanism of AP development in IPMN is generally considered to be mucus production that leads to mechanical obstruction of the pancreatic duct, causing increased intra-pancreatic ductal pressure, rupture of the pancreatic vesicles, release, and activation of pancreatic enzymes, digestion of the pancreatic self-tissue, and activation of inflammatory factors that ultimately result in pancreatitis [27]. The described mechanism and the previous and present findings suggest that pancreatitis is associated with malignant IPMN. However, further study is still needed to identify associated factors between AP and malignancy in patients with IPMN.
The proportion of patients with a smoking history was significantly higher among non-AP IPMN patients than AP IPMN patients. Smoking is a known risk factor for pancreatitis [28]. However, Chavan et al. found a protective pancreatic effect of smoking against endoscopic retrograde cholangiopancreatography-induced pancreatitis, which may be due to the anti-inflammatory response of nicotine via the cholinergic anti-inflammatory pathway [29]. Recently, animal studies have also shown that nicotine reduces the severity of ERCP-induced pancreatitis by stimulating splenic T-cells, which play a protective role in the pancreas [30]. This mechanism, in particular, helps to explain the significantly lower proportion of smoking found in AP patients.
Implications
The findings of this study highlight the importance of considering AP history when assessing the risk of malignancy in IPMN patients during clinical practice. Further research is needed to identify specific factors linking AP and malignancy in IPMN, which could potentially contribute to improved risk stratification and management strategies for patients.
Limitations
The present study has several limitations, including the small sample size and data collected from only one center, which may include selection bias. The inherent restrictions of retrospective design also apply, including limiting the generalization of results to other populations and not allowing the measurement of certain factors or long-term follow-up. Protocol for the systematic review and meta-analysis was not pre-recorded on PROSPERO. Data on IPMN epithelial cell subtypes were missing for some patients. Lastly, the few studies in the meta-analysis may not provide sufficient power to draw reliable conclusions. The pooled analysis also included case-control studies with a lower evidence quality.
Conclusion
The findings of our clinical data and the systematic review and meta-analysis suggest that patients with AP and IPMN are at a higher risk of presenting HGD and the intestinal type of IPMN compared to those without AP.
Data Availability
All data analyzed during this study are included in this published article.
Abbreviations
- IPMN:
-
Intraductal papillary mucinous neoplasm
- AP:
-
acute pancreatitis
- ORs:
-
odds ratios
- CIs:
-
confidence intervals
- HGD:
-
high-grade dysplasia
- LGD:
-
low-grade dysplasia
- MGD:
-
intermediate-grade dysplasia
- HGD:
-
high-grade dysplasia
- IC:
-
invasive carcinoma
References
Del Chiaro M, Verbeke C. Intraductal papillary mucinous neoplasms of the pancreas: reporting clinically relevant features. Histopathology. 2017;70(6):850–60.
Aronsson L, Andersson R, Ansari D. Intraductal papillary mucinous neoplasm of the pancreas - epidemiology, risk factors, diagnosis, and management. Scand J Gastroenterol. 2017;52(8):803–15.
Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12(3):183–97.
Bosman FTCF, Hruban RH. WHO classification of tumours of the digestive system. Volume 3, 4th ed. Lyon: International Agency for Research on Cancer; 2010.
Furukawa T, Klöppel G, Volkan Adsay N, Albores-Saavedra J, Fukushima N, Horii A, et al. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch. 2005;447(5):794–9.
Masuda A, Arisaka Y, Hara S, Matsumoto I, Takenaka M, Sakai A, et al. MUC2 expression and prevalence of high-grade dysplasia and invasive carcinoma in mixed-type intraductal papillary mucinous neoplasm of the pancreas. Pancreatology. 2013;13(6):583–8.
Koh YX, Zheng HL, Chok AY, Tan CS, Wyone W, Lim TK, et al. Systematic review and meta-analysis of the spectrum and outcomes of different histologic subtypes of noninvasive and invasive intraductal papillary mucinous neoplasms. Surgery. 2015;157(3):496–509.
Ban S, Naitoh Y, Mino-Kenudson M, Sakurai T, Kuroda M, Koyama I, et al. Intraductal papillary mucinous neoplasm (IPMN) of the pancreas: its histopathologic difference between 2 major types. Am J Surg Pathol. 2006;30(12):1561–9.
Heckler M, Brieger L, Heger U, Pausch T, Tjaden C, Kaiser J, et al. Predictive performance of factors associated with malignancy in intraductal papillary mucinous neoplasia of the pancreas. BJS Open. 2018;2(1):13–24.
Tenner S, Baillie J, DeWitt J, Vege SS. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108(9):1400–15.
Coyle WJ, Pineau BC, Tarnasky PR, Knapple WL, Aabakken L, Hoffman BJ, et al. Evaluation of unexplained acute and acute recurrent pancreatitis using endoscopic retrograde cholangiopancreatography, sphincter of Oddi manometry and endoscopic ultrasound. Endoscopy. 2002;34(8):617–23.
Mujica VR, Barkin JS, Go VL. Acute pancreatitis secondary to pancreatic carcinoma. Study Group Participants Pancreas. 2000;21(4):329–32.
Venkatesh PG, Navaneethan U, Vege SS. Intraductal papillary mucinous neoplasm and acute pancreatitis. J Clin Gastroenterol. 2011;45(9):755–8.
Jang JW, Kim MH, Jeong SU, Kim J, Park DH, Lee SS, et al. Clinical characteristics of intraductal papillary mucinous neoplasm manifesting as acute pancreatitis or acute recurrent pancreatitis. J Gastroenterol Hepatol. 2013;28(4):731–8.
