Abstract
Background
Acute pancreatitis remains an unpredictable, potentially lethal disease with significant morbidity and mortality rates. New insights in the pathophysiology of acute pancreatitis have changed management concepts. In the first phase, characterized by a systemic inflammatory response syndrome, organ failure, not related to infection but rather to severe inflammation, dominates the focus of treatment. In the second phase, secondary infectious complications largely determine the clinical outcome. As infection is associated with increased mortality in acute pancreatitis, numerous prophylactic strategies have been explored in the past two decades.
Purpose
This review describes the strategies that have been developed to lower the infection rate, in an attempt to lower mortality. Antibiotic prophylaxis has been the subject of many RCT’s without showing convincing evidence of their efficacy. Probiotics, although theoretically capable of lowering the rate of infection, also had no effect on infectious complications, and consequently, no effective strategy to lower the rate of infectious complications is currently available. In the second part of this review, new approaches for necrosectomy that have been designed by different centers around the world are discussed. All the interventional techniques have in common their aim to lower the invasive character, hypothesizing that lowering the surgical trauma will improve survival and lower complication rates. Recent advances include postponing intervention as a strategy to facilitate necrosectomy and improve prognosis and the “step-up approach” in case of infected necrosis. The step-up approach includes percutaneous catheter drainage as the first step, to be followed by necrosectomy, either through a minimally invasive approach or by open necrosectomy, as the next step.
Conclusions
All attempts to develop treatment strategies to lower the infection rate in acute pancreatitis have failed. Accumulating evidence is emerging to show that the combination of centralization, the use of catheter drainage as the first step of invasive treatment, and the development of minimally invasive techniques, improve the outlook for patients with infected necrosis. It is uncertain at this point in time as to which of the three effects is dominant in the improvement of prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute pancreatitis is a relatively common, potentially life-threatening disease. It is the third most common gastrointestinal disorder requiring acute hospitalization in the United States, with annual costs exceeding $2 billion (1, 2). Approximately 20 % of patients develop severe acute pancreatitis (3). Severe pancreatitis is associated with a mortality of 15–30 %, whereas mortality of mild pancreatitis is only 0–1 % (4). Organ failure is the most important determinant for mortality in acute pancreatitis (4). However, in around 30 % of patients with necrotizing pancreatitis, secondary infection of necrosis occurs, mostly 3–4 weeks after the onset of disease (4). If left untreated, mortality of infected necrosis approaches 100 % (3).
In most Western countries, gallstones are the cause of pancreatitis in approximately 50 % of patients and alcohol in 20 %. In about 20 % of cases, the cause remains unknown (idiopathic). The remaining 10 % constitutes a rather large group of possible causes of acute pancreatitis, which include hypercalcemia, hypertriglyceridemia, medications, hereditary causes, sphincter of Oddi dysfunction, pancreas divisum, pancreatic neoplasms, and others.
In the last years, data has become available to lend evidence-based support for changes in the surgical approach to pancreatitis, specifically for those patients who develop infected necrosis at some point in the course of the disease.
Diagnosis and clinical course
Clinical presentation
The diagnosis of acute pancreatitis is based on two or more of the following criteria: (a) severe abdominal pain, (b) serum amylase or lipase three or more times the upper limit of normal, (c) computed tomography (CECT) findings of acute pancreatitis. Usually, the first two criteria are present and CECT is not required. It takes at least 72–96 h of disease for a CECT scan to demonstrate relevant morphological changes like intra- and/or peripancreatic necrosis or fluid collections.
Clinical course
Acute pancreatitis runs a biphasic clinical course. The first phase (i.e., 1–2 weeks after onset of symptoms) is characterized by a systemic inflammatory response syndrome (SIRS). Organ failure in the SIRS phase is usually not related to infection but rather a direct result of severe systemic inflammation. Infectious complications like bacteremia and (ventilator associated) pneumonia do, however, occur in the first week of admission (4). Early organ failure may affect all organ systems and is diagnosed at a median of 2 days after admission, but may already be present from the start. Half of all fatal cases in acute pancreatitis are related to organ failure and the other half is related to infected necrosis. A recent systematic review of cohort studies demonstrated that the mortality of organ failure in acute pancreatitis is 32 % (5). Mortality in patients with both organ failure and infected necrosis is 43 % (5).
