Abstract
Purpose
Osteopenia is common in postmenopausal women and effective interventions increasing or stabilizing bone mineral density (BMD) to prevent fractures are urgently needed.
Methods
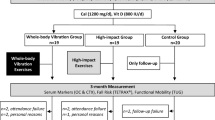
Sixty-five postmenopausal women diagnosed with osteopenia (T-score between -1.0 and -2.5) were randomly assigned to either a vibration training group (VT), a resistance training group (RT), or a control group (CG). BMD T-score values (primary endpoint) were assessed at baseline (T0) and after 12 months (T12), secondary endpoints (muscle strength, postural control, and health-related quality of life) at baseline (T0), after 6 months (T6), after 12 months (T12), and as follow-up after 15 months (T15).
Results
After the intervention period, neither the VT nor the RT showed any significant changes in BMD T-score values compared to the CG. Isokinetic strength improved significantly within all training groups, with the exception of the flexors of VT at an angular velocity of 240°/s. Health-related quality of life as well as postural control improved significantly for the RT only.
Conclusions
We conclude that participants of all three groups were able to maintain their BMD. The improvements in quality of life and postural control after resistance training are nevertheless meaningful for postmenopausal osteopenic women and support the importance of regular loadings of the musculoskeletal system.
This study was retrospectively registered in January 2022 at the DRKS (S00027816) as clinical trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Osteoporotic fractures are a major individual and socioeconomical burden in our aging society (Burge et al. 2007). Therefore, prevention of osteoporosis is essential. Osteopenia is considered a precursor to osteoporosis and is characterized by T-score values between − 1.0 and − 2.5. At this stage at the latest, interventions to increase or maintain bone mineral density (BMD) are justified.
Resistance training positively affects both BMD (Howe et al. 2011) and muscle strength (Macaluso and De Vito 2004). However, patients’ adherence and compliance with this lifelong training intervention is less than optimal. Strenuous exercises, generating high-intensity loading forces to the skeleton (Marques et al. 2012), can be challenging and require regular, at least weekly visits to training facilities. Alternative, less-demanding and time-efficient training regimes are therefore of utmost importance for a good prognosis.
Whole body vibration training (WBVT) is a promising intervention that increases muscle strength (Machado et al. 2010) and balance (Ritzmann et al. 2014). In fact, enhanced markers of bone formation (Chung et al. 2014; Xie et al. 2006) and bone density (Wenger et al. 2010) have been reported in animal studies. There is conflicting evidence in humans. While some authors found increases in BMD after WBVT (e.g., Zha et al. 2012; Iwamoto et al. 2005; Verschueren et al, 2004; Von Stengel et al. 2011a, b), others reported no effect (e.g., Liphardt et al. 2015; Slatkovska et al. 2011). In addition, previous meta-analysis were not able to clarify the effect of WBVT on BMD (Lau et al. 2011; Oliveira et al. 2016;). One explanation might be the large heterogeneity in study designs, delivery of intervention (e.g., intensity, length of intervention), and WBVT specifications ranging from 12 to 113 Hz, 0.2 to 32.2 g or 0.005 to 8 mm amplitude (Lau et al. 2011). A previously published meta-analysis (Fratini et al. 2016) suggests that training in a static squatting position on a side-alternating vibration platform with accelerations ≥ 3 g is the most effective WBVT protocol to enhance BMD in the hip and lumbar spine in postmenopausal women. However, when these settings were used in osteopenic women, no beneficial effects of WBVT were found on BMD in the lumbar spine or the femoral neck, bone microarchitecture of the distal radius and the tibia, or balance and strength (Liphardt et al. 2015). Of note, the participants performed the same WBVT static squatting settings during the 12 month intervention period. For this long period of time, load progression might be necessary to provide further physiological adaptation stimuli. In addition, BMD for the total hip was not reported by Liphardt et al. (2015). However, this whole area has been shown to be specifically stimulated using side altering vibration platforms (Rittweger 2010). Therefore, some regional effects of WBVT on BMD need further evaluation.
Aims
Hence, the primary objective of this study was to investigate the effects of progressive WBVT and resistance training in postmenopausal osteopenic women on BMD T-score values of the total hip and lumbar spine. Secondary objectives were effects of WBVT and resistance training on strength, balance, and quality of life. Both interventions were compared to a control group (CG).
