Abstract
Purpose
The treatment of choice for duodenal neuroendocrine tumors (NETs) ranges from endoscopic resection and local excision to pancreaticoduodenectomy. The aim of this study was to investigate the optimal treatment for this tumor.
Methods
We retrospectively analyzed the clinicopathological data of 14 patients with NETs in the second portion of the duodenum who underwent surgery in our hospital from 2000 to 2015. The duodenal NETs were classified as either ampullary or non-ampullary. Additionally, a systematic review and pooled analysis was conducted.
Results
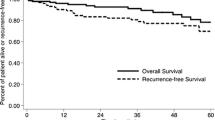
Among eight patients with ampullary NETs and six patients with non-ampullary NETs, seven and three patients underwent pancreaticoduodenectomy and one and three patients underwent local resection, respectively. The maximum tumor diameter were 11–30 mm in ampullary and 10–100 mm in non-ampullary NETs, respectively. In patients with ampullary NETs, lymph node metastases were suspected in only three cases preoperatively, but five patients actually had regional nodal metastases. Among patients with non-ampullary NETs, lymph node metastases were suspected in none preoperatively, but three of the four patients who underwent lymph node dissection had regional nodal metastases. According to a pooled analysis of 1245 patients in 88 studies, even small tumors confined to the submucosal layer and G1 tumors—ampullary and non-ampullary—have been associated with lymph node metastases. In patients with non-ampullary NETs and lymph node metastasis, 10-year recurrence-free survival rate was 51% for patients who underwent pancreaticoduodenectomy (n = 19) and 53% for patients who underwent partial duodenal resection (n = 9), respectively (p = 0.960).
Conclusion
Lymph node metastases were common in association with both ampullary and non-ampullary NETs, and it was difficult to radiologically diagnose metastases. Additionally, there were no clinicopathological factors that could reliably predict the absence of lymph node metastases preoperatively. Therefore, to maximize the ability to achieve a curative resection, pancreaticoduodenectomy is considered appropriate in well-conditioned patients with NETs in the second portion of the duodenum. However, to further clarify the impact of lymph node dissection on survival after duodenal NET resection, a multi-institutional study with a large number of patients, thorough examination of lymph node metastasis, and a long observation period is warranted.





Similar content being viewed by others
References
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A, Evans DB (2008) One hundred years after "carcinoid": epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 26(18):3063–3072
Oberndorfer S (1907) Karzinoide Tumoren des Dünndarms. Frankf Z Pathol 1:425–432
WHO (2010) Classification of Tumours of the Digestive System. 4th ed: WHO PRESS
Ito T, Sasano H, Tanaka M, Osamura RY, Sasaki I, Kimura W, Takano K, Obara T, Ishibashi M, Nakao K, Doi R, Shimatsu A, Nishida T, Komoto I, Hirata Y, Nakamura K, Igarashi H, Jensen RT, Wiedenmann B, Imamura M (2010) Epidemiological study of gastroenteropancreatic neuroendocrine tumors in Japan. J Gastroenterol 45(2):234–243
Delle Fave G, Kwekkeboom DJ, Van Cutsem E, Rindi G, Kos-Kudla B, Knigge U, Sasano H, Tomassetti P, Salazar R, Ruszniewski P, Barcelona Consensus Conference p (2012) ENETS Consensus Guidelines for the management of patients with gastroduodenal neoplasms. Neuroendocrinology 95(2):74–87
