Abstract
Purpose
This study aimed to elucidate the impact of anatomic location of residual disease (RD) after initial cholecystectomy on survival following re-resection of incidental gallbladder cancer (IGBC).
Methods
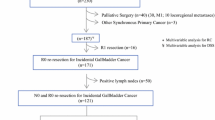
Patients with pT2 or pT3 gallbladder cancer (36 with IGBC and 171 with non-IGBC) who underwent resection were analyzed. Patients with IGBC were classified as follows according to the anatomic location of RD after initial cholecystectomy: no RD (group 1); RD in the gallbladder bed, stump of the cystic duct, and/or regional lymph nodes (group 2); and RD in the extrahepatic bile duct and/or distant sites (group 3).
Results
Timing of resection (IGBC vs. non-IGBC) did not affect survival in either multivariate or propensity score matching analysis. RD was found in 16 (44.4%) of the 36 patients with IGBC; R0 resection following re-resection was achieved in 32 patients (88.9%). Overall survival (OS) following re-resection was worse in group 3 (n = 7; 5-year OS, 14.3%) than in group 2 (n = 9; 5-year OS, 55.6%) (p = 0.035) or in group 1 (n = 20; 5-year OS, 88.7%) (p < 0.001). There was no survival difference between groups 1 and 2 (p = 0.256). Anatomic location of RD was independently associated with OS (group 2, HR 2.425, p = 0.223; group 3, HR 9.627, p = 0.024).
Conclusion
The anatomic location of RD independently predicts survival following re-resection, which is effective for locoregional disease control in IGBC, similar to resection for non-IGBC. Not all patients with RD have poor survival following re-resection for IGBC.

Similar content being viewed by others
References
Shirai Y, Yoshida K, Tsukada K, Muto T (1992) Inapparent carcinoma of the gallbladder: an appraisal of a radical second operation after simple cholecystectomy. Ann Surg 215:326–331
Søreide K, Guest RV, Harrison EM , Kendall TJ, Garden OJ, Wigmore SJ (2019) Systemic review of management of incidental gallbladder cancer after cholecystectomy. Br J Surg 106:32–45
Ethun CG, Le N, Lopez-Aguiar AG, Pawlik TM, Poultsides G, Tran T, Idrees K, Isom CA, Fields RC, Krasnick BA, Weber SM, Salem A, Martin RCG, Scoggins CR, Shen P, Mogal HD, Schmidt C, Beal E, Hatzaras I, Shenoy R, Russell MC, Maithel SK (2017) Pathologic and prognostic implications of incidental versus nonincidental gallbladder cancer: a 10-institution study from the United States Extrahepatic Biliary Malignancy Consortium. Am Surg 83:679–686
Cherkassky L, D’Angelica M (2019) Gallbladder cancer: managing the incidental diagnosis. Surg Oncol Clin N Am 28:619–630
Aloia TA, Járufe N, Javle M, Maithel SK, Roa JC, Adsay V, Coimbra FJF, Jarnagin WR (2015) Gallbladder: expert consensus statement. HPB 17:681–690
Wakai T, Shirai Y, Hatakeyama K (2002) Radical second resection provides survival benefit for patients with T2 gallbladder carcinoma first discovered after laparoscopic cholecystectomy. World J Surg 26:867–871
Wakai T, Shirai Y, Yokoyama N, Ajioka Y, Watanabe H, Hatakeyama K (2003) Depth of subserosal invasion predicts long-term survival after resection in patients with T2 gallbladder carcinoma. Ann Surg Oncol 10:447–454
Lundgren L, Muszynska C, Ros A, Persson G, Gimm O, Andersson B, Sandström P (2019) Management of incidental gallbladder cancer in a national cohort. Br J Surg 106:1216–1227
de Savornin Lohman EAJ, van der Geest LG, de Bitter TJJ, Nagtegaal ID, van Laarhoven CJHM, van den Boezem P, van der Post CS, de Reuver PR (2020) Re-resection in incidental gallbladder cancer: survival and the incidence of residual disease. Ann Surg Oncol 27:1132–1142