The second phase (i.e., after 1–2 weeks) is characterized by a counteractive anti-inflammatory response syndrome (CARS). Organ failure in the CARS phase is related to infections, such as infected necrosis.
With reference to the biphasic course, three scenarios can develop in severe acute pancreatitis: (a) Improvement with supportive measures, after early onset organ failure followed by deterioration in and around the third–fourth week of admission, often because of infection of necrosis. Further interventional treatment is usually indicated. (b) Clinical deterioration without distinct early organ failure, in and around the third–fourth week of admission. With this scenario, the chances of infected necrosis as the cause of clinical deterioration are also high. (c) Early onset organ failure that does not improve, even after 2–3 weeks of supportive treatment. Here, fine needle aspiration (FNA) of the peripancreatic collection (if no gas bubbles are present on CECT) may be performed to confirm or rule out infection and thus determine the need for intervention.
Laboratory investigation
Etiology of acute pancreatitis should be determined immediately on admission as this may be the only episode when there are significant clinical consequences like endoscopic retrograde cholangiopancreaticography (ERCP) with endoscopic sphincterotomy (ES) in case of gallstones as the cause of disease. Laboratory investigation should include liver function tests, calcium, and triglycerides. The latter two are often forgotten but hypercalcemia (usually related to hyperparathyroidism) and hypertriglyceridemia (arbitrarily >15 mmol/l) both need treatment to prevent recurrence of pancreatitis after recovery from the first attack.
Imaging
The most relevant imaging modality on admission is a transabdominal ultrasound in order to detect gallstones or sludge in the gallbladder or in the common bile duct.
The diagnosis biliary pancreatitis is made on the basis of imaging (in the presence of documented gallstones or sludge) but can also be made in the absence of stones or sludge. In the absence of gallstones or sludge, a widened common bile duct (>8 mm if age ≤5 years or >10 mm if age >75 years) or alanine amino transferase (ALAT) >100 U/l with ALAT > ASAT may suffice. If the etiology remains unknown and other causes than gallstones are excluded, endoscopic ultrasound can reveal gallstones or sludge in the gallbladder or common bile duct to support an indication for ERCP and ES. CECT scan, performed in patients who do not improve after the first week of symptoms, is used to diagnose necrosis and peripancreatic collections. Inaccuracy in defining peripancreatic collections has crept in and too often, a homogenous peripancreatic fluid collection is diagnosed as a “pseudocyst” whereas it actually contains pancreatic or peripancreatic necrosis. This misconception is caused by the incapacity of CECT to demonstrate solid components (necrosis) in a predominantly fluid collection (Fig. 1a). Magnetic resonance imaging (MRI; Fig. 1b) or ultrasonography are modalities capable of showing necrosis with high accuracy, which, if present, is a prerequisite to discard a collection as a pseudocyst (6). A true pseudocyst (i.e., fully encapsulated collection containing fluid only) during an episode of acute pancreatitis is very rare.
CT and MRI images, performed within 2 days of each other, of a patient with necrotizing pancreatitis. a CT scan with a typical peripancreatic collection. The collection appears homogeneous without apparent necrosis. Often, such a collection is misdiagnosed as a pseudocyst. b MRI, T2-weighted image shows clearly a large amount of necrosis in the collection. This is therefore not a pseudocyst, but rather an example of walled-off necrosis
Treatment
Conservative management
SIRS phase (week 1–2)
In the first phase of severe pancreatitis, characterized by a fulminant systemic inflammatory response, adequate fluid resuscitation is the mainstay of treatment. A diuresis-guided fluid regime (goal 1 ml/kg/h urine production) is sufficient in the initial phase, as long as organ failure is not yet present. Close monitoring is required and some patients may require over 20 l of intravenous fluid supplementation in the initial 24 h of severe pancreatitis. Unrestricted fluid resuscitation may, however, be harmful. A recent Chinese randomized trial demonstrated that very rapid fluid supplementation aiming at hematocrit levels <35 % in 48 h, leads to increased mortality (7). Another more recent study showed that early fluid resuscitation reduces morbidity (8).
Other treatments in the first phase focuses on prevention of infection (see below) or intervention for rare but severe complications like the abdominal compartment syndrome (see below). At this stage, there is no room for radiologic, endoscopic, or surgical intervention aiming at removing necrosis: i.e., the necrosis is mostly sterile in this phase, and patients with sterile necrosis can be treated conservatively.