Soga J (2003) Endocrinocarcinomas (carcinoids and their variants) of the duodenum. An evaluation of 927 cases. J Exp Clin Cancer Res 22(3):349–363
Witzigmann H, Loracher C, Geissler F, Wagner T, Tannapfel A, Uhlmann D, Caca K, Hauss J, Hehl JA (2002) Neuroendocrine tumours of the duodenum. Clinical aspects, pathomorphology and therapy. Langenbeck’s Arch Surg 386(7):525–533
Clements WM, Martin SP, Stemmerman G, Lowy AM (2003) Ampullary carcinoid tumors: rationale for an aggressive surgical approach. J Gastrointest Surg 7(6):773–776
Hartel M, Wente MN, Sido B, Friess H, Buchler MW (2005) Carcinoid of the ampulla of Vater. J Gastroenterol Hepatol 20(5):676–681
Makhlouf HR, Burke AP, Sobin LH (1999) Carcinoid tumors of the ampulla of Vater: a comparison with duodenal carcinoid tumors. Cancer 85(6):1241–1249
Untch BR, Bonner KP, Roggin KK, Reidy-Lagunes D, Klimstra DS, Schattner MA, Fong Y, Allen PJ, D’Angelica MI, DeMatteo RP, Jarnagin WR, Kingham TP, Tang LH (2014) Pathologic grade and tumor size are associated with recurrence-free survival in patients with duodenal neuroendocrine tumors. J Gastrointest Surg 18(3):457–462
National_Comprehensive_Cancer_Network (2016) Neuroendocrine Tumors Version 2.2016
Miyazaki M, Ohtsuka M, Miyakawa S, Nagino M, Yamamoto M, Kokudo N, Sano K, Endo I, Unno M, Chijiiwa K, Horiguchi A, Kinoshita H, Oka M, Kubota K, Sugiyama M, Uemoto S, Shimada M, Suzuki Y, Inui K, Tazuma S, Furuse J, Yanagisawa A, Nakanuma Y, Kijima H, Takada T (2015) Classification of biliary tract cancers established by the Japanese Society of Hepato-Biliary-Pancreatic Surgery: 3(rd) English edition. J Hepatobiliary Pancreat Sci 22(3):181–196
TNM (2009) Classifacation of Malignat Tumours. 7 th ed: Wiley-Blackwell
Scherubl H, Jensen RT, Cadiot G, Stolzel U, Kloppel G (2010) Neuroendocrine tumors of the small bowels are on the rise: early aspects and management. World J Gastrointest Endosc 2(10):325–334
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M, International Study Group on Pancreatic Fistula D (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13
Lee JH, Lee KG, Ha TK, Jun YJ, Paik SS, Park HK, Lee KS (2011) Pattern analysis of lymph node metastasis and the prognostic importance of number of metastatic nodes in ampullary adenocarcinoma. Am Surg 77(3):322–329
Rose DM, Hochwald SN, Klimstra DS, Brennan MF (1996) Primary duodenal adenocarcinoma: a ten-year experience with 79 patients. J Am Coll Surg 183(2):89–96
Winter JM, Cameron JL, Olino K, Herman JM, de Jong MC, Hruban RH, Wolfgang CL, Eckhauser F, Edil BH, Choti MA, Schulick RD, Pawlik TM (2010) Clinicopathologic analysis of ampullary neoplasms in 450 patients: implications for surgical strategy and long-term prognosis. J Gastrointest Surg 14(2):379–387
Kato Y, Takahashi S, Kinoshita T, Shibasaki H, Gotohda N, Konishi M (2014) Surgical procedure depending on the depth of tumor invasion in duodenal cancer. Jpn J Clin Oncol 44(3):224–231
Kachare SD, Liner KR, Vohra NA, Zervos EE, Fitzgerald TL (2014) A modified duodenal neuroendocrine tumor staging schema better defines the risk of lymph node metastasis and disease-free survival. Am Surg 80(8):821–826
Carter JT, Grenert JP, Rubenstein L, Stewart L, Way LW (2009) Neuroendocrine tumors of the ampulla of Vater: biological behavior and surgical management. Arch Surg 144(6):527–531
Mullen JT, Wang H, Yao JC, Lee JH, Perrier ND, Pisters PW, Lee JE, Evans DB (2005) Carcinoid tumors of the duodenum. Surgery 138(6):971–977 discussion 977-978
