Abstract
Purpose
The purpose of this study was to compare the effects of acupuncture and acupressure of acupoints on tendon blood circulation with those of both types of stimulation of tendon itself.
Methods
Before, during (except for acupressure), and after acupuncture and acupressure of the tendon and acupoint, blood circulation of the Achilles tendon was measured using red laser lights.
Results
The blood volume of the treated and non-treated tendons increased after acupuncture of the tendon (effect of time p = 0.030), whereas that tended to increase after acupuncture of the acupoint (effect of time p = 0.063). In addition, no significant difference in the increases in blood volume was found among the four conditions, i.e., after acupuncture stimulation of the tendon and acupoint for the treated and non-treated tendons (p = 0.492). The blood volume of the treated tendon significantly increased after acupressure of the tendon (effect of time p < 0.001), but not of the acupoint (effect of time p = 0.260), whereas that of the non-treated tendon did not change after acupressure of both the tendon and acupoint.
Conclusion
These results suggested that acupuncture of the tendon and acupoint acted centrally to enhance blood circulation of both the treated and non-treated tendons during the recovery period, whereas acupressure of the tendon locally increased blood circulation of the treated tendon only, but not the non-treated tendon and both the treated and non-treated tendons after acupressure of acupoint.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is known that tendon disorders are linked to disturbances in tendon vasculature, which result in insufficiency in blood circulation (Jarvinen et al. 1997). As a result of local tissue hypoxia and inadequate nutrition brought on by decreased blood circulation within the tendons, tendon degeneration is likely to occur (Ahmed et al. 1998; Carr and Norris 1989; Stein et al. 2000; Zantop et al. 2003). In the medical field, acupuncture and acupressure are known to be effective in treating tendon disorders (e.g., Alim et al. 2018; Kleinhenz et al. 1999). The healing mechanisms of tendon disorders with these therapies included improved blood circulation of the tendons (Chen et al. 2001; Greve et al. 2012; Praxitelous et al. 2018). In fact, our studies showed that blood volume and oxygen saturation of the human tendons increased after acupuncture and acupressure (Kubo et al. 2010, 2011, 2020a, b; Yasuda et al. 2022). In all of these studies, acupuncture and acupressure were directly applied to the tendons. In the medical field, however, these therapies are generally performed at a distance from the affected area, i.e., the remote acupoint (Haker and Lunderberg 1990; Fink et al. 2002).
Many previous studies have shown that muscle and skin blood flow increased with acupuncture and acupressure of acupoints (Hsiu et al. 2010; Li et al. 2007; Litscher et al. 2002; Sandberg et al. 2003). To our knowledge, no studies animal or human studies have examined the effects of acupuncture and acupressure of remote acupoints on tendon blood circulation. Although the acupoints have not been fully elucidated, histochemical studies reported that acupoints were sites of dense concentrations of Aδ and C afferent sensory nerve fibers (Li et al. 2004). To apply our findings in a medical setting, we need to investigate the effects of acupuncture and acupressure of the acupoints, i.e., at points distant from the tendons, on the blood circulation of the human tendons in vivo.
From the results of animal experiments (Kagitani et al. 2005, 2010), acupuncture of acupoints on the lower leg has been shown to cause activation of Aδ and C fibers in the dorsal root ganglion of the lumbar region. In human experiments, acupuncture and acupressure of acupoints have been shown to decrease heart rate and alter the autonomic nervous system (as assessed by heart rate variability) (Arai et al. 2011; Haker et al. 2000; Matsubara et al. 2011; Nishijo et al. 1997). Our previous studies demonstrated that blood circulation of the tendons in the treated and non-treated sides increased after acupuncture and acupressure of the Achilles tendon (Kubo et al. 2011, 2020a, b). These results suggested that acupuncture and acupressure of tendons elicited a systemic response. In light of the above, acupuncture and acupressure of acupoints is also expected to produce a systemic reaction (i.e., an increase in tendon blood circulation in the treated and non-treated sides) through the sensory nerves distribution to the acupoints.
The purpose of this study was to compare the effects of acupuncture and acupressure of acupoints on tendon blood circulation with those of both types of stimulation of tendons. We hypothesized that acupuncture and acupressure of acupoint would enhance blood circulation of the tendon on both the treated and non-treated sides due to a systemic response during the recovery period after stimulation, as is the case with stimulation of the tendon, because of the dense concentration of sensory nerves at the acupoint as described above.
