Abstract
Purpose
The aim of the study was to examine subjective health-related quality of life (HRQoL) in patients undergoing adrenalectomy.
Methods
The study included patients scheduled for adrenalectomy 2014–2017 after giving informed consent. The SF-36 questionnaire was administrated before operation and 1 year postoperatively. Results were compared with published normative values in Sweden.
Results
Some 50 patients were included. SF-36 scores for the whole cohort improved significantly after adrenalectomy in all dimensions except for bodily pain. Compared with the general Swedish population, the patients reported a significantly reduced HRQoL before and after adrenalectomy in all domains except for bodily pain postoperatively. Patients with benign functional tumours had lower HRQoL in physical domains before adrenalectomy than patients with benign non-functional tumours; Physical Component Summary (PCS), median 33.1 (range 17.1–62.9) vs. 44.2 (20.0–66.5), p = 0.018. Postoperatively, HRQoL was similar in the two groups of patients. Patients with benign functional tumours reported significantly improved HRQoL in all dimensions after adrenalectomy: PCS 33.1 (17.1–62.9) preoperatively vs. 47.6 (19.8-57.3) postoperatively, p = 0.005; Mental Component Summary (MCS) 33.8 (11.8–62.0) preoperatively vs. 52.7 (16.4–59.8) postoperatively, p = 0.004. These improvements were not seen in patients with benign non-functional or malignant tumours. Patients with malignant tumours reported no difference in SF-36 scores before or after adrenalectomy compared with patients with benign non-functional tumours.
Conclusions
Adrenalectomy improved HRQoL in patients with benign functional tumours. Adrenalectomy did not improve HRQoL in patients with benign non-functional tumours or in patients with malignant tumours.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An increasing number of patients are being diagnosed with adrenal incidentaloma due to more frequent use and improvement in imaging. Adrenal incidentalomas increase with age [1], and the prevalence of incidentaloma in routine imaging has been reported to be 1–4% [2, 3]. Annual rates of adrenalectomy have nearly doubled since 1998 in many countries [4]. This increase in adrenal surgery has not been followed by an increase in detection of malignant adrenal disease [5], which could indicate that considerable number of patients undergo unnecessary surgery. Adrenal cortical adenoma is the most frequent pathological finding in incidentalomas [6]. Most of these benign tumours are non-functional cortical adenomas [7], but it has been suggested that these tumours can be associated with poor health outcomes [8,9,10], and possibly ameliorated by surgery[11].
Patients with hormonally inactive, small tumours with low density on computed tomography (CT) are usually not treated with surgery. Treatment for growing hormonally inactive tumours with low density on CT or small tumours with high density on CT is still debated [12].
A, sometimes, neglected aspect in patients with adrenal tumours is health-related quality of life (HRQoL) [13]. Quality of life (QoL) evaluation describes the subjective perception of the patient [14]. HRQoL is to which degree the illness or treatment affects the life of the patient [15]. There is a growing interest in QoL evaluation in patients with adrenal disease but data are very scant [13]. Previous studies have indicated reduced HRQoL in patients with adrenal tumours independent of diagnosis [16]. Kastelan et al. demonstrated impaired QoL in patients with non-functional adrenal incidentalomas compared with controls [17]. Previous reports that focused on patients with functional tumours reported an improvement in HRQoL after adrenalectomy [18].
In the view of these data, the effect of adrenalectomy on HRQoL in different adrenal conditions is of considerable interest. The aim of this study was to evaluate HRQoL in all patients undergoing adrenalectomy and to investigate the difference in the effect of adrenalectomy for patients with functioning, non-functioning and malignant tumours.
Material and methods
Study design and population
Patients undergoing unilateral adrenalectomy, at the Department of Surgery, Skåne University Hospital-Lund November 2013–March 2017 were included in the study after information and written consent. This was as part of a quality control program within the Scandinavian Quality Register for Thyroid, Parathyroid and Adrenal Surgery (SQRTPA) and thus ethical clearance was waived [19]. Patients were invited to participate in the study at their preoperative visit. They were included after returning two complete questionnaires administrated by mail 2 weeks before and at 1 year after surgery. Up to one remainder was sent to non-responders. Results were compared with values from a large sample of the general Swedish population [20].
