Abstract
Purpose
The aim of this systematic review was to determine the rates of failure following nonoperative management for acute sigmoid diverticulitis complicated by abscess.
Methods
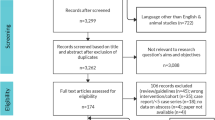
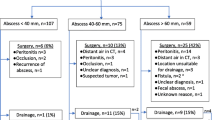
Pubmed and Medline were systematically searched by two independent researchers. Studies reporting outcomes of nonoperative management of diverticulitis with abscess revealed on CT scan were included. The endpoint of the study was failure of nonoperative management which included relapse and recurrence. Relapse was defined as development of additional complications such as peritonitis or obstruction that required urgent surgery during index admission or readmission within 30 days. Recurrence was defined as development of symptoms after an asymptomatic period of 30–90 days following nonoperative management. Nonoperative management included nil per os, intravenous fluids and antibiotics, CT-guided percutaneous drainage, and/or total parenteral nutrition.
Results
Twenty-four of 844 studies yielded by literature search totaling 12,601 patients were eligible for inclusion. Pooled relapse rate was 18.9%. The pooled rate of recurrence of acute diverticulitis was found to be 25.5%. 60.9% of recurrences were complicated diverticulitis. Failure rate appeared to be significantly increased in patients undergoing percutaneous drainage for distant abscess as compared with pericolic abscess (51% vs. 18%; p = 0.0001).
Conclusion
The rate of failure of nonoperative management was 44.4%. The rate of relapse at 30 days following nonoperative management was at 18.9%. Distant abscesses were associated with significantly increased rates of relapse compared with pericolic abscesses. The rate of recurrence following nonoperative management was 25.5% at the mean follow-up of 38 months.


Similar content being viewed by others
References
Telling WHM (1908) Acquired diverticula of the sigmoid flexure, considered especially in relation to secondary pathological processes and their clinical symptoms. Lancet 171:843–850
Schoetz DJ Jr (1999) Diverticular disease of the colon. A century-old problem. Dis Colon Rectum 42:703–709
Stollman N, Raskin JB (2004) Diverticular disease of the colon. Lancet 363(9409):631–639
Greenberg AS, Gal R, Coben RM, Cohen S, Dimarino AJ Jr (2005) A retrospective analysis of medical or surgical therapy in young patients with diverticulitis. Aliment Pharmacol Ther 21:1225–1229
Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD, Rafferty JF (2014) Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum 57:284–294
Dharmarajan S, Hunt SR, Birnbaum EH, Fleshman JW, Mutch MG (2011) The efficacy of nonoperative management of acute complicated diverticulitis. Dis Colon Rectum 54:663–671
You K, Bendl R, Sullivan TR, Gachabayov M, Bergamaschi R (2018) Randomized clinical trial of elective resection versus observation in diverticulitis with extraluminal air or abscess initially managed conservatively. Br J Surg 105:971–979
Gregersen R, Mortensen LQ, Burcharth J, Pommergaard HC, Rosenberg J (2016) Treatment of patients with acute colonic diverticulitis complicated by abscess formation: a systematic review. Int J Surg 35:201–208
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Alvarez JA, Baldonedo RF, Bear IG, Otero J, Pire G, Alvarez P, Jorge JI (2007) Presentation, management and outcome of acute sigmoid diverticulitis requiring hospitalization. Dig Surg 24:471–476
Ambrosetti P, Chauterns R, Soravia C, Peiris-Waser N, Terrier F (2005) Long-term outcome of mesocolic and pelvic diverticular abscesses of the left colon: a prospective study of 73 patients. Dis Colon Rectum 48:787–791
Bahadursingh AM, Virgo KS, Kaminski DL, Longo WE (2003) Spectrum of disease and outcome of complicated diverticular disease. Am J Surg 186:696–701
Brandt D, Gervaz P, Durmishi Y, Platon A, Morel P, Poletti PA (2006) Percutaneous CT scan-guided drainage vs. antibiotherapy alone for Hinchey II diverticulitis: a case-control study. Dis Colon Rectum 49:1533–1538
Devaraj B, Liu W, Tatum J, Cologne K, Kaiser AM (2016) Medically treated diverticular abscess associated with high risk of recurrence and disease complications. Dis Colon Rectum 59:208–215