Methods
Study design
This study was designed as a single-blinded, randomized controlled trial including three study groups: a vibration training group (VT), a resistance training group (RT), and a control group (CG). The intervention period lasted for 12 months and included two training sessions per week. A follow-up examination was performed 3 months after the end of the active intervention period. Patients were randomly allocated by using sealed opaque envelopes (n = 90) of a 1:1:1 ratio of VT, RT, and CG. All physicians remained blinded to the patient’s allocation. Due to the nature of the intervention, participants could not be blinded. Patient identity was independently coded after enrollment and decoded after data analysis.
Participants
Eligible participants were postmenopausal women aged ≥ 45. Postmenopausal was defined as 12 consecutive months without menstruation. Exclusion criteria included: acute disc prolapse, acute thrombosis, acute inflammation of the musculoskeletal system, kidney or bladder stones, acute hernias, epilepsy, seizures, pregnancy, arrhythmias, pacemaker, osteoporotic-induced fractures, multiple sclerosis, chronic obstructive pulmonary disease, uncontrolled angina pectoris, coronary heart disease, uncontrolled cardiac failure, high-grade aortic stenosis, hypertrophic cardiomyopathy, dizziness, surgery, or hospitalization within the previous 6 months and receiving any drug treatment for osteoporosis affecting bone metabolism and/or muscle strength within the last year.
Recruitment
Eligible participants were identified at the University Institute of Nuclear Medicine and Endocrinology, Paracelsus Medical University, Salzburg. BMD T-score values were determined by dual-energy X-ray absorptiometry (DXA- QDR 4500 W, Hologic, Marlborough, Mass., USA) on the left side of the hip and at the lumbar spine (L1-L4). Subjects were diagnosed as osteopenic when T-score values between − 1.0 and − 2.5 were measured at least at one of these sites. Patients, who met inclusion and none of the exclusion criteria, were invited to participate in the trial. All patients were fully informed about the research purpose, possible adverse events but also expected health benefits. Recruitment took place from February 2010 to June 2012.
Intervention programs
Two sport scientists at the Institute of Physical Medicine and Rehabilitation supervised the intervention from March 2010 to December 2013. Standardized training programs (vibration and resistance training group) were applied as described below.
Vibration training
The VT group performed different exercises standing barefoot on a side-alternating vibration platform (Galileo Sport, Typ 8N056001C, Pforzheim, Germany) twice a week for 12 months. The exercises were introduced gradually, depending on the physical condition of the patients. During the first 3 weeks, patients began static squats with a knee angle of about 30° (0° = full extension) three times for 1 min (frequency (f): 18 Hz, amplitude (A): 2 mm) with 1 min rest between repetitions, increasing to 6 repetitions (f: 20 Hz, A: 2 mm) of 1 min each, corresponding to approximately 3.2 G (calculated with the equation g = A(2πf)2/9.81). After 3 weeks of static squatting and reaching the target frequency, load progression was ensured by adding dynamic upper body exercises (e.g., by lifting dumbbells or using swing sticks) during the static squat. In this phase, patients performed three static squats of 1 min each without and three static squats with upper body exercises on the vibration plate. If this was well tolerated by the patients, additional dynamic squats were added to the program. Finally, one training session included 2 bouts of static squats without upper body movement, 2 bouts of static squats with different upper body exercises, and 2 bouts of dynamic squats (supplemental material 1). Exercises were added for patients only if the present program could be performed without problems (for example balance). Before vibration, patients began their exercise session with a 10-min warm-up on a bicycle ergometer (Daum electronic, Fürth, Germany) at 1.0 W/kg and a cadence of 50–70 per minute and ended it after vibration with a cool-down, including stretching of the leg, hip, and lumbar muscles. In total, the entire training lasted about 30 min.