Methods
Participants
The sample size was estimated according to our previous studies in which the increases in the blood volume of the Achilles tendon by acupuncture and acupressure were determined (0.63 ± 0.56 µmol·L−1 in Kubo et al. 2010, 0.65 ± 0.56 µmol·L−1 in Kubo et al. 2011, 0.87 ± 1.05 µmol·L−1 in Kubo et al. 2020a). Based on an α level of 0.05 and a power (1 – ß) of 0.8, it was shown that at least eleven participants per group were necessary for the present study. Twenty-six healthy volunteers (23 males and 3 females; age: 27.8 ± 9.7 years, height: 170.9 ± 6.7 cm, body mass: 69.2 ± 14.0 kg, mean ± SD) participated in this study. Twelve and fourteen volunteers participated in the acupuncture and acupressure experiments (Fig. 1). Exclusion criteria included a history of injuries and surgery on the Achilles tendon and cardiovascular diseases related to blood circulation. The participants were fully informed of the procedures to be utilized and the purpose of this study. Written informed consent was obtained from all participants. This study was approved by the office of the Department of Sports Sciences, The University of Tokyo, and complied with their requirements for human experimentation, and was performed by the Declaration of Helsinki. One part of the data in our previous study (n = 13, tendon blood circulation during and after acupuncture of the tendon in Kubo et al. 2020a) diverted to the data in the present study (n = 12; tendon blood circulation during and after acupuncture of the tendon), because 12 of the 13 participants in our previous study (Kubo et al. 2020a) took part in the measurement of the changes in tendon blood circulation with acupuncture of the acupoint due to scheduling limitations.
Experimental protocol (see Methods for a detailed description of the protocol)
Acupuncture and acupressure
The participants lay prone on a test bench to acclimate to the laboratory conditions for 15 min before the experiment. Initially, the participants lay in a prone position for a 20 min rest period (baseline). After that, a needle was inserted (acupuncture stimulation experiment) or acupressure was applied (acupressure stimulation experiment) to the right Achilles tendon or acupoint (BL57 Chengshan). BL57 was chosen as an acupoint and was located in the myotendinous junction of the triceps surae, which is continuous with the Achilles tendon (Zhang et al. 2004). After the needle was removed or the acupressure was stopped, the participants remained relaxed in the same position for 40 min. Each participant received two treatments (stimulation of tendon and acupoint) on two separate days, with at least one week between sessions and no longer than two weeks separating the two sessions. The entire experimental protocol is described in Fig. 1. The order of the two experimental conditions was randomized for each participant.
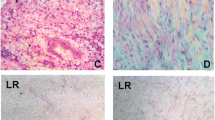
Acupuncture Acupuncture was performed by one of the authors (H.Y.), an experienced (more than 25 years) licensed acupuncturist (Fig. 2A). A stainless steel needle of 0.16 mm in diameter and 40 mm in length was inserted vertically into the skin at 40 mm proximal to the calcaneus (stimulation of the tendon experiment) or the acupoint (stimulation of the acupoint experiment). To locate the acupoint (BL57), ultrasonography (SSD-3500, Aloka, Tokyo, Japan) was used to identify the boundary between the medial and lateral gastrocnemius muscles and the myotendinous junction between the Achilles tendon and gastrocnemius muscle. After insertion of the needle to a targeted depth (4 mm for the tendon, 10 mm for the acupoint), it was left for 5 min without manipulation (Acu-1). Then, the tip of the needle was moved up and down from the targeted depth (up-and-down manipulation) at an approximately 1-mm amplitude and 2 Hz for 3 min (Acu-2). During Acu-2, the needle tip was moved at an approximately constant speed and frequency with the aid of a metronome, and the insertion depth was confirmed visually. After this technique, the needle was left for 2 min without manipulation (Acu-3).
Acupressure Acupressure was applied by one of the authors (A.Y.) (Fig. 2B). In the present study, we used a modified wooden stick (Tubo, Lieb Corporation, Japan) with a force sensor to monitor the pressing force during acupressure (Yasuda et al. 2022). This stick was pressed perpendicularly to the skin at 40 mm proximal to the calcaneus (stimulation of the tendon experiment) or the acupoint (stimulation of the acupoint experiment). Acupressure was performed at a frequency of 1.5 Hz for 3 min with a pressing force of 50 N, as described in our previous study (Yasuda et al. 2022).