Elagili F, Stocchi L, Ozuner G, Dietz DW, Kiran RP (2014) Outcomes of percutaneous drainage without surgery for patients with diverticular abscess. Dis Colon Rectum 57:331–336
Felder SI, Barmparas G, Lynn J, Murrell Z, Margulies DR, Fleshner P (2013) Can the need for colectomy after computed tomography-guided percutaneous drainage for diverticular abscess be predicted? Am Surg 79:1013–1016
Gaertner WB, Willis DJ, Madoff RD, Rothenberger DA, Kwaan MR, Belzer GE, Melton GB (2013) Percutaneous drainage of colonic diverticular abscess: is colon resection necessary? Dis Colon Rectum 56:622–626
Garfinkle R, Kugler A, Pelsser V, Vasilevsky CA, Morin N, Gordon P, Feldman L, Boutros M (2016) Diverticular abscess managed with long-term definitive nonoperative intent is safe. Dis Colon Rectum 59:648–655
Hachigian MP, Honickman S, Eisenstat TE, Rubin RJ, Salvati EP (1992) Computed tomography in the initial management of acute left-sided diverticulitis. Dis Colon Rectum 35:1123–1129
Jalouta T, Jrebi N, Luchtefeld M, Ogilvie JW Jr (2017) Diverticulitis recurrence after percutaneous abscess drainage. Int J Color Dis 32:1367–1373
Macias LH, Haukoos JS, Dixon MR et al (2004) Diverticulitis: truly minimally invasive management. Am Surg 70:932–935
Pautrat K, Bretagnol F, Huten N, De Calan L (2007) Acute diverticulitis in very young patients: a frequent surgical management. Dis Colon Rectum 50:472–477
Sallinen VJ, Mentula PJ, Leppäniemi AK (2014) Nonoperative management of perforated diverticulitis with extraluminal air is safe and effective in selected patients. Dis Colon Rectum 57:875–881
Singh B, May K, Coltart I, Moore NR, Cunningham C (2008) The long-term results of percutaneous drainage of diverticular abscess. Ann R Coll Surg Engl 90:297–301
Stabile BE, Puccio E, van Sonnenberg E, Neff CC (1990) Preoperative percutaneous drainage of diverticular abscesses. Am J Surg 159:99–104
Titos-García A, Aranda-Narváez JM, Romacho-López L, González-Sánchez AJ, Cabrera-Serna I, Santoyo-Santoyo J (2017) Nonoperative management of perforated acute diverticulitis with extraluminal air: results and risk factors of failure. Int J Color Dis 32:1503–1507
van de Wall BJM, Draaisma WA, Consten ECJ, van der Kaaij RT, Wiezer MJ, Broeders IAMJ (2013) Does the presence of abscesses in diverticular disease prelude surgery? J Gastrointest Surg 17:540–547
Aquina CT, Becerra AZ, Xu Z, Justiniano CF, Noyes K, Monson JRT, Fleming FJ (2019) Population-based study of outcomes following an initial acute diverticular abscess. Br J Surg 106(4):467–476
Lambrichts DPV, Bolkenstein HE, van der Does DCHE, Dieleman D, Crolla RMPH, Dekker JWT, van Duijvendijk P, Gerhards MF, Nienhuijs SW, Menon AG, de Graaf EJR, Consten ECJ, Draaisma WA, Broeders IAMJ, Bemelman WA, Lange JF (2019) Multicentre study of non-surgical management of diverticulitis with abscess formation. Br J Surg 106(4):458–466
Subhas G, Rana G, Bhullar J, Essad K, Mohey L, Mittal VK (2014) Percutaneous drainage of a diverticular abscess should be limited to two attempts for a resilient diverticular abscess. Am Surg 80(7):635–639
Trenti L, Kreisler E, Galvez A, Golda T, Frago R, Biondo S (2015) Long-term evolution of acute colonic diverticulitis after successful medical treatment. World J Surg 39(1):266–274
Lamb MN, Kaiser AM (2014) Elective resection versus observation after nonoperative management of complicated diverticulitis with abscess: a systematic review and meta-analysis. Dis Colon Rectum 57:1430–1440
Gachabayov M, Essani R, Bergamaschi R (2018) Laparoscopic approaches to complicated diverticulitis. Langenbeck’s Arch Surg 403(1):11–22
Schmidt S, Ismail T, Puhan MO, Soll C, Breitenstein S (2018) Meta-analysis of surgical strategies in perforated left colonic diverticulitis with generalized peritonitis. Langenbeck’s Arch Surg 403(4):425–433
Author information
Authors and Affiliations
Contributions
All authors have contributed to the following: substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
This is not applicable as this is a summary design study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, H., Gachabayov, M., Rojas, A. et al. Systematic review of failure of nonoperative management in complicated sigmoid diverticulitis with abscess. Langenbecks Arch Surg 405, 277–281 (2020). https://doi.org/10.1007/s00423-020-01872-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01872-5