Variables
Data extraction from SQRTPA included age, sex, indication for surgery (clinical syndrome of hormonal excess, suspected malignancy on the basis of radiological examination, preoperative diagnosed metastases, tumour size) and histopathology (adrenal cortical adenoma, adrenal cortical hyperplasia, phaeochromocytoma, myelolipoma, metastasis and other benign tumours). The transabdominal, laparoscopic robot-assisted technique was used in all patients.
Health-related quality of Life
SF-36 (36-Item Short Form Health Survey) was used to evaluate patients’ subjective perception of HRQoL. SF-36 is a self-administrated validated generic questionnaire that has been used extensively previously [21,22,23,24,25,26]. It consists of 36 questions evaluating both physical and mental health in eight health domains; physical functioning (PF), bodily pain (BP), role limitations due to physical health problems (role-physical, RP), role limitations due to personal or emotional problems (role-emotional, RE), emotional wellbeing (mental health, MH), social functioning (SF), energy or fatigue (vitality, VT) and general health perception (general health, GH). Scores range from 0 to 100 with higher values representing better QoL. The scores may be aggregated into two summary measures; Physical Component Summary (PCS) and Mental Component Summary (MCS) [27].
The primary outcomes were differences in HRQoL before and after adrenalectomy assessed by SF-36.
HRQoL depending on indication for surgery, hormonal hypersecretion and histopathology was also reported.
Statistics
Descriptive statistics are presented as number with valid percentage and mean and standard deviation (SD) or median and range, as appropriate. Preoperative and postoperative SF-36 scores were assessed using paired samples t test or Wilcoxon test where appropriate. Differences between different patient groups were evaluated using independent samples t test or Mann-Whitney U test.
Missing values were handled according to the SF-36 manual and substituted as a person-specific estimate when at least 50% of the items in a specific domain were answered [20].
Minimally important difference (MID), defined as the smallest difference in score which patients perceived as beneficial or harmful, was used to determine clinical significance [28]. According to Osoba et al., who used the questionnaire QLQ-C30 in patients with chemotherapy for breast cancer and small-cell lung cancer, differences of 5–10 points between groups on a 100-point scale were interpreted as clinically small difference, 10–20 points as moderate difference and > 20 points as large difference [29].
Analyses were conducted using IBM SPSS Statistics 25 for Windows (IBM Corporation, Armonk, NY, USA) and STATA/SE 13.1 for Mac (StataCorpLp, College Station, USA). A p value < 0.05 was considered significant.
Results
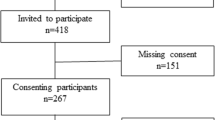
Some 161 patients underwent adrenalectomy during this time period. Fifty-nine patients returned questionnaires before adrenalectomy and at follow-up 1 year after operation. Nine patients were excluded; the first questionnaire was dated after adrenalectomy (six patients), two patients had a poor health status and were not able to complete the 1-year follow-up form, and one patient had a second operation on the contralateral adrenal before the one-year follow up.
The study flow chart is shown in Fig. 1. In all, 50 patients were included in the study. Preoperative characteristics of the cohort are summarized in Table 1. No differences were detected between the cohort and non-included patients (Supplementary Table 1).
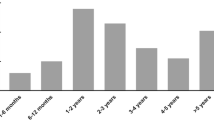
The median age was 64 (range 20–84) years, and 26 (52%) patients were women. Indication for operation could be one or several. The most common indication was a clinical syndrome of hormonal excess; 12 (24%) patients had hormonal excess of cortisol, 10 (20%) patients had hypersecretion of cathecholamines, and 5 (10%) patients had primary aldosteronism. In 4 (8%) patients, malignancy was suspected on the basis of radiological examination (CT or MRI). Seven (14%) patients had preoperatively diagnosed metastasis and 12 (24%) patients underwent surgery because of a tumour size larger than 40 mm as the sole surgical indication. The most frequent histopathological diagnoses were adrenal cortical adenoma, 26 (52%) patients, and phaeochromocytoma, 12 (24%) patients (Table 1). There were six patients with malignant tumour (metastasis from renal cancer four patients, metastasis from rectal cancer one patient and metastasis from sarcoma one patient). Mean length of hospital stay was 2.7 days, there was no reoperation and 2 (4%) patients had at least one complication.
