Abstract
Purpose
3D imaging is an upcoming technology in laparoscopic surgery, and recent studies have shown that the modern 3D technique is superior in an experimental setting. However, the first randomized controlled clinical trial in this context dates back to 1998 and showed no significant difference between 2D and 3D visualization using the first 3D generation technique, which is now more than 15 years old.
Methods
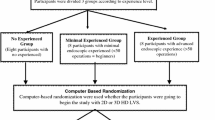
Positive results measured in an experimental setting considering 3D imaging on surgical performance led us to initiate a randomized controlled pragmatic clinical trial to validate our findings in daily clinical routine. Standard laparoscopic operations (cholecystectomy, appendectomy) were preoperatively randomized to a 2D or 3D imaging system. We used a surgical comfort scale (Likert scale) and the Raw NASA Workload TLX for the subjective assessment of 2D and 3D imaging; the duration of surgery was also measured.
Results
The results of 3D imaging were statistically significant better than 2D imaging concerning the parameters “own felt safety” and “task efficiency”; the difficulty level of the procedures in the 2D and 3D groups did not differ. Overall, the Raw NASA Workload TLX showed no significance between the groups.
Conclusion
3D imaging could be a possible advantage in laparoscopic surgery. The results of our clinical trial show increased personal felt safety and efficiency of the surgeon using a 3D imaging system. Overall of the procedures, the findings assessed using Likert scales in terms of own felt safety and task efficiency were statistically significant for 3D imaging. The individually perceived workload assessed with the Raw NASA TLX shows no difference. Although these findings are subjective impressions of the performing surgeons without a clear benefit for 3D technology in clinical outcome, we think that these results show the capability that 3D laparoscopy can have a positive impact while performing laparoscopic procedures.