Fuks D, Regimbeau JM, Le Treut YP, Bachellier P, Raventos A, Pruvot FR, Chiche L, Farges O (2011) Incidental gallbladder cancer by the AFC-GBC-2009 Study Group. World J Surg 35:1887–1897
Butte JM, Waugh E, Meneses M, Parada H, de la Fuente HA (2010) Incidental gallbladder cancer: analysis of surgical findings and survival. J Surg Oncol 102:620–625
Goetze TO, Paolucci V (2010) Adequate extent in radical re-resection of incidental gallbladder carcinoma: analysis of the German Registry. Surg Endosc. 24:2156–2164
Butte JM, Kingham TP, Gönen M, D’Angelica MI, Allen PJ, Fong Y, DeMatteo RP, Jarnagin WR (2014) Residual disease predicts outcomes after definitive resection for incidental gallbladder cancer. J Am Coll Surg 219:416–429
Gil L, de Aretxabala X, Lendoire J, Duek F, Hepp J, Imventarza O (2019) Incidental gallbladder cancer: how residual disease affects outcome in two referral HPB centers from South America. World J Surg 43:214–220
Ethun CG, Postlewait LM, Le N, Pawlik TM, Buettner S, Poultsides G, Tran T, Idrees K, Isom CA, Fields RC, Jin LX, Weber SM, Salem A, Martin RC, Scoggins C, Shen P, Mogal HD, Schmidt C, Beal E, Hatzaras I, Shenoy R, Merchant N, Cardona K, Maithel SK (2017) A novel pathology-based preoperative risk score to predict locoregional residual and distant disease and survival for incidental gallbladder cancer: a 10-institution study from the U.S. Extrahepatic Biliary Malignancy Consortium. Ann Surg Oncol 24:1343–1350
Ramos E, Lluis N, Llado L, Torras J, Busquets J, Rafecas A, Serrano T, Mils K, Leiva D, Fabregat J (2020) Prognostic value and risk stratification of residual disease in patients with incidental gallbladder cancer. World J Surg Oncol 18:18
Sakata J, Kobayashi T, Tajima Y, Ohashi T, Hirose Y, Takano K, Takizawa K, Miura K, Wakai T (2017) Relevance of dissection of the posterior superior pancreaticoduodenal lymph nodes in gallbladder carcinoma. Ann Surg Oncol 24:2474–2481
Toge K, Sakata J, Hirose Y, Yuza K, Ando T, Soma D, Katada T, Miura K, Takizawa K, Kobayashi T, Wakai T (2019) Lymphatic spread of T2 gallbladder carcinoma: regional lymphadenectomy is required independent of tumor location. Eur J Surg Oncol 45:1446–1452
Japanese Society of Hepato-Biliary-Pancreatic Surgery (2013) General rules for clinical and pathological studies on cancer of the biliary tract, 6th edn. Kanehara & Co., Ltd, Tokyo
Zhu AX, Pawlik TM, Kooby DA, Schefter TE, Vauthey JN (2017) Gallbladder. In: AJCC cancer staging manual, 8th edn. Springer, New York, pp 303–309
Ishihara S, Horiguchi A, Miyakawa S, Endo I, Miyazaki M, Takada T (2016) Biliary tract cancer registry in Japan from 2008 to 2013. J Hepatobiliary Pancreat Sci 23:149–157
Birnbaum DJ, Viganò L, Ferrero A, Langella S, Russolillo N, Capussotti L (2014) Locally advanced gallbladder cancer: which patients benefit from resection? Eur J Surg Oncol 40:1008–1015
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Yao XI, Wang X, Speicher PJ, Hwang ES, Cheng P, Harpole DH, Berry MF, Schrag D, Pang HH (2017) Reporting and guidelines in propensity score analysis: a systematic review of cancer and cancer surgical studies. J Natl Cancer Inst 109:djw323
Vega EA, Vinuela E, Okuno M, Joechle K, Sanhueza M, Diaz C, Jarufe N, Martinez J, Troncoso A, Diaz A, Chun YS, Tzeng CWD, Lee JE, Vauthey JN, Conrad C (2019) Incidental versus non-incidental gallbladder cancer: index cholecystectomy before oncologic re-resection negatively impacts survival in T2b tumors. HPB 21:1046–1056