CARS phase and thereafter
Systemic signs of infection with or without organ failure in the weeks to follow, after initial stabilization or improvement, strongly suggest infection of pancreatic and/or peripancreatic necrosis. To anticipate clinical deterioration, several authors advocate FNA of pancreatic collections depicted at CECT to establish or exclude infection, at a weekly basis. However, risks are a false-negative fine needle aspirate and introduction of infection by aspiration as such. Additionally, in case of clinical deterioration, a negative FNA does not withhold the clinician from intervention. Intervention performed in the CARS phase merely based on clinical signs and symptoms yields infected necrosis in 92 % of patients (9). Gas bubbles in peripancreatic collections are generally considered pathognomonic for infected necrosis. A recent Dutch study confirmed that FNA does not add to the diagnosis of infection of necrosis (submitted for publication).
Prevention of infection
As infection is associated with increased mortality in acute pancreatitis, numerous strategies to prevent infection have been explored in the past two decades. Enteral bacteria, crossing the mucosal barrier in the first 24 h of disease, are considered responsible for the majority of these infections. In a recent study, the first infection (bacteremia or ventilator associated pneumonia) were diagnosed at a median of 8 days after admission, whereas infection of necrosis was diagnosed median 26 days after admission (4). In a multivariable analysis in this series, persistent organ failure and bacteremia were the strongest predictors of mortality.
In mild pancreatitis, enteral nutrition can be started on the day of admission or the day thereafter as shown in a recent randomized trial (10). In predicted severe pancreatitis, it is now generally advised to start enteral nutrition by nasojejunal feeding tube if the patient is not expected to resume a normal diet within approximately 3 days. A recent meta-analysis showed that enteral nutrition reduces both infection and mortality when compared to total parenteral nutrition (11, 12). The optimal route for the administration of enteral feeding—through a nasojejunal or a nasogastric feeding tube—has yet to be established. Results of ongoing large studies are awaited before using nasogastric feeding routinely in patients with severe acute pancreatitis.
Systemic intravenous antibiotics, selective bowel decontamination, enteral probiotics, and enteral nutrition all have been tried to lower the rate of infection. In the following paragraphs, all these strategies are described.
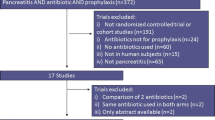
Antibiotic prophylaxis in an attempt to lower the rate of infectious complications in (predicted) severe acute pancreatitis has been the subject of many randomized controlled trials (RCTs). Although initial, non-blinded, non-placebo controlled, randomized trials showed somewhat positive effects, a recent updated meta-analysis clearly demonstrated no beneficial effect in the routine use of systemic antibiotic prophylaxis (13, 14).
Probiotics, although theoretically capable of lowering the rate of infection, had no effect on infectious complications in a recent randomized controlled trial. Probiotics were, however, associated with a twofold higher mortality rate (15). At this stage, it therefore seems that the probiotic mixture used in that study, should no longer be given to patients with “predicted severe acute pancreatitis.”
Routine selective bowel decontamination (SBD) or selective oropharyngeal decontamination is nowadays used in many intensive care units for a variety of indications. The only RCT performed in necrotizing pancreatitis demonstrated a reduction in (corrected) mortality in the SBD group, caused mostly by a reduction of gram-negative infections of pancreatic necrosis. Yet, up till now, no study has repeated the effect of SBD on the clinical course of acute pancreatitis and SBD as a prophylactic strategy in acute pancreatitis has not gained wide acceptance, but the concept deserves further exploration (16).
Interventional treatment
Sterile pancreatic necrosis and sterile peripancreatic collections can usually be treated conservatively. The only exception is probably severe mechanical complications (i.e., gastric outlet obstruction, duodenal obstruction, or persistent obstructive jaundice due to common bile duct compression) at least 1 month into the disease.
Intervention in the SIRS phase (weeks 1–2)
In gallstone pancreatitis, early ERCP with ES may theoretically prevent further clinical deterioration and reduce the risk of complications. However, a recent meta-analysis of randomized trials comparing ERCP with conservative treatment concluded that there are no benefits in performing routine ERCP in patients with predicted severe biliary pancreatitis without cholangitis (17). However, a recent prospective multicenter study demonstrated that ERCP with endoscopic sphincterotomy reduces the complication rate in the subgroup of patients with predicted severe biliary pancreatitis and cholestasis (18).