Hata T, Sakata N, Okada T, Aoki T, Motoi F, Katayose Y, et al. Dilated papilla with mucin extrusion is a potential predictor of acute pancreatitis associated with intraductal papillary mucinous neoplasms of pancreas. Pancreatology. 2013;13(6):615–20.
Pelletier AL, Hammel P, Rebours V, Couvelard A, Vullierme MP, Maire F, et al. Acute pancreatitis in patients operated on for intraductal papillary mucinous neoplasms of the pancreas: frequency, severity, and clinicopathologic correlations. Pancreas. 2010;39(5):658–61.
Tsutsumi K, Ohtsuka T, Oda Y, Sadakari Y, Mori Y, Aishima S, et al. A history of acute pancreatitis in intraductal papillary mucinous neoplasms of the pancreas is a potential predictive factor for malignant papillary subtype. Pancreatology. 2010;10(6):707–12.
Shin SH, Han DJ, Park KT, Kim YH, Park JB, Kim SC. Validating a simple scoring system to predict malignancy and invasiveness of intraductal papillary mucinous neoplasms of the pancreas. World J Surg. 2010;34(4):776–83.
Morales-Oyarvide V, Mino-Kenudson M, Ferrone CR, Gonzalez-Gonzalez LA, Warshaw AL, Lillemoe KD, et al. Acute pancreatitis in intraductal papillary mucinous neoplasms: a common predictor of malignant intestinal subtype. Surgery. 2015;158(5):1219–25.
Hwang JA, Choi SY, Lee JE, Kim SS, Lee S, Moon JY, et al. Pre-operative nomogram predicting malignant potential in the patients with intraductal papillary mucinous neoplasm of the pancreas: focused on imaging features based on revised international guideline. Eur Radiol. 2020;30(7):3711–22.
Tanaka T, Masuda A, Sofue K, Toyama H, Shiomi H, Sakai A, et al. Acute pancreatitis in intraductal papillary mucinous neoplasms correlates with pancreatic volume and epithelial subtypes. Pancreatology. 2021;21(1):138–43.
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102–11.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med. 2021;18(3):e1003583.
Kosmahl M, Pauser U, Peters K, Sipos B, Lüttges J, Kremer B, et al. Cystic neoplasms of the pancreas and tumor-like lesions with cystic features: a review of 418 cases and a classification proposal. Virchows Arch. 2004;445(2):168–78.
Kirkegård J, Cronin-Fenton D, Heide-Jørgensen U, Mortensen FV. Acute Pancreatitis and Pancreatic Cancer risk: a Nationwide Matched-Cohort Study in Denmark. Gastroenterology. 2018;154(6):1729–36.
Roch AM, Parikh JA, Al-Haddad MA, DeWitt JM, Ceppa EP, House MG, et al. Abnormal serum pancreatic enzymes, but not pancreatitis, are associated with an increased risk of malignancy in patients with intraductal papillary mucinous neoplasms. Surgery. 2014;156(4):923–9.
Tanaka M, Kobayashi K, Mizumoto K, Yamaguchi K. Clinical aspects of intraductal papillary mucinous neoplasm of the pancreas. J Gastroenterol. 2005;40(7):669–75.
Engjom T, Nordaas IK, Tjora E, Dimcevski G, Haldorsen IS, Olesen SS, et al. Aetiological risk factors are associated with distinct imaging findings in patients with chronic pancreatitis: a study of 959 cases from the Scandinavian Baltic Pancreatic Club (SBPC) imaging database. Pancreatology. 2021;21(4):688–97.
Chavan SS, Pavlov VA, Tracey KJ. Mechanisms and therapeutic relevance of neuro-immune communication. Immunity. 2017;46(6):927–42.
Shahid RA, Vigna SR, Huang MN, Gunn MD, Liddle RA. Nicotinic stimulation of splenic T cells is protective in endoscopic retrograde cholangiopancreatography-induced acute pancreatitis in mice. Am J Physiol Gastrointest Liver Physiol. 2022;323(5):G420–g7.
Acknowledgements
None.
Funding
This study was supported by grants from the Key Laboratory of Malignant Tumor Molecular Mechanism and Translational Medicine of Guangzhou Bureau of Science and Information Technology (Grant [2013]163); the Key Laboratory of Malignant Tumor Gene Regulation and Target Therapy of Guangdong Higher Education Institutes (Grant KLB09001); the National Natural Science Foundation of China (No. 81270442 and No. 81970464); the Science and Technology Program of Guangzhou, China (No. 202201011066); the Science and Technology and Social Development Project of Guangdong Province (No. 2012B031800030) and the Natural Science Foundation of Guangdong Province (No. 2022A1515110529)
Author information
Authors and Affiliations
Contributions
Ji-Hao Xu: data acquisition; manuscript preparation. Chu-Yan Ni: clinical studies; manuscript preparation. Yan-Yan Zhuang: data analysis. Li Li: statistical analysis. Ying Lin: definition of intellectual content. Zhong-Sheng Xia: study concepts; manuscript review. Wei-Rong Wu: literature research. Qi-Kui Chen: data analysis; data acquisition. Wa Zhong: guarantor of integrity of the entire study; study design; manuscript editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board of Sun Yat-Sen Memorial Hospital (approval number: SYSEC-KY-KS-2021-017), and written informed consent of included patients was waived by the Institutional Review Board of Sun Yat-Sen Memorial Hospital due to the retrospective nature of the study. All methods followed the Declaration of Helsinki and relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, JH., Ni, CY., Zhuang, YY. et al. Acute pancreatitis in intraductal papillary mucinous neoplasm: a single-center retrospective cohort study with systematic review and meta-analysis. BMC Gastroenterol 23, 424 (2023). https://doi.org/10.1186/s12876-023-02972-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-02972-4