Blood circulation of the Achilles tendon
During the experimental period, the blood circulation (oxyhemoglobin; Oxy, deoxyhemoglobin; Deoxy, total hemoglobin; THb, oxygen saturation; StO2) of the Achilles tendon was measured on both the treated and non-treated sides using a previously described procedure (Kubo et al. 2011, 2020a, b). First, a probe (SF-DS, Omega Wave, Tokyo, Japan) was positioned at 20 mm proximal to the calcaneus to measure the blood circulation of the tendon using red laser lights (BOM-L1TRSF, Omega Wave, Tokyo, Japan). This instrument uses three red laser lights (635, 650, and 690 nm) and calculates the relative tissue levels of Oxy, Deoxy, and THb (corresponding to the blood volume) according to the Beer-Lambert law. Oxy, Deoxy, THb, and StO2 at a specific depth (measurement depth of 3–5 mm) of the tissue could be measured by changing the location of the two detectors (Kashima 2003; Kubo et al. 2008).
In the present study, the units of Oxy, Deoxy, and THb are expressed as µmol / l, although this does not represent the actual physical volume. StO2 was calculated using the formula from Oxy and THb values: StO2 (%) = 100 · Oxy · THb−1. Our data were input into a personal computer at a sampling frequency of 10 Hz via an A/D transducer (Power Lab, AD Instruments, Australia). The mean values over a given duration (Acu-1, Acu-2, Acu-3, and every 10 min during the recovery period) were calculated using analytical software (Chart ver. 7.1, AD Instruments, Australia). Oxy, Deoxy, THb, and StO2 data are presented as the increase from the resting level. The repeatability of measurement of tendon blood circulation (Oxy, Deoxy, THb, and StO2) had been investigated in our previous studies (Kubo et al. 2008).
Statistical analysis
Values are reported as means ± SD. Two-way (site x time) analysis of variance (ANOVA) with repeated measures was used to detect significant differences in the measured variables from the resting level. One-way ANOVA was used to detect a significant difference in mean changes in THb during the recovery period among the four conditions (the treated and non-treated tendons due to the treatments of the tendon and acupoint). The F ratios for main effects and interactions were considered significant at p < 0.05. Significant differences among means at p < 0.05 were detected using the Tukey’s HSD post-hoc test. In ANOVA, Mauchly's sphericity test was performed to assess the homogeneity of variance. Greenhouse–Geisser correction was applied where the assumption of sphericity was violated. The effect size was calculated using partial eta-squared (pη2) for two-way ANOVA. Pearson product-moment correlations were computed to assess the associations among the measured variables. The level of significance was set at p < 0.05.
Results
The changes in the blood circulation of the treated and non-treated tendons due to acupuncture of the tendon are shown in Fig. 3A–D. For Oxy, THb, and StO2, the effect of time was significant (p = 0.024 pη2 = 0.299 for Oxy, p = 0.030 pη2 = 0.294 for THb, p = 0.024 pη2 = 0.264 for StO2), although the effects of site (p = 0.377 pη2 = 0.071 for Oxy, p = 0.514 pη2 = 0.040 for THb, p = 0.433 pη2 = 0.057 for StO2) and the interaction between site and time (p = 0.081 pη2 = 0.211 for Oxy, p = 0.144 pη2 = 0.169 for THb, p = 0.160 pη2 = 0.148 for StO2) were not significant. The post-hoc analysis identified significant increases for Oxy and THb at 20, 30, and 40 min points during the recovery period, although that did not identify significant differences for StO2 at any point. For Deoxy, the effects of site (p = 0.853 pη2 = 0.003) and time (p = 0.377 pη2 = 0.084) and the interaction between site and time (p = 0.851 pη2 = 0.011) were not significant.