Analysis of the whole cohort
SF-36 scores for the whole cohort before and at 1 year after adrenalectomy and compared with published normative values in Sweden [20] are shown in Table 2. The statistical precision of our findings was quantified (Supplementary Figure 1). Patients reported improved HRQoL after adrenalectomy in all dimensions except for bodily pain, mean ± SD 63.1 ± 30.7 preoperatively vs. 69.0 ± 31.5 postoperatively, p = 0.15. Compared with the general Swedish population, the patients reported significantly lower SF-36 scores both before and after adrenalectomy in all domains except for bodily pain postoperatively, which was no different compared with the general Swedish population (Table 2).
Analysis of groups based on indication for surgery and histopathology
SF-36 scores were compared in patients with benign functional and benign non-functional tumours before and after adrenalectomy, respectively. Patients with functional tumours had lower HRQoL in physical domains before adrenalectomy than patient with non-functional tumours; physical component summary functional tumours median 33.1 (range 17.1–62.9) vs. non-functional 44.2 (20.0-66.5) p = 0.018 (Table 3). Postoperatively, HRQoL was similar in the two groups of patients.
Differences between malignant and benign non-functional tumours were investigated. A lower HRQoL was only found for physical functioning in malignant tumours after adrenalectomy; malignant tumour median 67.5 (range 0-95) vs. benign non-functional tumour 85 (0–100), p = 0.049 (Supplementary Table 2).
Patients with benign functional tumours reported significantly improved HRQoL in all dimensions after adrenalectomy: Physical Component Summary 33.1 (17.1–62.9) preoperatively vs. 47.6 (19.8–57.3) postoperatively, p = 0.005; Mental Component Summary preoperatively 33.8 (11.8–62.0) vs. 52.7 (16.4–59.8) postoperatively, p = 0.004 (Table 4). These improvements were not seen in patients with benign non-functional tumours (Table 5).
In the six patients operated due to malignant tumours, there was no improvement in either Physical or Mental Component Summary score: Physical Component Summary 41.8 (20.5–53.2) preoperatively vs. 34.7 (16.2–53.9) postoperatively, p = 0.116; Mental Component Summary 54.5 (32.1–61.7) preoperatively vs. 56.6 (36.5–60.9) postoperatively, p = 0.345 (Supplementary Table 2).
When comparing patients with benign functional tumours with the general Swedish population, they had significantly lower SF-36 scores both before and after adrenalectomy (Table 6).
Patients with malignant tumours had lower SF-36 scores in four of eight dimensions before surgery compared with the general population; physical functioning malignant mean ± SD 62.5 ± 29.8 vs. general population 87.9 ± 19.6 p = 0.002, role-physical 54.2 ± 51.0 vs. 83.2 ± 31.8 p = 0.026, general health 56.0 ± 25.8 vs. 75.8 ± 22.2 p = 0.029 and role-emotional 55.6 ± 50.2 vs. 85.7 ± 29.2 p = 0.012. The difference remained after adrenalectomy except for the domain role-emotional.
Compared with the general Swedish population, patients with benign non-functional tumours had significantly reduced HRQoL before adrenalectomy except for bodily pain, mean ± SD benign non-functional 77.2 ± 29.2 vs. general population 74.8 ± 26.1 p = 0.772. Postoperatively, significant differences remained only in the domains social functioning and role-emotional.
Discussion
In the last decade, the prevalence of adrenal incidentaloma has increased, making the management of adrenal tumours an important aspect of health care. A positive outcome is not only measured by a survival benefit and cure but also by preventing morbidity and by subjective wellbeing of the patients [30]. There are few data on the impact of adrenalectomy on HRQoL in patients with adrenal tumours. Theoretically, HRQoL in patients with small, benign non-functional tumours should not differ from the normal population.
In this cohort of consisting 50 patients with a variety of functional and histological diagnosis, HRQoL improved after adenalectomy. However, compared with the Swedish general population, the patients reported lower SF-36 values both preoperatively and postoperatively. These differences were also deemed clinically significant with more pronounced differences preoperatively.
Patients with benign functional tumours reported lower HRQoL preoperatively when compared with patients with benign non-functional tumours.