Pawlik TM, Gleisner AL, Vigano L, Kooby DA, Bauer TW, Frilling A, Adams RB, Staley CA, Trindade EN, Schulick RD, Choti MA, Capussotti L (2007) Incidence of finding residual disease for incidental gallbladder carcinoma: implications for re-resection. J Gastrointest Surg 11:1478–1487
Shih SP, Schulick RD, Cameron JL, Lillemoe KD, Pitt HA, Choti MA, Campbell KA, Yeo CJ, Talamini MA (2007) Gallbladder cancer: the role of laparoscopy and radical resection. Ann Surg 245:893–901
Shindoh J, de Aretxabala X, Aloia TA, Roa JC, Roa I, Zimmitti G, Javle M, Conrad C, Maru DM, Aoki T, Vigano L, Ribero D, Kokudo N, Capussotti L, Vauthey JN (2015) Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer: an international multicenter study. Ann Surg 261:733–739
Lee W, Jeong CY, Jang JY, Kim YH, Roh YH, Kim KW, Kang SH, Yoon MH, Seo HI, Yun SP, Park JI, Jung BH, Shin DH, Choi YI, Moon HH, Chu CW, Ryu JH, Yang K, Park YM, Hong SC (2017) Do hepatic-sided tumors require more extensive resection than peritoneal-sided tumors in patients with T2 gallbladder cancer? Results of a retrospective multicenter study. Surgery 162:515–524
Primrose JN, Fox RP, Palmer DH, Malik HZ, Prasad R, Mirza D, Anthony A, Corrie P, Falk S, Finch-Jones M, Wasan H, Ross P, Wall L, Wadsley J, Evans JTR, Stocken D, Praseedom R, Ma YT, Davidson B, Neoptolemos JP, Iveson T, Raftery J, Zhu S, Cunningham D, Garden OJ, Stubbs C, Valle JW, Bridgewater J, Primrose JN, Fox RP, Morement H, Chan O, Rees C, Ma YT, Hickish T, Falk S, Finch-Jones M, Pope I, Corrie P, Crosby T, Sothi S, Sharkland K, Adamson D, Wall L, Evans J, Dent J, Hombaiah U, Iwuji C, Anthoney A, Bridgewater J, Cunningham D, Gillmore R, Ross P, Slater S, Wasan H, Waters J, Valle JW, Palmer D, Malik H, Neoptolemos J, Faluyi O, Sumpter K, Dernedde U, Maduhusudan S, Cogill G, Archer C, Iveson T, Wadsley J, Darby S, Peterson M, Mukhtar AA, Thorpe JG, Bateman A, Tsang D, Cummins S, Nolan L, Beaumont E, Prasad R, Mirza D, Stocken D, Praseedom R, Davidson B, Raftery J, Zhu S, Garden J, Stubbs C, Coxon F (2019) Capecitabine compared with observation in resected biliary tract cancer (BILCAP): a randomised, controlled, multicentre, phase 3 study. Lancet Oncol 20:663–673
Shroff RT, Kennedy EB, Bachini M, Bekaii-Saab T, Crane C, Edeline J, el-Khoueiry A, Feng M, Katz MHG, Primrose J, Soares HP, Valle J, Maithel SK (2019) Adjuvant therapy for resected biliary tract cancer: ASCO clinical practice guideline. J Clin Oncol 37:1015–1027
Author information
Authors and Affiliations
Contributions
Study conception and design: Ando T and Sakata J; acquisition of data: Ando T, Sakata J, Hirose Y, Takano K, Takizawa K, and Miura K; analysis and interpretation of data: Ando T, Sakata J, Kobayashi T, Ichikawa H, Hanyu T, Shimada Y, and Nagahashi M; drafting of manuscript: Ando T and Sakata J; critical revision of manuscript: Nomura T, Miura K, Takizawa K, Kobayashi T, Ichikawa H, Shimada Y, Nagahashi M, Kosugi SI, and Wakai T
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the institutional review boards of Niigata University and Niigata Cancer Center Hospital. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration.
Informed consent
The need for informed consent was waived due to the retrospective observational nature of the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ando, T., Sakata, J., Nomura, T. et al. Anatomic location of residual disease after initial cholecystectomy independently determines outcomes after re-resection for incidental gallbladder cancer. Langenbecks Arch Surg 406, 1521–1532 (2021). https://doi.org/10.1007/s00423-021-02165-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02165-1