Abstract
Introduction
The aim of our study was to compare single incision laparoscopic cholecystectomy (SILC) and laparoscopic cholecystectomy (LC) with respect to complications, operating time, postoperative pain, use of analgesics, length of stay, return to work, rate of incisional hernia, and cosmetic outcome.
Methods
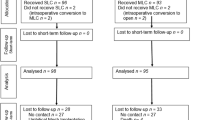
Sixty-seven patients underwent SILC. Of a cohort of 163 LC operated in the same time period, 67 patients were chosen for a matched pair analysis. Pairs were matched for age, gender, ASA, BMI, acuity, and previous abdominal surgery. In the SILC group, patient characteristics (gender, age, BMI, comorbidities, ASA, previous abdominal surgery, symptomatic cholecystolithiasis, cholecystitis) and perioperative data (surgeon, operation time, conversion rate and cause, intraoperative complications, postoperative complications, reoperation rate, VAS at 24 h, VAS at 48 h, use of analgesics according to WHO class, and length of stay) were collected prospectively.
Results
Follow-up in the SILC and LC group was completed with a minimum of 17 and a maximum of 26 months; data acquired were recovery time the patients needed until they were able to get back into the working process, long-term incidence of postoperative hernias, and satisfaction with cosmetic outcome. Operating time was longer for SILC (median 75 min, range 39–168 vs. 63, range 23–164, p = 0.039). There were no significant differences for SILC and LC with regard to postoperative pain measured by VAS at 24 h (median 3, range 0–8 vs. 2, range 0–8, p = 0.224), at 48 h (median 2, range 0–6 vs. 2, range 0–8, p = 0.571), use of analgesics, and length of stay (median 2 days, range 1–9 vs. 2, range 1–11, p = 0.098). There was no major complication in either group. The completion rate of SILC was 85.1% (57 of 67). Although there was a trend towards an earlier return to the working process in patients of the SILC group, this was not significant. The rate of incisional hernias was 1.9% (1/53) in the SILC and 2.1% (1/48) in the LC group indicating no significant difference. Self-assessment of satisfaction with the cosmetic outcome was not judged different by patients in both groups.
Conclusion
SILC is associated with longer operating time, but equals LC with respect to safety, postoperative pain, use of analgesics, length of stay, return to work, rate of incisional hernia, and cosmetic outcome.
Similar content being viewed by others
References
Mühe E (1986) Die erste Cholecystektomie durch das Laparoskop (The first laparoscopic cholecystectomy). Langenbecks Arch Surg 369:804
Reddick EJ, Olsen DO (1989) Laparoscopic laser cholecystectomy. A comparison with mini-lap cholecystectomy. Surg Endosc 3:131–133
Cuschieri A, Dubois F, Mouiel J, Mouret P, Becker H, Buess G, Trede M, Troidl H (1991) The European experience with laparoscopic cholecystectomy. Am J Surg 161:385–387
Dolan JP, Diggs BS, Sheppard BC, Hunter JG (2009) The national mortality burden and significant factors associated with open and laparoscopic cholecystectomy: 1997–2006. J Gastrointest Surg 13:2292–2301
Meining A, Feussner H, Swain P, Yang GZ, Lehmann K, Zorron R, Meisner S, Ponsky J, Martiny H, Reddy N, Armengol-Miro JR, Fockens P, Fingerhut A, Costamagna G (2011) Natural-Orifice Transluminal Endoscopic Surgery (NOTES) in Europe: summary of the working group reports of the Euro-NOTES meeting 2010. Endoscopy 43(2):140–143
Antoniou SA, Pointner R, Granderath FA (2011) Single-incision laparoscopic cholecystectomy: a systematic review. Surg Endosc 25(2):367–377
Hodgett ST, Hernandez JM, Morton CA, Ross SB, Albrink M, Rosemurgy AS (2009) Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg 13:188–192
Philipp SR, Miedema BW, Thaler K (2009) Single-incision laparoscopic cholecystectomy using conventional instruments: early experience in comparison with the gold standard. J Am Coll Surg 209:632–637
Hernandez JM, Morton CA, Ross S, Albrink M, Rosemurgy AS (2009) Laparoendoscopic single site cholecystectomy: the first 100 patients. Am Surg 75(8):681–685
Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, Manataki A (2010) Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 24(8):1842–1848
Fronza JS, Linn JG, Nagle AP, Soper NJ (2010) A single institution’s experience with single incision cholecystectomy compared to standard laparoscopic cholecystectomy. Surgery 148(4):731–734
Prasad A, Mukherjee KA, Kaul S, Kaur M (2010) Postoperative pain after cholecystectomy: conventional laparoscopy versus single-incision laparoscopic surgery. J Minim Access Surg 7(1):24–27
Chang SK, Tay CW, Bicol RA, Lee YY, Madhavan K (2011) A case–control study of single-incision versus standard laparoscopic cholecystectomy. World J Surg 35(2):289–293
Khambaty F, Brody F, Vaziri K, Edwards C (2011) Laparoscopic versus single-incision cholecystectomy. World J Surg 35(5):967–972
Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I (1997) One-wound laparoscopic cholecystectomy. Br J Surg 84:695
Marks J, Tacchino R, Roberts K, Onders R, Denoto G, Paraskeva P, Rivas H, Soper N, Rosemurgy A, Shah S (2011) Prospective randomized controlled trial of traditional laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy: report of preliminary data. Am J Surg 201(3):369–373
Emami CN, Garrett D, Anselmo D, Nguyen NX (2011) Pediatric single incision laparoscopic cholecystectomy: lessons learned in the first 25 cases. Pediatr Surg Int [Epub ahead of print]
Bignell M, Hindmarsh A, Nageswaran H, Mothe B, Jenkinson A, Mahon D, Rhodes M (2011) Assessment of cosmetic outcome after laparoscopic cholecystectomy among women 4 years after laparoscopic cholecystectomy: is there a problem? Surg Endosc [Epub ahead of print]
Lee PC, Lo C, Lai PS, Chang JJ, Huang SJ, Lin MT, Lee PH (2010) Randomized clinical trial of single-incision laparoscopic cholecystectomy versus minilaparoscopic cholecystectomy. Br J Surg 97(7):1007–1012
Hernandez J, Ross S, Morton C, McFarlin K, Dahal S, Golkar F, Albrink M, Rosemurgy A (2010) The learning curve of laparoendoscopic single-site (LESS) cholecystectomy: definable, short, and safe. J Am Coll Surg 211(5):652–657
Solomon D, Bell RL, Duffy AJ, Roberts KE (2010) Single-port cholecystectomy: small scar, short learning curve. Surg Endosc 24(12):2954–2957
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gangl, O., Hofer, W., Tomaselli, F. et al. Single incision laparoscopic cholecystectomy (SILC) versus laparoscopic cholecystectomy (LC)—a matched pair analysis. Langenbecks Arch Surg 396, 819–824 (2011). https://doi.org/10.1007/s00423-011-0817-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-011-0817-4