Interestingly, no major differences could be detected between patients with malignant and benign non-functional tumours. Thus, patients with benign non-functional tumours reported lower SF-36 scores in mental dimensions and patients with malignant tumours in physical dimensions. The psychological aspects of the disease, e.g. anxiety and fear of malignant disease, may affect HRQoL. Also, small abnormalities in hormonal secretion could be associated with poor health outcomes [31, 32]. In the study cohort, no patients with adrenocortical cancer were detected.
When analyzing the cohort in subgroups, significant improvements in SF-36 scores were only seen in patients with benign functional tumours. The clinical relevance of these results was interpreted as being of moderate or large MID.
Data on HRQoL in patients with tumours in the adrenals are scant [13]. In a case-control study, Kastelan et al. demonstrated reduced quality of life in patients with adrenal incidentalomas compared with age- and sex-matched controls [17]. Brunaud et al. reported lower QoL, estimated by SF-36, in patients with adrenal tumours before adrenalectomy and at 6-weeks follow-up compared with the French general population [16]. During this short time frame, no significant improvement after adrenalectomy could be observed. Previous reports that focused on patients with subclinical Cushing’s syndrome (SCS) reported that adrenalectomy led to an improvement in HRQoL [31, 33]. Similar results have been shown for primary aldosteronism with Conn’s adenoma [18, 34, 35]. These results are in agreement with the results in the previous study. Thus, patients with functional tumours benefited from adrenalectomy with an improvement in HRQoL as estimated by SF-36. However, statistical significance does not equal clinical significance. Clinical significance is rarely commented on in reports on QoL in patients with adrenal tumours [13]. In the present investigation, clinical significance was defined according to Osoba et al. [29]. The results showed that minimal important differences mirrored statistical significance with large differences in SF-36 preoperatively compared with the general Swedish population and with large improvements in HRQoL in patients with benign functional tumours postoperatively.
There are some limitations to the present study. General instruments like SF-36 might not be sensitive enough to grasp the full perspective of patients with a variety of adrenal tumours. Furthermore, SF-36 is a generic instrument, i.e. not disease-specific. Ideally SF-36 should be combined with a tailored questionnaire depending on diagnosis for a greater in-depth knowledge of HRQoL. However, at present, disease-specific instruments are only available for patients with Cushing’s disease [13].
Comorbidity could be associated with poorer HRQoL. These variables were not taken into consideration in the present study. No detailed long-term follow-up was performed after the first outpatient visit 4–6 weeks after adrenalectomy. Only 37% of patients undergoing adrenalectomy during the time period were included in the study. This could lead to inclusion bias. However, this patient group was not different compared with the patients not included the same period.
However, patients with non-functional cortical tumours have been suggested to have an increased risk for the so-called metabolic syndrome, including hypertension and diabetes and cardiovascular risk [8,9,10, 36, 37], and an improvement of some aspects may be suggested after adrenalectomy [11]. If so, this does not seem to be reflected by an improvement in HRQoL, as shown in the present study.
The strength of the present study is that HRQoL was measured with the well-validated questionnaire SF-36, and results were compared with a sample of the general Swedish population as a reference group. Follow-up was performed at 12 months postoperatively when laboratory and clinical stabilization could be expected.
Conclusion
Within the context of these limitations, the present study shows that adrenalectomy improved HRQoL in patients with benign functional tumours. Adrenalectomy did not improve HRQoL in patients with benign non-functional tumours or malignant tumours.