A–D The changes in oxyhemoglobin (Oxy), deoxyhemoglobin (Deoxy), total hemoglobin (THb), and oxygen saturation (StO2) of treated (open circle) and non-treated (closed circle) tendons during acupuncture of the tendon and recovery periods. E–H The changes in oxyhemoglobin (Oxy), deoxyhemoglobin (Deoxy), total hemoglobin (THb), and oxygen saturation (StO2) of treated (open circle) and non-treated (closed circle) tendons during acupuncture of the acupoint and recovery periods. *Significantly different from the resting level (*p < 0.05, **p < 0.01, ***p < 0.001)
The changes in the blood circulation of the treated and non-treated tendons due to acupuncture of the acupoint are shown in Fig. 3E–H. For Oxy, Deoxy, THb, and StO2, the effects of site (p = 0.949 pη2 = 0.000 for Oxy, p = 0.739 pη2 = 0.010 for Deoxy, p = 0.848 pη2 = 0.004 for THb, p = 0.931 pη2 = 0.001 for StO2) and the interaction between site and time (p = 0.757 pη2 = 0.021 for Oxy, p = 0.702 pη2 = 0.027 for Deoxy, p = 0.791 pη2 = 0.015 for THb, p = 0.811 pη2 = 0.017 for StO2) were not significant. The effect of time for Oxy (p = 0.052 pη2 = 0.253), THb (p = 0.063 pη2 = 0.242), and StO2 (p = 0.109 pη2 = 0.195) tended to be significant, although that for Deoxy was not (p = 0.691 pη2 = 0.019).
No significant difference in the changes in THb during the recovery period after acupuncture of the tendon and acupoint for the treated and non-treated tendons was found among the four conditions (p = 0.492 pη2 = 0.069; Fig. 4). The changes in THb on the treated tendons during the latter half of the recovery period (21–40 min) were not correlated with the changes in THb on the non-treated tendons after acupuncture of the tendon (r = 0.459, p = 0.133) and acupoint (r = 0.382, p = 0.221) (Fig. 5).
The changes in the blood circulation of the treated and non-treated tendons due to acupressure of the tendon are shown in Fig. 6A–D. For Oxy, Deoxy, and THb, the effects of site (p = 0.002 pη2 = 0.538 for Oxy, p = 0.030 pη2 = 0.313 for Deoxy, p = 0.001 pη2 = 0.574 for THb) and time (p = 0.002 pη2 = 0.384 for Oxy, p = 0.002 pη2 = 0.389 for Deoxy, p < 0.001 pη2 = 0.437 for THb) and the interaction between site and time (p < 0.001 pη2 = 0.454 for Oxy, p = 0.014 pη2 = 0.318 for Deoxy, p < 0.001 pη2 = 0.490 for THb) were significant. Regarding the treated tendon due to acupressure of the tendon, the post-hoc analysis identified significant increases for Oxy, Deoxy, and THb at all time points during the recovery period (except for Deoxy at 10 min). For StO2, the effect of site (p = 0.525 pη2 = 0.032) and the interaction between site and time (p = 0.120 pη2 = 0.161) were not significant. Although the effect of time for StO2 was significant (p = 0.031 pη2 = 0.229), the post-hoc analysis did not identify significant differences at any point.
A–D The changes in oxyhemoglobin (Oxy), deoxyhemoglobin (Deoxy), total hemoglobin (THb), and oxygen saturation (StO2) of treated (open circle) and non-treated (closed circle) tendons before (rest) and after acupressure of the tendon (recovery). E–H The changes in oxyhemoglobin (Oxy), deoxyhemoglobin (Deoxy), total hemoglobin (THb), and oxygen saturation (StO2) of treated (open circle) and non-treated (closed circle) tendons before (rest) and after acupressure of the acupoint (recovery). *Significantly different from the resting level (**p < 0.01, ***p < 0.001) #significantly different from the non-treated side (#p < 0.05, ##p < 0.01, ###p < 0.001)
The changes in the blood circulation of the treated and non-treated tendons due to acupressure of the acupoint are shown in Fig. 6E–H. For Oxy, Deoxy, THb, and StO2, the effects of site (p = 0.233 pη2 = 0.107 for Oxy, p = 0.799 pη2 = 0.005 for Deoxy, p = 0.280 pη2 = 0.089 for THb, p = 0.204 pη2 = 0.121 for StO2) and time (p = 0.273 pη2 = 0.095 for Oxy, p = 0.620 pη2 = 0.028 for Deoxy, p = 0.260 pη2 = 0.099 for THb, p = 0.458 pη2 = 0.054 for StO2) and the interaction between site and time (p = 0.154 pη2 = 0.140 for Oxy, p = 0.854 pη2 = 0.007 for Deoxy, p = 0.175 pη2 = 0.130 for THb, p = 0.235 pη2 = 0.107 for StO2) were not significant.
