Abstract
Purpose
Onflex™ mesh has replaced Polysoft™ patch on the market, without being clinically evaluated thus far in the transinguinal preperitoneal (TIPP) technique.
Methods
All consecutive TIPP registered in our registry during the overlap period of availability of both meshes were included and studied with the chronic postoperative inguinal pain (CPIP) as primary endpoint, assessed with a verbal rating scale (VRS), and included in a patient-related outcome measurement (PROM) phone questionnaire.
Results
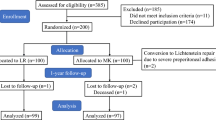
A total of 181 Onflex cases vs 182 Polysoft cases were studied with a 2-year follow-up rate of 92% vs 88%. The overall rate of pain or discomfort was not statistically different in the 2 studied subgroups (16.5% vs 17.6%; p = 0.71), while moderate or severe pain were significantly more frequent in the Polysoft subgroup (5.5% vs 11.6%; p = 0.01). These symptoms did not interfere with the patient daily life in 16% vs 16.5% of cases, and they were self-assessed as more bothersome than the hernia in only 0.5% vs 0.5% of cases, suggesting an overestimation of the pain by the VRS. Patients assessed the result of their hernia repair as excellent or good in 97.8% vs 96.7% and medium or bad in 2.2% vs 3.3% (p = 0.53). The cumulative recurrence rate was 0% vs 2.2%. Two reoperations (one for early and one for late recurrence) were reported in the Polysoft subgroup (1%), none related to the non-absorbable memory ring.
Conclusions
These results suggest that TIPP with Onflex provides results at least similar than those with Polysoft.


Similar content being viewed by others
Data availability
De-identified Excel download of the database is available for double check if needed.
References
Stoppa RE, Rives JL, Warlaumont CR, Palot JP, Verhaeghe PJ, Delattre JF (1984) The use of Dacron in the repair of hernias of the groin. Surg Clin North Am 64(2):269–285. https://doi.org/10.1016/s0039-6109(16)43284-6
Read RC, Barone GW, Hauer-Jensen M, Yoder G (1993) Properitoneal prosthetic placement through the groin. The anterior (Mahorner-Goss, Rives-Stoppa) approach. Surg Clin North Am 73(3):545–555. https://doi.org/10.1016/s0039-6109(16)46036-6
Alexandre JH, Bouillot JL, Dupin P, Aouad K, Bethoux JP (2006) Cure of inguinal hernias with large preperitoneal prosthesis: experience of 2,312 cases. J Minim Access Surg 2(3):134–138. https://doi.org/10.4103/0972-9941.27725
Ugahary A, Ugahary F (2010) Technique De Grid-Iron Ugahary®. In: Vidèo-Atlas Chirurgie Herniaire Tome 1. Springer, Paris. Vidèo-Atlas Chirurgie Herniaire Tome 1 Springer, Paris: Springer, Paris; 2010
Lange JF, Lange MM, Voropai DA, van Tilburg MW, Pierie JP, Ploeg RJ et al (2014) Trans rectus sheath extra-peritoneal procedure (TREPP) for inguinal hernia: the first 1,000 patients. World J Surg 38(8):1922–1928. https://doi.org/10.1007/s00268-014-2475-5
Kugel RD (2003) The Kugel repair for groin hernias. Surg Clin North Am 83(5):1119–1139. https://doi.org/10.1016/S0039-6109(03)00123-3
Pelissier EP, Blum D, Marre P, Damas JM (2001) Inguinal hernia: a patch covering only the myopectineal orifice is effective. Hernia. 5(2):84–87. https://doi.org/10.1007/s100290100002
Lourenco A, da Costa RS (2013) The ONSTEP inguinal hernia repair technique: initial clinical experience of 693 patients, in two institutions. Hernia. 17(3):357–364. https://doi.org/10.1007/s10029-013-1057-z
Alexandre JH, Dupin P, Levard H, Billebaud T (1984) Treatment of inguinal hernia with unsplit mersylene prosthesis. Significance of the parietalization of the spermatic cord and the ligation of epigastric vessels. Presse Med 13(3):161–163
Berrevoet F, Maes L, Reyntjens K, Rogiers X, Troisi R, de Hemptinne B (2010) Transinguinal preperitoneal memory ring patch versus Lichtenstein repair for unilateral inguinal hernias. Langenbeck's Arch Surg 395(5):557–562. https://doi.org/10.1007/s00423-009-0544-2