Treatment of acute life-threatening complications, like bleeding (unsuccessfully managed by angiographic coiling), perforation of a hollow viscus organ, and abdominal compartment syndrome, is the only justification for surgery in this early SIRS phase. In 1997, a RCT was published which compared early surgical intervention within 72 h (“early”) intervention after 12 days (“late”) (19). The authors terminated this study prematurely because of a much higher, not yet statistically significant, mortality for surgery within 72 h (58 vs 27 %). From then onwards, early necrosectomy was abandoned. The lessons learned from the past decades are that in the early phase of acute pancreatitis, the clinical picture is dominated by SIRS while infection of necrosis plays essentially no role. In the absence of suspicion of abdominal compartment syndrome, bowel ischemia, or other acute complications, there is no benefit at all to be expected from surgical exploration. If exploratory laparotomy is performed for acute complications, it is best advised not to explore the lesser sac and not to perform a necrosectomy because there is risk of introducing infection and bleeding complications.
According to the 2007 International Consensus meeting, abdominal compartment syndrome is defined by an intra-abdominal pressure higher than 20 mm Hg with signs of new organ failure (20). Although the optimal treatment strategy of abdominal compartment syndrome has yet to be defined, percutaneous drainage can be used as an initial step if intra-abdominal drainable fluid is present. If this does not lead to immediate clinical improvement or if there is no drainable fluid left, a decompression laparotomy is the next step. Most authors advise not to explore the pancreas during this operation because it is too early to remove necrosis safely and there is a risk of infection of the necrosis, probably still sterile at that stage.
Decompression, by drainage or surgery of peripancreatic fluid collections, in patients with (multi-)organ failure, is not indicated, as long as the pancreatic collections are not infected and do not cause obstruction of the digestive tract or common bile duct. Percutaneous drainage may seem alluring, but sterile collections may become iatrogenically contaminated by the percutaneous drains. A recent randomized study, actually advocating the strategy of draining sterile collections, reported on a significant increase in infected necrosis due to the practice of routine percutaneous drainage (21, 22).
Intervention in the second phase or CARS phase
The CARS phase or second phase is the phase where the patient is threatened by yet another episode of systemic infection or sepsis, caused most often by secondary infection of pancreatic and/or peripancreatic necrosis. Documented infection (by FNA or “gas” on CT scan) or suspected infection of pancreatic or peripancreatic necrosis in combination with systemic signs of infection and an encapsulated collection represents the accepted indication for intervention.
Once the stage for intervention has been reached, there is a choice between (minimally invasive) surgical, endoscopic, and radiologic percutaneous techniques. Open necrosectomy, with or without closed retroperitoneal lavage and with or without open packing, has been the standard for surgical treatment of infected necrosis for the last decades.
A recent Dutch multicenter-randomized patients with acute necrotizing pancreatitis pancreatitis: a step-up approach or open necrosectomy for infected necrosis (PANTER) trial in patients with documented or suspected infection of necrosis compared primary open necrosectomy with a minimally invasive “step-up approach (8).” The step-up approach consisted of percutaneous or transgastric drainage, followed if necessary, by drain-guided minimally invasive necrosectomy. A significant difference in major complications and costs was observed, all in favor of the step-up approach. The study was not powered to detect a difference in mortality as the primary endpoint and as a consequence, no significant difference was found.
In addition to all the advantages of the step-up approach described above, 35 % of patients who were treated by the step-up approach did not need any further intervention than percutaneous drainage only. Therefore, the step-up approach should be considered the new treatment paradigm for infected pancreatic necrosis. The type of additional intervention after drainage was not the subject of that study and needs to be left to the discretion of the treating surgeon
In the decades before this Dutch RCT, percutaneous drainage has been the subject of many, mostly uncontrolled, observational studies. A recent systematic review suggested that percutaneous drainage can be the only treatment needed in up to 55 % of patients with necrotizing pancreatitis. In this review, patients had a rate of preoperative organ failure of 77 %, and ultimately, 17 % of patients died. The technical success rate was 99 % (2,243). A multicenter series from USA and Canada found that 25 % of 40 patients with infected necrotizing pancreatitis can be treated with percutaneous drainage alone (23).