The change in THb during the recovery period after acupressure of the tendon for the treated tendon was significantly greater than that of the tendon (p < 0.001) and acupoint (p < 0.001) for the non-treated tendon and that of the acupoint for the treated tendon (p = 0.005) (Fig. 7).
Discussion
Consistent with our previous studies (Kubo et al. 2010, 2011, 2020a, b), acupuncture stimulation of the tendon showed a rapid change in blood circulation on the treated tendon during acupuncture with up-and-down manipulation (Acu-2), with no change on the contralateral side (non-treated tendon). These changes during acupuncture with up-and-down manipulation are thought to be due to the release of neurotransmitters (e.g., substance P), resulting in axon reflex (Kashiba and Ueda 1991; Sato et al. 2000). During the recovery period after removal of the needle, tendon blood volume significantly increased on both the treated and non-treated sides (Fig. 3C). Unfortunately, no significant correlation was found between tendon blood volume on the treated and non-treated sides (Fig. 5), although several of our previous studies found significant correlations between the two (Kubo et al. 2011, 2020b). However, regarding acupuncture of the tendon, the increase in tendon blood volume of the treated tendon was significantly correlated with that of the non-treated one, if the outlier of one participant was excluded (r = 0.729, p = 0.011; Fig. 5A). Reasons for the discrepancies may include the number of participants (n = 17 in Kubo et al. 2011, n = 21 in Kubo et al. 2020b, n = 12 in the present study). In any case, the present results may be attributed to central effects via cholinergic vasodilator fibers (Inoue et al. 2001). On the other hand, both during and after acupuncture stimulation, Oxy increased, and Deoxy did not change (Fig. 3). These results are presumably due to increased blood inflow to the tendon via the axon reflex (primarily during acupuncture with up-and-down manipulation) and cholinergic vasodilator fibers (primarily during the recovery period). Thus, acupuncture of tendons altered blood circulation of the treated tendon by peripheral and central effects and the non-treated tendon by central effect.
Acupuncture of the acupoint did not change tendon blood circulation during acupuncture with up-and-down manipulation, unlike acupuncture of the tendon. Our inference that the increased blood circulation in the Achilles tendon with a needle insertion to this tendon is due to the axon reflex (Kashiba and Ueda 1991; Sato et al. 2000) is supported by the present finding that blood circulation in the Achilles tendon did not increase with a needle insertion to the acupoint. On the other hand, during the recovery period after the removal of the needle, blood volume tended to increase on both treated and non-treated tendons (effect of time p = 0.063; Fig. 3G). This result suggested that acupuncture of the acupoint acted to enhance blood inflow to tendons by cholinergic vasodilator fibers through the central nervous system (Inoue et al. 2001). However, the increase in tendon blood volume due to acupuncture of the acupoint did not show a significant correlation between the treated and non-treated sides as in the case of acupuncture of the tendon in the latter half of the recovery period (Fig. 5). Therefore, there may be a greater abundance of sensory nerves (related to cholinergic vasodilation) in the Achilles tendon than in the acupoint (Chengshan, BL57). Regardless, further studies using isolated animal tendons are needed to clarify this point.
We recently reported that acupressure of the tendon increased blood volume on both the treated and the non-treated tendons (Kubo et al. 2020a). In the present study, however, no change in blood volume on the non-treated tendon was observed. In this previous study (Kubo et al 2020a), no significant correlation was found between the increase in blood volume on the treated and non-treated tendons as in the case of acupuncture of tendons (data not shown in Kubo et al. 2020a). Furthermore, in Yasuda et al. (2022), we obtained a similar result in which blood volume on the non-treated tendon did not change when acupressure was applied to the Achilles tendon (data not shown in Yasuda et al. 2022). Although the reasons for these discrepancies in results are unknown, the possible reason is the method of acupressure, i.e., 5-mm amplitude and 1.5 Hz in Kubo et al. (2020a) and 50 N and 1.5 Hz in the present study. In any case, it can be said that, unlike acupuncture, acupressure in this study does not produce centrally mediated changes in tendon blood circulation. Regarding the difference in hemodynamic changes caused by both types of stimulation, it is speculated that the nociceptive stimulation of tissues by acupuncture causes peripheral vasodilatation through the autonomic nervous system at the spinal level by ascending Aδ and C fibers (Chae et al. 2013). Furthermore, unlike acupuncture, acupressure of the tendon increased Deoxy on the treated side, resulting in no significant increase in StO2. Therefore, it is likely that acupressure of the tendon alters tendon blood circulation by enhancing the metabolism of the treated tendon, which is due to a local rather than a systemic response.