Berrevoet F, Vanlander A, Bontinck J, Troisi RI (2013) Open preperitoneal mesh repair of inguinal hernias using a mesh with nitinol memory frame. Hernia. 17(3):365–371. https://doi.org/10.1007/s10029-013-1110-y
Rosenberg J, Andresen K (2018) Open new simplified totally extraperitoneal (ONSTEP) technique for inguinal hernia repair. In: Campanelli G (ed) The art of hernia surgery. Springer International Publishing AG, pp 301–306. https://doi.org/10.1007/978-3-319-72626-7_30
Pelissier EP, Monek O, Blum D, Ngo P (2007) The Polysoft patch: prospective evaluation of feasibility, postoperative pain and recovery. Hernia. 11(3):229–234. https://doi.org/10.1007/s10029-007-0203-x
Pelissier EP (2006) Inguinal hernia: preperitoneal placement of a memory-ring patch by anterior approach. Preliminary experience. Hernia 10(3):248–252. https://doi.org/10.1007/s10029-006-0079-1
Gillion JF, Chollet JM (2013) Chronic pain and quality of life (QoL) after transinguinal preperitoneal (TIPP) inguinal hernia repair using a totally extraperitoneal, parietalized, Polysoft (R) memory ring patch : a series of 622 hernia repairs in 525 patients. Hernia. 17(6):683–692. https://doi.org/10.1007/s10029-013-1121-8
Sajid MS, Craciunas L, Singh KK, Sains P, Baig MK (2013) Open transinguinal preperitoneal mesh repair of inguinal hernia: a targeted systematic review and meta-analysis of published randomized controlled trials. Gastroenterol Rep (Oxf) 1(2):127–137. https://doi.org/10.1093/gastro/got002
Djokovic A, Delibegovic S (2019) Tipp versus the Lichtenstein and Shouldice techniques in the repair of inguinal hernias - short-term results. Acta Chir Belg:1–7. https://doi.org/10.1080/00015458.2019.1706323
Koning GG, Keus F, Koeslag L, Cheung CL, Avci M, van Laarhoven CJ et al (2012) Randomized clinical trial of chronic pain after the transinguinal preperitoneal technique compared with Lichtenstein’s method for inguinal hernia repair. Br J Surg 99(10):1365–1373. https://doi.org/10.1002/bjs.8862
Koning GG, de Vries J, Borm GF, Koeslag L, Vriens PW, van Laarhoven CJ (2013) Health status one year after TransInguinal PrePeritoneal inguinal hernia repair and Lichtenstein’s method: an analysis alongside a randomized clinical study. Hernia. 17(3):299–306. https://doi.org/10.1007/s10029-012-0963-9
Cadanova D, van Dijk JP, Mollen R (2017) The transinguinal preperitoneal technique (TIPP) in inguinal hernia repair does not cause less chronic pain in relation to the ProGrip technique: a prospective double-blind randomized clinical trial comparing the TIPP technique, using the PolySoft mesh, with the ProGrip self-fixing semi-resorbable mesh. Hernia. 21(1):17–27. https://doi.org/10.1007/s10029-016-1522-6
Pelissier EP, Koning GG, Ngo P (2017) Comment to: The transinguinal preperitoneal technique (TIPP) in inguinal hernia repair does not cause less chronic pain in relation to the ProGrip technique: a prospective double-blind randomized clinical trial comparing the TIPP technique, using the PolySoft mesh, with the ProGrip self-fixing semi-resorbable mesh. D. Cadanova, J. P. van Dijk, R. M. H. G. Mollen. Hernia. https://doi.org/10.1007/s10029-017-1584-0
Andresen K, Burcharth J, Fonnes S, Hupfeld L, Rothman JP, Deigaard S, Winther D, Errebo MB, Therkildsen R, Hauge D, Sørensen FS, Bjerg J, Rosenberg J (2017) Chronic pain after inguinal hernia repair with the ONSTEP versus the Lichtenstein technique, results of a double-blinded multicenter randomized clinical trial. Langenbeck's Arch Surg 402(2):213–218. https://doi.org/10.1007/s00423-016-1532-y
Oberg S, Andresen K, Hauge D, Rosenberg J (2016) Recurrence mechanisms after inguinal hernia repair by the ONSTEP technique: a case series. Hernia. 20(5):681–685. https://doi.org/10.1007/s10029-016-1496-4
Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH, Hoeferlin A, Kingsnorth AN, Mandala V, Palot JP, Schumpelick V, Simmermacher RKJ, Stoppa R, Flament JB (2007) The European Hernia Society groin hernia classification: simple and easy to remember. Hernia. 11(2):113–116. https://doi.org/10.1007/s10029-007-0198-3
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Gillion JF, Fagniez PL (1999) Chronic pain and cutaneous sensory changes after inguinal hernia repair: comparison between open and laparoscopic techniques. Hernia. 3:75–80
Aasvang E, Kehlet H (2005) Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 95(1):69–76. https://doi.org/10.1093/bja/aei019
Loos MJ, Houterman S, Scheltinga MR, Roumen RM (2008) Evaluating postherniorrhaphy groin pain: visual analogue or verbal rating scale? Hernia. 12(2):147–151. https://doi.org/10.1007/s10029-007-0301-9
Franneby U, Sandblom G, Nyren O, Nordin P, Gunnarsson U (2008) Self-reported adverse events after groin hernia repair, a study based on a national register. Value Health 11(5):927–932. https://doi.org/10.1111/j.1524-4733.2008.00330.x
Staal E, Nienhuijs SW, Keemers-Gels ME, Rosman C, Strobbe LJ (2008) The impact of pain on daily activities following open mesh inguinal hernia repair. Hernia. 12(2):153–157. https://doi.org/10.1007/s10029-007-0297-1
Molegraaf M, Lange J, Wijsmuller A (2017) Uniformity of chronic pain assessment after inguinal hernia repair: a critical review of the literature. Eur Surg Res 58(1–2):1–19. https://doi.org/10.1159/000448706
Heniford BT, Lincourt AE, Walters AL, Colavita PD, Belyansky I, Kercher KW, Sing RF, Augenstein VA (2018) Carolinas comfort scale as a measure of hernia repair quality of life: a reappraisal utilizing 3788 international patients. Ann Surg 267(1):171–176. https://doi.org/10.1097/SLA.0000000000002027
Olsson A, Sandblom G, Franneby U, Sonden A, Gunnarsson U, Dahlstrand U (2019) The short-form inguinal pain questionnaire (sf-IPQ): an instrument for rating groin pain after inguinal hernia surgery in daily clinical practice. World J Surg 43(3):806–811. https://doi.org/10.1007/s00268-018-4863-8
Lundstrom KJ, Holmberg H, Montgomery A, Nordin P (2018) Patient-reported rates of chronic pain and recurrence after groin hernia repair. Br J Surg 105(1):106–112. https://doi.org/10.1002/bjs.10652
Tsirline VB, Colavita PD, Belyansky I, Zemlyak AY, Lincourt AE, Heniford BT (2013) Preoperative pain is the strongest predictor of postoperative pain and diminished quality of life after ventral hernia repair. Am Surg 79(8):829–836
Niebuhr H, Wegner F, Hukauf M, Lechner M, Fortelny R, Bittner R et al (2018) What are the influencing factors for chronic pain following TAPP inguinal hernia repair: an analysis of 20,004 patients from the Herniamed Registry. Surg Endosc 32(4):1971–1983. https://doi.org/10.1007/s00464-017-5893-2
Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T (2012) Reoperation versus clinical recurrence rate after ventral hernia repair. Ann Surg 256(6):955–958. https://doi.org/10.1097/SLA.0b013e318254f5b9
Baucom RB, Ousley J, Feurer ID, Beveridge GB, Pierce RA, Holzman MD, Sharp KW, Poulose BK (2016) Patient reported outcomes after incisional hernia repair-establishing the ventral hernia recurrence inventory. Am J Surg 212(1):81–88. https://doi.org/10.1016/j.amjsurg.2015.06.007
Tastaldi L, Barros PHF, Krpata DM, Prabhu AS, Rosenblatt S, Petro CC, Alkhatib H, Szutan LA, Silva RA, Olson MA, Stewart TG, Roll S, Rosen MJ, Poulose BK (2019) Hernia recurrence inventory: inguinal hernia recurrence can be accurately assessed using patient-reported outcomes. Hernia 24:127–135. https://doi.org/10.1007/s10029-019-02000-z