Similar content being viewed by others
References
Hanna GB, Shimi SM, Cuschieri A (1998) Randomised study of influence of two-dimensional versus three-dimensional imaging on performance of laparoscopic cholecystectomy. Lancet 351:248–251. https://doi.org/10.1016/S0140-6736(97)08005-7
Gurusamy K, Samraj K, Davidson BR (2008) Three dimensional versus two dimensional imaging for laparoscopic cholecystectomy. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD006882
McLachlan G (2011) From 2D to 3D: the future of surgery? Lancet 378:1368. https://doi.org/10.1016/S0140-6736(11)61597-3
Buia A, Stockhausen F, Filmann N, Hanisch E (2017) 3D vs. 2D imaging in laparoscopic surgery—an advantage? Results of standardised black box training in laparoscopic surgery. Langenbeck's Arch Surg 402:167–171. https://doi.org/10.1007/s00423-016-1526-9
Sedgwick P (2014) Explanatory trials versus pragmatic trials. BMJ 349:g6694–g6694. https://doi.org/10.1136/bmj.g6694
Hart SG, Staveland LE (1986) Development of NASA-TLX (Task Load Index): results of empirical and theoretical research. NASA-Ames Res, Cent
Hart SG (2006) Nasa-Task Load Index (NASA-TLX); 20 years later. Proc Hum Factors Ergon Soc Annu Meet 50:904–908. https://doi.org/10.1177/154193120605000909
Gómez-Gómez E, Carrasco-Valiente J, Valero-Rosa J, Campos-Hernández JP, Anglada-Curado FJ, Carazo-Carazo JL, Font-Ugalde P, Requena-Tapia MJ (2015) Impact of 3D vision on mental workload and laparoscopic performance in inexperienced subjects. Actas Urol Esp (English Ed) 39:229–235. https://doi.org/10.1016/j.acuroe.2015.03.006
Özsoy M, Kallidonis P, Kyriazis I, Panagopoulos V, Vasilas M, Sakellaropoulos GC, Liatsikos E (2015) Novice surgeons: do they benefit from 3D laparoscopy? Lasers Med Sci 30:1325–1333. https://doi.org/10.1007/s10103-015-1739-0
Johnson KE, Tachibana C, Coronado GD, Dember LM, Glasgow RE, Huang SS, Martin PJ, Richards J, Rosenthal G, Septimus E, Simon GE, Solberg L, Suls J, Thompson E, Larson EB (2014) A guide to research partnerships for pragmatic clinical trials. BMJ 349:g6826–g6826. https://doi.org/10.1136/bmj.g6826
Tanagho YS, Andriole GL, Paradis AG, Madison KM, Sandhu GS, Varela JE, Benway BM (2012) 2D versus 3D visualization: impact on laparoscopic proficiency using the fundamentals of laparoscopic surgery skill set. J Laparoendosc Adv Surg Tech 22:121016060844000. https://doi.org/10.1089/lap.2012.0220
Smith R, Day a, Rockall T, Ballard K, Bailey M, Jourdan I (2012) Advanced stereoscopic projection technology significantly improves novice performance of minimally invasive surgical skills. Surg Endosc 26:1522–1527. https://doi.org/10.1007/s00464-011-2080-8
Lusch A, Bucur PL, Menhadji AD, Okhunov Z, Liss MA, Perez-Lanzac A, McDougall EM, Landman J (2014) Evaluation of the impact of three-dimensional vision on laparoscopic performance. J Endourol 28:261–266. https://doi.org/10.1089/end.2013.0344
Currò G, La Malfa G, Caizzone A, Rampulla V, Navarra G (2015) Three-dimensional (3D) versus two-dimensional (2D) laparoscopic bariatric surgery: a single-surgeon prospective randomized comparative study. Obes Surg:1–5. https://doi.org/10.1007/s11695-015-1674-y
Smith R, Schwab K, Day A, Rockall T, Ballard K, Bailey M, Jourdan I (2014) Effect of passive polarizing three-dimensional displays on surgical performance for experienced laparoscopic surgeons. Br J Surg 101:1453–1459. https://doi.org/10.1002/bjs.9601
Storz P, Buess GF, Kunert W, Kirschniak A (2012) 3D HD versus 2D HD: surgical task efficiency in standardised phantom tasks. Surg Endosc 26:1454–1460. https://doi.org/10.1007/s00464-011-2055-9
Bagan P, De Dominicis F, Hernigou J, Dakhil B, Zaimi R, Pricopi C, Le Pimpec Barthes F, Berna P (2015) Complete thoracoscopic lobectomy for cancer: comparative study of three-dimensional high-definition with two-dimensional high-definition video systems. Interact Cardiovasc Thorac Surg:1–4. https://doi.org/10.1093/icvts/ivv031
Ashraf a, Collins D, Whelan M, O’Sullivan R, Balfe P (2015) Three-dimensional (3D) simulation versus two-dimensional (2D) enhances surgical skills acquisition in standardised laparoscopic tasks: a before and after study. Int J Surg 14:12–16. https://doi.org/10.1016/j.ijsu.2014.12.020
Cicione A, Autorino R, Breda A, De Sio M, Damiano R, Fusco F, Greco F, Carvalho-Dias E, Mota P, Nogueira C, Pinho P, Mirone V, Correia-Pinto J, Rassweiler J, Lima E (2013) Three-dimensional vs standard laparoscopy: comparative assessment using a validated program for laparoscopic urologic skills. Urology 82:1444–1450. https://doi.org/10.1016/j.urology.2013.07.047
Chiu CJ, Lobo Prabhu K, Tan-Tam CC-H, Panton ONM, Meneghetti A (2015) Using three-dimensional laparoscopy as a novel training tool for novice trainees compared with two-dimensional laparoscopy. Am J Surg 209:824–827.e1. https://doi.org/10.1016/j.amjsurg.2015.01.007
Usta T a., Ozkaynak A, Kovalak E, Ergul E, Naki MM, Kaya E (2014) An assessment of the new generation three-dimensional high definition laparoscopic vision system on surgical skills: a randomized prospective study. Surg Endosc. https://doi.org/10.1007/s00464-014-3949-0
Nolan GJ, Howell S, Hewett P (2015) Impact of three-dimensional imaging in acquisition of laparoscopic skills in novice operators. J Laparoendosc Adv Surg Tech A 25:301–304. https://doi.org/10.1089/lap.2014.0608
Nickel F, Hendrie JD, Kowalewski KF, Bruckner T, Garrow CR, Mantel M, Kenngott HG, Romero P, Fischer L, Müller-Stich BP (2016) Sequential learning of psychomotor and visuospatial skills for laparoscopic suturing and knot tying-a randomized controlled trial (The Shoebox Study) DRKS00008668. Langenbeck's Arch Surg:1–9. https://doi.org/10.1007/s00423-016-1421-4
Sakata S, Watson AMO, Grove APM, Stevenson ARL, Fracs A (2016) The conflicting evidence of three-dimensional displays in laparoscopy. A Review of Systems Old and New. Ann Surg 263:234–239. https://doi.org/10.1097/SLA.0000000000001504
Sakata S, Grove PM, Hill A, Watson MO, Stevenson ARL (2016) The viewpoint-specific failure of modern 3D displays in laparoscopic surgery. Langenbeck's Arch Surg 401:1007–1018. https://doi.org/10.1007/s00423-016-1495-z
Sakata S, Grove PM, Watson MO, Stevenson ARL (2017) The impact of crosstalk on three-dimensional laparoscopic performance and workload. Surg Endosc:1–7. https://doi.org/10.1007/s00464-017-5449-5
Currò G, La Malfa G, Lazzara S, Caizzone A, Fortugno A, Navarra G (2015) Three-dimensional versus two-dimensional laparoscopic cholecystectomy: is surgeon experience relevant? J Laparoendosc Adv Surg Tech A 25:566–570. https://doi.org/10.1089/lap.2014.0641
Probst P, Knebel P, Grummich K, Tenckhoff S, Ulrich A, Büchler MW, Diener MK (2015) Industry bias in randomized controlled trials in general and abdominal surgery. Ann Surg 264:1. https://doi.org/10.1097/SLA.0000000000001372
Author information
Authors and Affiliations
Contributions
Buia, A., Stockhausen, F., Filmann, N., and Hanisch, E. solely contributed to this paper.
Corresponding author
Ethics declarations
Technical support
The study was supported by the Olympus Corp., Hamburg, Germany.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Conflict of interest
The authors declare that they have no conflicts of interest.
Appendices
Appendix 1


Appendix 2—NASA Task Load Index

Rights and permissions
About this article
Cite this article
Buia, A., Stockhausen, F., Filmann, N. et al. 2D vs. 3D imaging in laparoscopic surgery—results of a prospective randomized trial. Langenbecks Arch Surg 402, 1241–1253 (2017). https://doi.org/10.1007/s00423-017-1629-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-017-1629-y