Acupressure of the acupoint did not produce changes in blood circulation on either the treated or non-treated tendons, although acupuncture of the acupoint tended to change tendon blood circulation. These results indicated that the sensory nerves present in acupoints could be stimulated by acupuncture but not by acupressure. In this regard, it has been pointed out that the excitation by nociceptive stimulation with acupuncture may ascend Aδ and C fibers and cause a vasodilating effect via the autonomic nervous system at the level of the spinal cord (Pomeranz and Chui 1976; Pomeranz and Warma 1988). Thus, the microscopic tissue damage caused by acupuncture may be related to differences between acupuncture and acupressure in their effects on tendon blood circulation.
Based on the results of this study, in acupuncture, when there is pain in the affected area immediately after the injury, therapeutic effects can be expected by applying the treatment to acupoints that are distant from the affected area. Acupuncture treatment on Chengshan (BL57), the acupoint employed in the present study, has actually been shown to be effective in the treatment of Achilles tendon disorders (Zhang et al. 2017). In addition, experiments with animals reported that acupuncture with a low voltage electrical current at BL57 increased the concentration of collagen and the collagen fibril diameters in rat Achilles tendons, indicating the strengthening of the tendons (Almeida et al. 2012, 2015). Unfortunately, it is inferred that acupressure of acupoints is not effective in curing tendon disorders. However, acupressure may be useful as maintenance to prevent injury by increasing the metabolism of the tendon.
In the present study, we must draw attention to the limitations associated with the methodology followed. Firstly, the locations of acupoints are defined (by WHO) by the bone, muscle, blood vessels, etc. as indicators, but the locations as acupoints in individuals may differ from the difference of these anatomical landmarks. If so, differences in the location of acupoints in different individuals may affect the results of acupuncture and acupressure of acupoints. In this study, we used ultrasonography to define the stimulation location while confirming the boundary between the medial gastrocnemius muscle and lateral gastrocnemius muscle and the muscle–tendon junction of the gastrocnemius muscle with images. Secondly, changes in the blood circulation of the Achilles tendon were only measured 40 min after both acupuncture and acupressure. Further observation over a longer post-stimulation period is needed to examine the therapeutic effect on tendon disorders. Thirdly, all of the participants in this study were healthy and were not patients with tendon disorders. It cannot be ruled out that changes in tendon blood circulation in response to acupuncture or acupressure may differ between healthy participants and patients with tendon disorders. Future studies should be conducted on patients with tendon disorders to verify the therapeutic effects of acupuncture and acupressure treatment.
In conclusion, the main results of the present study were that (1) acupuncture of tendon and acupoint acted centrally to enhance blood circulation of both the treated and non-treated tendons during the recovery period after stimulation, and (2) acupressure of tendon locally increased tendon blood circulation by enhancing the metabolism of the treated tendon only, whereas acupressure of acupoint did not alter tendon blood circulation.
Abbreviations
- Acu:
-
Acupuncture
- ANOVA:
-
Analysis of variance
- Deoxy:
-
Deoxyhemoglobin
- Oxy:
-
Oxyhemoglobin
- pη2 :
-
Partial eta-squared
- SD:
-
Standard deviation
- StO2 :
-
Oxygen saturation
- THb:
-
Total hemoglobin
References
Ahmed IM, Lagopoulos M, McConnell P, Soames RW, Sefton GK (1998) Blood supply of the Achilles tendon. J Orthop Res 16(5):591–596
Alim MA, Domeij-Arverud E, Nilsson G, Edman G, Ackermann PW (2018) Achilles tendon rupture healing is enhanced by intermittent pneumatic compression upregulating collagen type I synthesis. Knee Surg Sports Traumatol Arthrosc 26:2021–2029