Tsai SD, Kawamoto S, Wolfgang CL, Hruban RH, Fishman EK (2015) Duodenal neuroendocrine tumors: retrospective evaluation of CT imaging features and pattern of metastatic disease on dual-phase MDCT with pathologic correlation. Abdom Imaging 40(5):1121–1130
Baumann T, Rottenburger C, Nicolas G, Wild D (2016) Gastroenteropancreatic neuroendocrine tumours (GEP-NET)—imaging and staging. Best Pract Res Clin Endocrinol Metab 30(1):45–57
Cameron JL, Riall TS, Coleman J, Belcher KA (2006) One thousand consecutive pancreaticoduodenectomies. Ann Surg 244(1):10–15
Huang JJ, Yeo CJ, Sohn TA, Lillemoe KD, Sauter PK, Coleman J, Hruban RH, Cameron JL (2000) Quality of life and outcomes after pancreaticoduodenectomy. Ann Surg 231(6):890–898
Odabasi M, Yildiz KM, Cengiz E, Hasan AH, Gunay E, Ozkan E, Aktekin A, Kaya B, Muftuoglu TM (2013) Treatment of ampullary neuroendocrine tumor by endoscopic snare papillectomy. Am J Case Rep 14:439–443
Kim GH, Kim JI, Jeon SW, Moon JS, Chung IK, Jee SR, Kim HU, Seo GS, Baik GH, Lee YC, Korean College of H, Upper Gastrointestinal R (2014) Endoscopic resection for duodenal carcinoid tumors: a multicenter, retrospective study. J Gastroenterol Hepatol 29(2):318–324
Zhang RC, Xu XW, Wu D, Zhou YC, Ajoodhea H, Chen K, Mou YP (2013) Laparoscopic transduodenal local resection of periampullary neuroendocrine tumor: a case report. World J Gastroenterol 19(39):6693–6698
Tsujimoto H, Ichikura T, Nagao S, Sato T, Ono S, Aiko S, Hiraki S, Yaguchi Y, Sakamoto N, Tanimizu T, Yamamoto J, Hase K (2010) Minimally invasive surgery for resection of duodenal carcinoid tumors: endoscopic full-thickness resection under laparoscopic observation. Surg Endosc 24(2):471–475
Kayahara M, Nagakawa T, Ohta T, Kitagawa H, Miyazaki I (1997) Surgical strategy for carcinoma of the papilla of vater on the basis of lymphatic spread and mode of recurrence. Surgery 121(6):611–617
Moriya T, Kimura W, Hirai I, Mizutani M, Ma J, Kamiga M, Fuse A (2006) Nodal involvement as an indicator of postoperative liver metastasis in carcinoma of the papilla of Vater. J Hepato-Biliary-Pancreat Surg 13(6):549–555
Gratian L, Pura J, Dinan M, Roman S, Reed S, Sosa JA (2014) Impact of extent of surgery on survival in patients with small nonfunctional pancreatic neuroendocrine tumors in the United States. Ann Surg Oncol 21(11):3515–3521
Albores-Saavedra J, Hart A, Chable-Montero F, Henson DE (2010) Carcinoids and high-grade neuroendocrine carcinomas of the ampulla of vater: a comparative analysis of 139 cases from the surveillance, epidemiology, and end results program-a population based study. Arch Pathol Lab Med 134(11):1692–1696
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269 W264
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
None of the authors have conflicts of interest associated with the publication of this article. Because our institutional review board approves the conduction of retrospective cohort studies on an occasional basis, the present study was exempt from obtaining additional statements of informed consent from each patient. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Iwasaki, T., Nara, S., Kishi, Y. et al. Surgical treatment of neuroendocrine tumors in the second portion of the duodenum: a single center experience and systematic review of the literature. Langenbecks Arch Surg 402, 925–933 (2017). https://doi.org/10.1007/s00423-016-1537-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1537-6