References
Kloos RT, Gross MD, Francis IR, Korobkin M, Shapiro B (1995) Incidentally discovered adrenal masses. Endocr Rev 16(4):460–484
Bovio S, Cataldi A, Reimondo G, Sperone P, Novello S, Berruti A, Borasio P, Fava C, Dogliotti L, Scagliotti GV, Angeli A, Terzolo M (2006) Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J Endocrinol Investig 29(4):298–302
Davenport C, Liew A, Doherty B, Win HH, Misran H, Hanna S, Kealy D, al-Nooh F, Agha A, Thompson CJ, Lee M, Smith D (2011) The prevalence of adrenal incidentaloma in routine clinical practice. Endocrine 40(1):80–83
Gallagher SF et al (2007) Trends in adrenalectomy rates, indications, and physician volume: A statewide analysis of 1816 adrenalectomies. Surgery 142(6):1011–1021
Lafemina J, Brennan MF (2012) Adrenocortical carcinoma: past, present, and future. J Surg Oncol 106(5):586–594
Mansmann G, Lau J, Balk E, Rothberg M, Miyachi Y, Bornstein SR (2004) The clinically inapparent adrenal mass: update in diagnosis and management. Endocr Rev 25(2):309–340
Barzon L, Sonino N, Fallo F, Palu G, Boscaro M (2003) Prevalence and natural history of adrenal incidentalomas. Eur J Endocrinol 149(4):273–285
Ribeiro Cavalari EM, et al (2018) Nonfunctioning adrenal incidentaloma: a novel predictive factor for metabolic syndrome. 586–595
Arruda M, Mello Ribeiro Cavalari E, Pessoa de Paula M, Fernandes Cordeiro de Morais F, Furtado Bilro G, Alves Coelho MC, de Oliveira E Silva de Morais NA, Choeri D, Moraes A, Vieira Neto L (2017) The presence of nonfunctioning adrenal incidentalomas increases arterial hypertension frequency and severity, and is associated with cortisol levels after dexamethasone suppression test. J Hum Hypertens 32(1):3–11
Cansu GB, Sarı R, Yılmaz N, Özdem S, Çubuk M (2017) Markers of subclinical cardiovascular disease in nonfunctional adrenal incidentaloma patients without traditional cardiovascular risk factors. Exp Clin Endocrinol Diabetes 125(1):57–63
Midorikawa S, Sanada H, Hashimoto S, Suzuki T, Watanabe T (2001) The improvement of insulin resistance in patients with adrenal incidentaloma by surgical resection. Clin Endocrinol 54(6):797–804
Dinnes J, Bancos I, Ferrante di Ruffano L, Chortis V, Davenport C, Bayliss S, Sahdev A, Guest P, Fassnacht M, Deeks JJ, Arlt W (2016) Imaging for the diagnosis of malignancy in incidentally discovered adrenal masses: a systematic review and meta-analysis. Eur J Endocrinol 175(2):R51–R64
Ho W, Druce M (2018) Quality of life in patients with adrenal disease: a systematic review. Clin Endocrinol 89(2):119–128
The World Health Organization Quality of Life Assessment (WHOQOL) (1982) Development and general psychometric properties. Soc Sci Med 46(12):1569–1585
Fayers PM, Machin D (2016) Quality of life : the assessment, analysis, and reporting of patient-reported outcomes, vol 2016, 3rd edn. John Wiley & Sons Inc., Chichester
Brunaud L, Bresler L, Zarnegar R, Ayav A, Cormier L, Tretou S, Boissel P (2004) Does robotic adrenalectomy improve patient quality of life when compared to laparoscopic adrenalectomy? World J Surg 28(11):1180–1185
Kastelan D, Dzubur F, Dusek T, Poljicanin T, Crncevic-Orlic Z, Kraljevic I, Solak M, Bencevic T, Aganovic I, Knezevic N, Kastelan Z, Korsic M (2011) Health-related quality of life and fatigue in patients with adrenal incidentaloma. Endocrine 40(1):84–89
Sukor N, Kogovsek C, Gordon RD, Robson D, Stowasser M (2010) Improved quality of life, blood pressure, and biochemical status following laparoscopic adrenalectomy for unilateral primary aldosteronism. J Clin Endocrinol Metab 95(3):1360–1364
Scandinavian Quality Register of Thyroid Parathyroid and Adrenal Surgery. https://sqrtpa.se
Sullivan M et al (2002) SF-36 hälsoenkät : svensk manual och tolkningsguide = (Swedish manual and interpretation guide). Sahlgrenska sjukhuset, Sektionen för vårdforskning, Göteborg 2. uppl
McHorney CA, Ware JE Jr, Raczek AE (1993) The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 3:247
McHorney CA et al (1994) The MOS 36-Item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care 1:40
Ware JE Jr, Sherbourne CD (1992) The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care 6:473