Almeida MS, Aro AA, Guerra FD, Vieira CP, Campos Vidal B, Rosa Pimentel E (2012) Electroacupuncture increases the concentration and organization of collagen in a tendon healing model in rats. Connect Tissue Res 53:542–547
Almeida MS, de Freitas KM, Oliveira LP, Vieira CP, Guerra Fda R, Dolder MA, Pimentel ER (2015) Acupuncture increases the diameter and reorganization of collagen fibrils during rat tendon healing. Acupunct Med 33:51–57
Arai YC, Ushida T, Matsubara T, Shimo K, Ito H, Sato Y, Wakao Y, Komatsu T (2011) The influence of acupressure at extra 1 acupuncture point on the spectral entropy of the EEG and the LF/HF ratio of heart rate variability. Evid Based Complement Alternat Med 2011:503698
Carr AJ, Norris SH (1989) The blood supply of the calcaneal tendon. J Bone Jt Surg 71B:100–101
Chae Y, Chang DS, Lee SH, Jung WM, Lee IS, Jackson S, Kong J, Lee H, Park HJ, Lee H, Wallraven C (2013) Inserting needles into the body: a meta-analysis of brain activity associated with acupuncture needle stimulation. J Pain 14:215–222
Chen AH, Frangos SG, Kilaru S, Sumpio BE (2001) Intermittent pneumatic compression devices—physiological mechanisms of action. Eur J Vasc Endovasc Surg 21:383–392
Fink M, Wolkenstein E, Karst M, Gehrke A (2002) Acupuncture in chronic epicondylitis: a randomized controlled trail. Rheumatology 41:205–209
Greve K, Domeij-Arverud E, Labruto F, Edman G, Bring D, Nilsson G, Ackermann PW (2012) Metabolic activity in early tendon repair can be enhanced by intermittent pneumatic compression. Scand J Med Sci Sports 22:e55–e63
Haker E, Lunderberg T (1990) Acupuncture treatment in epicondylalgia: a comparative study of two acupuncture techniques. Clin J Pain 6:221–226
Haker E, Egekvist H, Bjerring P (2000) Effect of sensory stimulation (acupuncture) on sympathetic and parasympathetic activities in healthy subjects. J Auton Nerv Syst 79(1):52–59
Hsiu H, Hsu WC, Chen BH, Hsu CL (2010) Differences in the microcirculatory effects of local skin surface contact pressure stimulateon between acupoints and nonacupoints: possible relevance to acupressure. Physiol Meas 31:829–841
Inoue M, Katayama K, Hojo T, Yano T, Katsumi Y (2001) The effects of electrical acupuncture to patellar tendon and electrical stimulation to femoral nerve on the blood flow of the patellar tendon in rat. Jpn J Phys Fitness Sports Med 50:119–128
Jarvinen M, Jozsa L, Kannus P, Jarvinen TLN, Kvist M, Leadbetter W (1997) Histopathological findings in chronic tendon disorders. Scand J Med Sci Sports 7:86–95
Kagitani F, Uchida S, Hotta H, Aikawa Y (2005) Manual acupuncture needle stimulation of the rat hindlimb activates groups I, II, III and IV single afferent nerve fibers in the dorsal spinal roots. Jpn J Pysiol 55:149–155
Kagitani F, Uchida S, Hotta H (2010) Afferent nerve fibers and acupuncture. Auton Neurosci 157:2–8
Kashiba H, Ueda Y (1991) Acupuncture to the skin induces release of substance P and calcitonin gene-related peptide from peripheral terminals of primary sensory neurons in the rat. Am J Clin Med 19:189–197
Kashima S (2003) Spectroscopic measurement of blood volume and its oxygenation in a small volume of tissue using red laser lights and differential calculation between two point detections. Opt Laser Technol 35:485–489
Kleinhenz J, Streitberger K, Windeler J, Gubbacher A, Mavridis G, Martin E (1999) Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendonitis. Pain 83:235–241
Kubo K, Ikebukuro T, Tsunoda N, Kanehisa H (2008) Noninvasive measures of blood volume and oxygen saturation of human Achilles tendon by red laser lights. Acta Physiol 193(3):257–264
Kubo K, Yajima H, Takayama M, Ikebukuro T, Mizoguchi H, Takakura N (2010) Effects of acupuncture and heating on blood volume and oxygen saturation of human Achilles tendon in vivo. Eur J Appl Physiol 109:545–550
Kubo K, Yajima H, Takayama M, Ikebukuro T, Mizoguchi H, Takakura N (2011) Changes in blood circulation of the contralateral Achilles tendon during and after acupuncture and heating. Int J Sports Med 32:807–813
Kubo K, Iizuka Y, Yajima H, Takayama M, Takakura N (2020a) Acupuncture- and intermittent compression-induced changes in blood circulation of tendon. J Alter Comp Med 26:231–238