The overall message of these studies is that in patients who do not improve after technically adequate drainage, necrosectomy should be performed as the next step. The percutaneous drain, together with the CECT scan, can be used as a roadmap for (minimally invasive) necrosectomy.
Percutaneous (or transgastric) drainage should be considered the first step of intervention and the indication for drainage should be the same as has been used in the (recent) past for surgical necrosectomy. However, the results of the Dutch RCT should not be interpreted as a license to drain any collection that may develop into infected necrosis at a later stage.
Minimally invasive necrosectomy
Different techniques have been described from Glasgow, Seattle, and Liverpool. The technique developed by Carter and Imrie from Glasgow, modified by the group from Liverpool is a strictly percutaneous minimally invasive retroperitoneal necrosectomy using an operating nephroscope (24).
Both in the United States and Netherlands, the most often used minimally invasive surgical intervention is the “video-assisted retroperitoneal debridement (VARD)” technique, developed in Seattle (25–27). For review of the complete procedure: see http://www.youtube.com/watch?v=XicI4a7Q768 or search YouTube “VARD pancreatitis.” The relevant steps are illustrated in Fig. 2a–e. The designers of the different techniques stress that the goal of surgery is to remove as many loosely adherent pieces of necrosis as possible and not to remove all necrosis, in order to reduce the risk of bleeding and to leave the remnants of necrosis to be resorbed. Although repeated necrosectomy is often required with the percutaneous techniques, the VARD technique is mostly a one-stage procedure. Postoperative continuous drainage is part of the VARD technique and not so much of the other minimally invasive procedures.
a Contrast-enhanced CT scan with drain inserted. b The VARD procedure is about to be started, guided by the percutaneous drain as shown in Fig. 1a. c Subcutaneous fat is removed and transected, on the way to the necrotic cavity (walled-off necrosis). d The cavity has been opened, the laparoscope has been introduced, continuous rinsing is performed to identify necrotic debris and necrotic lumps. e The laparoscope has been temporarily removed in order to facilitate large necrotic lump. f The necrosis tissue has been largely removed, the different layers have been sutured, and drains for continuous lavage have been inserted
Endoscopic transluminal necrosectomy
Endoscopic transluminal/transgastric necrosectomy (ETN) is another rapidly expanding appealing strategy for necrosectomy with promising results in non-controlled studies. Of all the techniques available, this technique is theoretically the least invasive and pancreatic fistulas will not develop, since pancreatic juice will drain to the stomach. The technique shares the disadvantage of the need for repeated, multiple procedures to remove sufficient amounts of necrosis with the Glasgow and the Liverpool percutaneous techniques (28–30).
A recent randomized controlled trial comparing the effect of ETN and surgery showed that both the effects on immunological response after intervention and postprocedural complications were significantly in favor of ETN (31). The numbers were small and all sorts of procedures were used in the surgical arm. The results need confirmation in a larger trial with uniform surgical procedures in the surgical necrosectomy arm. This trial is currently well underway in The Netherlands.
Open necrosectomy
Until the results of the PANTER trial were published, primary open necrosectomy was considered the reference standard of treatment in patients with infected necrotizing pancreatitis. One of the most frequently used techniques of open necrosectomy for infected necrosis is laparotomy with placement of retroperitoneal lavage system after complete necrosectomy has been performed. In this technique, initially described by Rau et al., drains are placed in the lesser sac after necrosectomy. These drains will be continuously lavaged with increasing amounts (2–4–6 l) of saline per day. The exact role (strictly mechanical, preventing clotting or by dilution of the pancreatic juice) of the lavage is unknown. The mortality of this technique is approximately 25 % (32).
Another open approach is open necrosectomy and closed packing. The group from Boston reported 11 % mortality in 167 patients (33). Necrosis is approached through the transverse mesocolon and debrided bluntly, with the goal of removing all necrotic tissue and particulate debris. The resulting cavity is then packed with gauze-stuffed Penrose drains that are removed one by one after a week.
Some centers use the “open abdomen strategy” with regular, planned relaparotomies as routine intervention strategy. The mortality of this procedure, when used routinely, is 70 % and it is advised to use this only as a “rescue strategy.” The use of these techniques is rapidly expanding but the exact place and indication for any of these three options has not been sorted out yet.
Timing of intervention
Timing and choice of the type of intervention under close guidance by a multidisciplinary team are crucial. A systematic review of cohort studies concluded that postponing interventions until the intra- and/or extrapancreatic collections are encapsulated, a process that usually takes 4 weeks, is beneficial. Such encapsulated collections are now called “walled-off necrosis.”