Persson LO, Karlsson J, Bengtsson C, Steen B, Sullivan M (1998) The Swedish SF-36 Health Survey II. Evaluation of clinical validity: results from population studies of elderly and women in Gothenborg. J Clin Epidemiol 51(11):1095–1103
Sullivan M, Karlsson J (1998) The Swedish SF-36 Health Survey III. Evaluation of criterion-based validity: results from normative population. J Clin Epidemiol 51(11):1105–1113
Sullivan M, Karlsson J, Ware JE Jr (1995) The Swedish SF-36 Health Survey--I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med 41(10):1349–1358
Ware JE Jr (1998) and B. Gandek, Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol 51(11):903–912
Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Norman GR, Clinical Significance Consensus Meeting Group (2002) Methods to explain the clinical significance of health status measures. Mayo Clin Proc 77(4):371–383
Osoba D et al (1998) Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 16(1):139–144
Guyatt GH, Ferrans CE, Halyard MY, Revicki DA, Symonds TL, Varricchio CG, Kotzeva A, Valderas JM, Alonso J, Clinical Significance Consensus Meeting Group (2007) Exploration of the value of health-related quality-of-life information from clinical research and into clinical practice. Mayo Clin Proc 82(10):1229–1239
Toniato A, Merante-Boschin I, Opocher G, Pelizzo MR, Schiavi F, Ballotta E (2009) Surgical versus conservative management for subclinical Cushing syndrome in adrenal incidentalomas: a prospective randomized study. Ann Surg 249(3):388–391
Bancos I, Alahdab F, Crowley RK, Chortis V, Delivanis DA, Erickson D, Natt N, Terzolo M, Arlt W, Young WF Jr, Murad MH (2016) THERAPY OF ENDOCRINE DISEASE: Improvement of cardiovascular risk factors after adrenalectomy in patients with adrenal tumors and subclinical Cushing’s syndrome: a systematic review and meta-analysis. Eur J Endocrinol 175(6):R283–R295
Iacobone M, Citton M, Viel G, Boetto R, Bonadio I, Mondi I, Tropea S, Nitti D, Favia G (2012) American Association of Endocrine Surgeon: adrenalectomy may improve cardiovascular and metabolic impairment and ameliorate quality of life in patients with adrenal incidentalomas and subclinical Cushing’s syndrome. Surgery 152:991–997
Velema M, Dekkers T, Hermus A, Timmers H, Lenders J, Groenewoud H, Schultze Kool L, Langenhuijsen J, Prejbisz A, van der Wilt G, Deinum J, SPARTACUS investigators (2018) Quality of life in primary aldosteronism: a comparative effectiveness study of adrenalectomy and medical treatment. J Clin Endocrinol Metab 103(1):16–24
Citton M et al (2019) Effect of unilateral adrenalectomy on the quality of life of patients with lateralized primary aldosteronism. BMC Surg S1:1
Comlekci A, Yener S, Ertilav S, Secil M, Akinci B, Demir T, Kebapcilar L, Bayraktar F, Yesil S, Eraslan S (2010) Adrenal incidentaloma, clinical, metabolic, follow-up aspects: single centre experience. Endocrine 37(1):40–46
Barutçu S et al (2014) Non functioning adrenal incidentalomas may be associated with insulin resistance. J Clin Exp Investig 4:589
Funding
Open access funding provided by Lund University. This research was supported by Skåne Regional Research and Development Fund, Skåne University Hospital Foundation, Skåne University Hospital and Lund University
Author information
Authors and Affiliations
Contributions
Lo Hallin Thompson participated in the study conception and design, acquisition of data, analysis and interpretation of data, and drafting of manuscript. Erik Nordenström participated in the study conception and design, and critical revision of manuscript. Martin Almquist participated in the critical revision of manuscript. Anders Bergenfelz participated in the study conception and design, analysis and interpretation of data, and critical revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Quality control and analysis of PROM were performed according to Swedish legislations for health care providers, and ethical approval was therefore accordingly void.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 146 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Thompson, L.H., Nordenström, E., Almquist, M. et al. Health-related quality of life in patients undergoing adrenalectomy: report from a Swedish National Audit. Langenbecks Arch Surg 404, 807–814 (2019). https://doi.org/10.1007/s00423-019-01844-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-019-01844-4