Kubo K, Iizuka Y, Yajima H, Takayama M, Takakura N (2020b) Changes in blood circulation of the tendon and heart rate variability during and after acupuncture. Med Acupunct 32:99–107
Li AH, Zhang JM, Xie YK (2004) Human acupuncture points mapped in rats are associated with excitable muscle/skin-nerve complexes with enriched nerve endings. Brain Res 1012:154–159
Li X, Hirokawa M, Inoue Y, Sugano N, Qian S, Iwai T (2007) Effects of acupressure on lower limb blood flow for the treatment of peripheral arterial occlusive diseases. Surg Today 37:103–108
Litscher G, Wang L, Huber E, Nilsson G (2002) Changed skin blood perfusion in the fingertip following acupuncture needle introduction as evaluated by laser Doppler perfusion imaging. Lasers Med Sci 17:19–25
Matsubara T, Arai YC, Shiro Y, Shimo K, Nishihara M, Sato J, Ushida T (2011) Comparative effects of acupressure at local and distal acupuncture points on pain conditions and autonomic function in females with chronic neck pain. Evid Based Complement Alternat Med 2011:543291
Nishijo K, Mori H, Yoshikawa K, Yazawa K (1997) Decreased heart rate by acupuncture stimulation in humans via facilitation of vagal cardiac activity and suppression of cardiac sympathetic nerve. Neurosci Lett 227(3):165–168
Pomeranz B, Chui D (1976) Naloxone blockade of acupuncture analgesia: endorphin implicated. Life Sci 19:1757–1762
Pomeranz B, Warma N (1988) Electroacupuncture suppression of a nociceptive reflex is potentiated by two repeated electroacupuncture treatments: the first opioid effect potentiates a second non-opioid effect. Brain Res 452:232–236
Praxitelous P, Edman G, Ackermann PW (2018) Microcirculation after Achilles tendon rupture correlates with functional and patient-reported outcomes. Scand J Med Sci Sports 28:294–302
Sandberg M, Lundeberg T, Lindberg LG, Gerdle B (2003) Effects of acupuncture on skin and muscle blood flow in healthy subjects. Eur J Appl Physiol 90:114–119
Sato A, Sato Y, Shimura M, Uchida S (2000) Calcitonin generated peptide produces skeletal muscle vasodilation following antidromic stimulation of unmyelinated afferents in the dorsal roots in rats. Neurosci Lett 283:137–140
Stein V, Laprell H, Tinnemeyer S, Petersen W (2000) Quantitative assessment of intravascular volume of the human Achilles tendon. Acta Orthop Scand 71(1):60–63
Yasuda A, Sasajima S, Kosaka T, Kubo K (2022) Changes in tendon blood circulation and heart rate variability after intermittent compression to patellar and Achilles tendons. Clin Biomech 97:105690
Zantop T, Tillmann B, Petersen W (2003) Quantitative assessment of blood vessels of the human Achilles tendon: an immunohistochemical cadaver study. Arch Orthop Trauma Surg 123:501–504
Zhang WT, Jin Z, Luo F, Zhang L, Zeng YW, Han JS (2004) Evidence from brain imaging with fMRI supporting functional specificity of acupoints in humans. Neurosci Lett 354:50–53
Zhang D, Ye X, Zhang X, Zhang W (2017) The application of the contralateral acupuncture for rehabilitation after acute closed achilles tendon rupture. Zhongguo Zhen Jiu 37(3):237–241
Acknowledgements
This study was supported by a Grant-in-Aid for Scientific Research (B) (17H02149 and 20H04070 to K. Kubo) from the Japan Society for the Promotion of Science. The authors thank Mr. Iizuka Y. for his technical assistance with the measurements and Dr. Takeshita D. (The University of Tokyo) for help with statistics.
Funding
Open access funding provided by The University of Tokyo.
Author information
Authors and Affiliations
Contributions
KK: conception of this study, drafting the manuscript. Ayaka Yasuda; acquisition of data, analysis data. HY: acquisition of data. MT: drafting the manuscript. NT: conception of this study, drafting the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
I have no conflict of interest with this work.
Additional information
Communicated by Olivier Seynnes.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kubo, K., Yasuda, A., Yajima, H. et al. Effects of acupuncture and acupressure of the acupoint compared to the tendon on the blood circulation of human tendon in vivo. Eur J Appl Physiol 124, 269–279 (2024). https://doi.org/10.1007/s00421-023-05277-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-023-05277-2