In some scenarios, encapsulation of pancreatic collections may not have been completed when clinical deterioration occurs. In order to postpone surgical intervention and to prevent bacteremia or sepsis, the administration of broad spectrum antibiotics is crucial in order to buy time and to allow the collection to further encapsulate. In the previously mentioned review, necrosectomy was performed at a median of 27 days after onset of disease, with a mortality rate of 25 %. Based on the current literature, postponing of intervention, preferably until 4 weeks after onset of disease, is widely accepted as the strategy of choice. A recently published study on a large prospective cohort of patients with necrotizing pancreatitis, the association between timing of intervention and outcome with logistical regression corrected for confounders, clearly showed the beneficial effect of postponing surgical intervention to allow for the necrosis to encapsulate; facilitating successful necrosectomy (34, 35). The length of the interval between the onset of symptoms and timing of intervention is mainly determined by the completeness of encapsulation and the clinical condition of the patient.
This policy is obviously only applicable to the subset of patients who survive the initial phase of SIRS and develop infection of necrosis in the phase of CARS.
Result of necrosectomy
All recent series suggest a decrease in mortality due to the use of minimal invasive techniques from over 30 to around 15–20 %. Indeed, even in the largest series from Glasgow, mortality still remains in the order of 15–20 %.
Percutaneous drainage is the only least-invasive technique for treatment of infected necrosis with a success rate (no open necrosectomy needed) of 25–55 % and mortality ranging from 15–20 %. However, results are difficult to weigh and to balance out against other minimally invasive techniques because of differences in patient selection and clinical details of treatment and follow-up. ETN is probably the next in line as far as invasiveness of the technique is concerned. Success rates are higher, between 80 and 93 % and mortality is lower, ranging from 0 to 6 %. Most of the published series suffer from selection bias and the rate of infection in some series is unacceptably low, raising the question of whether these patients needed necrosectomy at all. Percutaneous techniques, including VARD, need open necrosectomy in quite a high proportion of patients and mortality is around 20 %.
Prevention of recurrent pancreatitis
If gallstones are the cause of pancreatitis, cholecystectomy, possibly with bile duct clearance, is required to prevent recurrent episodes of biliary pancreatitis. The optimal timing of cholecystectomy is subject to debate. (36) Most authors propose to perform cholecystectomy during the index admission in case of mild biliary pancreatitis although some claim that this may be technically more difficult. The latter claim, however, is not substantiated by data reported in the literature. Because level 1 evidence on this subject is lacking, the Dutch Pancreatitis Study Group is currently performing the PONCHO trial to determine the optimal timing of cholecystectomy in patients with mild biliary pancreatitis (http://www.controlled-trials.com/isrctn/pf/72764151) Conversely, Nealon et al. demonstrated that early cholecystectomy in patients with severe pancreatitis (i.e., necrotizing pancreatitis) may be harmful as pancreatic collections may become infected due to cholecystectomy with dismal outcome (36).
Conclusion
Acute pancreatitis remains an unpredictable potentially lethal disease with significant morbidity and mortality rates. Recent advances include:
-
Postponing intervention as a way to facilitate necrosectomy and improve prognosis, (albeit the exact timing of intervention demands further study).
-
The use of catheter drainage (rather than necrosectomy) as the first therapeutic step in case of suspected or documented infected necrotizing pancreatitis.
-
The best technique for necrosectomy has yet to be established. Open necrosectomy therefore still remains a feasible option for treatment of patients with infected necrosis in whom primary percutaneous drainage has failed.