Lopez-Cano M, Vilallonga R, Sanchez JL, Hermosilla E, Armengol M (2007) Short postal questionnaire and selective clinical examination combined with repeat mailing and telephone reminders as a method of follow-up in hernia surgery. Hernia. 11(5):397–402. https://doi.org/10.1007/s10029-007-0239-y
Bakker WJ, Roos MM, Kerkman T, Burgmans JPJ (2019) Experience with the PINQ-PHONE telephone questionnaire for detection of recurrences after endoscopic inguinal hernia repair. Hernia. 23(4):685–691. https://doi.org/10.1007/s10029-019-01909-9
Arslan K, Erenoglu B, Turan E, Koksal H, Dogru O (2015) Minimally invasive preperitoneal single-layer mesh repair versus standard Lichtenstein hernia repair for inguinal hernia: a prospective randomized trial. Hernia. 19(3):373–381. https://doi.org/10.1007/s10029-014-1306-9
Soler M (2018) Minimal Open Preperitoneal (MOPP) Technique. In: Campanelli G (ed) The art of hernia surgery. Springer, pp 319–326
Ohmura Y, Suzuki H, Kotani K, Teramoto A (2019) Laparoscopic inguinal hernia repair with a joystick-guided robotic scope holder (Soloassist II(R)): retrospective comparative study with human assistant. Langenbeck's Arch Surg 404(4):495–503. https://doi.org/10.1007/s00423-019-01793-y
Muysoms F, Van Cleven S, Kyle-Leinhase I, Ballecer C, Ramaswamy A (2018) Robotic-assisted laparoscopic groin hernia repair: observational case-control study on the operative time during the learning curve. Surg Endosc 32(12):4850–4859. https://doi.org/10.1007/s00464-018-6236-7
Acknowledgments
The authors want to thank the Club-Hernie members and the dedicated CRA for their highly scientific behavior and involvement in the registry.
Author information
Authors and Affiliations
Consortia
Contributions
The three authors have contributed to the present study and reviewed the present article. Operating surgeons: JMC, JFG, and MS. Study design, data management, and article writing: JFG.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare conflict of interest not directly related to the submitted work: they were given honorarium for TIPP pilot centers (JFG, JMC, MS) and expert honorarium (JFG), but no financial support from industry was provided for this article.
The Hernia-Club is an independent scientific institution whose objective is to assess the results of different techniques and medical devices for hernia repair. It therefore has relationships with many companies having an interest in independent evaluation of their products.
Ethical approval
The patients are informed that their de-identified data are registered and that they will be offered a phone questionnaire at different steps of their follow-up. Only the operating surgeon and the clinical research assistant are able to link the randomly allocated identifying number and the patient. The data are stored in a specialized Swiss data bank where they are protected against network intrusion. The registry complies with the requirements of the General Data Protection Regulation (GDPR), the French “Méthodologies de référence de la Commission Nationale Informatique et Liberté” (MR001, MR003) and the different specific French ethics committees.
Consent for publication
The three authors consent for publication of this article. Patients give their non-opposition (observational study) at the registration in an online database of their de-identified data further used for studies and scientific publications as displayed on the public frontpage of club-hernie.com.
Code availability
Download in Excel shape.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gillion, J.F., Soler, M., Chollet, J.M. et al. A registry-based 2-year follow-up comparative study of two meshes used in transinguinal preperitoneal (TIPP) groin hernia repair. Langenbecks Arch Surg 406, 197–208 (2021). https://doi.org/10.1007/s00423-020-01993-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01993-x