References
Fagenholz PJ, Fernandez-del Castillo C, Harris NS, Pelletier AJ, Camargo CA (2007) Direct medical costs of acute pancreatitis hospitalizations in the United States. Pancreas 35(4):302–307
Shaheen NJ, Hansen RA, Morgan DR, Gangarosa LM, Ringel Y, Thiny MT et al (2006) The burden of gastrointestinal and liver diseases. Am J Gastroenterol 101(9):2128–2138
Banks PA, Freeman ML (2006) Practice guidelines in acute pancreatitis. Am J Gastroenterol 101(10):2379–2400
Besselink MG, Van Santvoort HC, Boermeester MA, Nieuwenhuijs VB, van Goor H, Dejong CH et al (2009) Timing and impact of infections in acute pancreatitis. Br J Surg 96(3):267–273
Petrov MS, Shanbhag S, Chakreborty M et al (2010) Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Gastroenterology 139:813–820
Working Party of the British Society of Gastroenterology, Association of Surgeons of Great Britain and Ireland, Pancreatic Society of Great Britain and Ireland, Association of Upper GI Surgeons of Great Britain and Ireland (2005) UK guidelines for the management of acute pancreatitis. Gut 54 Suppl 3:iii1–iii9
Mao EQ, Tang YQ, Fei J, Qin S, Wu J, Li L et al (2009) Fluid therapy for severe acute pancreatitis in acute response stage. Chin Med J (Engl) 122(2):169–173
Warndorf MG, Kurtzman JT, Bartel MJ, Cox M, Mackenzie T, Robinson S, Burchard PR, Gordon SR, Gardner TB (2011) Early fluid resuscitation reduces morbidity among patients with acute pancreatitis. Clin Gastroenterol Hepatol 8:705–709
Van Santvoort HC, Besselink MG, Bakker OJ, Hofker HS, Boermeester MA, Dejong CH et al (2010) A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med 362(16):1491–1502
Eckerwall GE, Tingstedt BB, Bergenzaun PE, Andersson RG (2007) Immediate oral feeding in patients with mild acute pancreatitis is safe and may accelerate recovery–a randomized clinical study. Clin Nutr 26(6):758–763
Petrov MS, Zagainov VE (2007) Influence of enteral versus parenteral nutrition on blood glucose control in acute pancreatitis: a systematic review. Clin Nutr 26(5):514–523
Petrov MS, Loveday BP, Pylypchuk RD, McIlroy K, Phillips AR, Windsor JA (2009) Systematic review and meta-analysis of enteral nutrition formulations in acute pancreatitis. Br J Surg 96(11):1243–1252
De Vries AC, Besselink MGH, Van der Kraats CIB, Buskens E, van Erpecum KJ, Gooszen HG (2005) Antibiotic prophylaxis in acute necrotising pancreatitis: methodological quality of randomised controlled trials in relation to outcome. Gut 54(Supplement VII):A38–A39
Wittau M, Mayer B, Scheele J, Henne-Bruns D, Dellinger EP, Isenmann R (2011) Systematic review and meta-analysis of antibiotic prophylaxis in severe acute pancreatitis. Scand J Gastroenterol 46(3):261–270
Besselink MGH, van Santvoort HC, Buskens E, Boermeester MA, van Goor H, Timmerman H, Nieuwenhuijs VB, Bollen TL, van Ramshorst B, Witteman BJ, Rosman C, Ploeg RJ, Brink M, Schaapherder AF, van Dejong CH, Wahab PJ, van Laarhoven CJHM, van der Harst E, van Eijck CHJ, Cuesta MA, Akkermans LMA, Gooszen HG (2008) Probiotic prophylaxis in predicted severe acute pancreatitis: a randomised, double-blind, placebo-controlled trial. Lancet 371(9613):651–659
Luiten EJ, Hop WC, Lange JF, Bruining HA (1995) Controlled clinical trial of selective decontamination for the treatment of severe acute pancreatitis. Ann Surg 222(1):57–65
Petrov MS, Van Santvoort HC, Besselink MG, van der Heijden GJ, van Erpecum KJ, Gooszen HG (2008) Early endoscopic retrograde cholangiopancreatography versus conservative management in acute biliary pancreatitis without cholangitis: a meta-analysis of randomized trials. Ann Surg 247(2):250–257
Van Santvoort HC, Besselink MG, De Vries AC, Boermeester MA, Fischer K, Bollen TL et al (2009) Early endoscopic retrograde cholangiopancreatography in predicted severe acute biliary pancreatitis: a prospective multicenter study. Ann Surg 250(1):68–75
Mier J, Luque-de León E, Castillo A, Robledo F, Blanco R (1997) Early versus late necrosectomy in severe pancreatitis. Am J Surg 173(2):71–75
Cheatham ML, Malbrain ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J et al (2007) Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome II. Recommendations. Intensive Care Med 33(6):951–962
Zerem E, Imamovic G, Omerovic S, Imsirovic B (2009) Randomized controlled trial on sterile fluid collections management in acute pancreatitis: should they be removed? Surg Endosc 23:2770–2777
Besselink MG, Van Santvoort HC, Bakker OJ, Bollen TL, Gooszen HG (2010) Draining sterile fluid collections in acute pancreatitis? Primum non nocere! Surg Endosc 25(1):331–332
Van Baal MC, Van Santvoort HC, Bollen TL, Bakker OJ, Besselink MG, Gooszen HG et al (2011) Systematic review of percutaneous catheter drainage as primary treatment for necrotizing pancreatitis. Br J Surg 98(1):18–27
Raraty MG, Halloran CM, Dodd S, Ghaneh P, Connor S, Evans J et al (2010) Minimal access retroperitoneal pancreatic necrosectomy: improvement in morbidity and mortality with a less invasive approach. Ann Surg 251(5):787–793
Horvath K, Freeny P, Escallon J, Heagerty P, Comstock B, Glickerman DJ et al (2010) Safety and efficacy of video-assisted retroperitoneal debridement for infected pancreatic collections: a multicenter, prospective, single-arm phase 2 study. Arch Surg 145(9):817–825
Horvath KD, Kao LS, Wherry KL, Pellegrini CA, Sinanan MN (2010) A technique for laparoscopic-assisted percutaneous drainage of infected pancreatic necrosis and pancreatic abscess. Surg Endosc 15(10):1221–1225
Van Santvoort HC, Besselink MGH, Horvath KD, Sinanan M, Bollen TL, Ramshorst B et al (2007) Videoscopic assisted retroperitoneal debridement in infected necrotizing pancreatitis. HPB 9(2):156–159
Papachristou GI, Takahashi N, Chahal P, Sarr MG, Baron TH (2007) Peroral endoscopic drainage/debridement of walled-off pancreatic necrosis. Ann Surg 245(6):943–951
Seifert H, Biermer M, Schmitt W, Jurgensen C, Will U, Gerlach R et al (2009) Transluminal endoscopic necrosectomy after acute pancreatitis: a multicentre study with long-term follow-up (the GEPARD Study). Gut 58(9):1260–1266
Voermans RP, Bruno MJ, van Berge Henegouwen MI, Fockens P (2007) Review article: translumenal endoscopic debridement of organized pancreatic necrosis—the first step towards natural orifice translumenal endoscopic surgery. Aliment Pharmacol Ther 26(Suppl 2):233–239
Bakker OJ, van Santvoort HC, van Brunschot S, Geskus RB, Besselink MG, Bollen TL et al (2012) Endoscopic transgastric vs surgical necrosectomy for infected necrotizing pancreatitis: a randomized trial. JAMA 307(10):1053–1061
Rau B, Bothe A, Beger HG (2005) Surgical treatment of necrotizing pancreatitis by necrosectomy and closed lavage: changing patient characteristics and outcome in a 19-year, single-center series. Surgery 138(1):28–39
Rodriguez JR, Razo AO, Targarona J, Thayer SP, Rattner DW, Warshaw AL et al (2008) Debridement and closed packing for sterile or infected necrotizing pancreatitis: insights into indications and outcomes in 167 patients. Ann Surg 247(2):294–299
Besselink MG, Verwer TJ, Schoenmaeckers EJ, Buskens E, Ridwan BU, Visser MR et al (2007) Timing of surgical intervention in pancreatitis. Arch Surg 142(12):1194–1201
Dutch Pancreatitis Study Group, van Santvoort HC, Bakker OJ, Bollen TL, Besselink MG, Ahmed Ali U, Schrijver AM et al (2011) A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology 141(4):1254–1263
Nealon WH, Bawduniak J, Walser EM (2004) Appropriate timing of cholecystectomy in patients who present with moderate to severe gallstone-associated acute pancreatitis with peripancreatic fluid collections. Ann Surg 239(6):741–749
Acknowledgments
This manuscript and parts of the display items were based on the chapter “acute pancreatitis” as prepared by the authors for the 7th Edition of “Shackelford’s Surgery of the Alimentary Tract,” copyright Elsevier (2012).
Conflicts of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gooszen, H.G., Besselink, M.G.H., van Santvoort, H.C. et al. Surgical treatment of acute pancreatitis. Langenbecks Arch Surg 398, 799–806 (2013). https://doi.org/10.1007/s00423-013-1100-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-013-1100-7