Resistance training
Patients in the RT group trained according to the Austrian recommendations for health-promoting activity for (older) adults, consisting of 10–15 repetitions to the point of volitional fatigue, 2–3 series of all large muscle groups (Titze et al. 2010). Resistance exercise training was performed twice a week for 12 months at the Institute of Physical Medicine and Rehabilitation, University Hospital Salzburg, Austria under the supervision of sport scientists. Each training session lasted for about 45 min in total. Resistance training started with a 10 min warm-up on a cycle (Daum electronic, ergo bike Medical8, Fürth, Germany) or upper body ergometer (Proxomed, kardiomed upper body cycle, Typ 2011, Alzenau, Germany) followed by balance exercises for another 10–15 min, e.g., on wobble boards. Afterward, resistance training was performed on 6 different machines: leg press, leg abduction, leg flexion, leg extension, latissimus machine, and pulley. During the first 12 weeks of resistance training, the intensity was systematically increased from three sets of 20 repetition of 50–60% one repetition maximum (RM) to three sets of 10–15 repetitions of 70% 1RM (supplemental material 1). Weights were noted for each individual patient and adjusted every 2 weeks.
Control group
Subjects of the CG were instructed to maintain their current level of physical activity during the study period and not to engage in any new form of exercise.
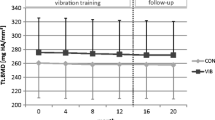
Data assessment and acquisition
BMD T-score values were measured at baseline (T0) and after 12 months (T12). Isokinetic strength, balance, and quality of life were assessed at baseline (T0), 6 (T6), 12 (T12), and 15 (T15) months (Fig. 1).
Primary outcome
At baseline (T0) and 12 months (T12), BMD was determined by DXA on the left side of the hip and the lumbar spine (L1–L4) (Tothill and Hannan 2007). Coefficients of variation have previously been reported as 1.3% for the lumbar spine and 1.4% for the femoral neck region (Von Stengel et al. 2011a, b). All scans were done by an experienced technician, who was blinded to the patients´ group allocation. An overview of the data collection and outcome assessment is presented in Fig. 1.
Secondary outcomes
Isokinetic muscle strength assessment
The isokinetic strength of the participants’ left knee extensors and flexors was measured on an isokinetic dynamometer (BIODEX System 3 and 4Pro, Biodex Medical Systems, USA) at baseline (T0), 6 (T6), 12 (T12), and 15 (T15) months (Fig. 1). The test–retest-reliability of this method has already been shown by Feiring et al. (1990) (knee extension peak torque at 60 degrees/sec (°/s), r = 0.95 and at 240°/s, r = 0.95). The test was done at two different angular velocities 60°/s with 5 repetitions (reps) and 240°/s with 25 reps. With these two test speeds, on the one hand, the maximum torque during a slow muscle contraction (60°/s) and thus approximately 66% of the maximum muscular power was determined and on the other hand, the faster muscle contraction (240°/s), which from a functional point of view corresponds to the speed of movement of the knee joint during human gait at 4 km/h. Patients were allowed to have 3–5 trial repetitions at each angular velocity directly before the outcome assessment. Between the different angular velocities, patients had a 90-s resting period. Relative peak torque to body mass (DMM/kg) at each testing speed was used to determine knee extension and flexion strength.
Postural control assessment
Postural control was measured by the “GGT” balance test (GGT: Acronym for the German word “Gleichgewichtstest”, i.e., balance test in English) (Bös et al. 1992). Quality criteria of this postural assessment were followed (Wydra 1993). This assessment consisted of 14 different items that determine static and dynamic balance ability. Each item consists of exercises with increasing difficulty. The more exercises one completes per item, the higher the score. The balance test was performed at baseline (T0), 6 (T6), 12 (T12), and 15 (T15) months (Fig. 1).
Health-related quality of life
The EQ-5D-3L questionnaire, self-administrated by the participants, was used to evaluate health-related quality of life (EuroQolGroup, 1990). The validity and reliability of the EQ-5D has been assessed for the different language versions and various health conditions (Van Hout et al. 2012). EQ-5D-3L index (EQ Index) and EQ visual analogue scale (EQ-VAS) were analyzed according to the manual. The questionnaire was completed at baseline (T0) and after 6 (T6), 12 (T12), and 15 (T15) months (Fig. 1).
Statistical analysis
All statistical analyses were performed with IBM SPSS Statistics 23.0. Figures were produced using the GraphPad Prism 9.0.0 (GraphPad Software Inc., La Jolla, United States). We evaluated our primary endpoint in an intention-to-treat analysis according to the CONSORT guidelines for the reporting of randomized controlled trials (Schulz et al. 2010). We applied the method of Baseline Observation Carried Forward (BOCF) for missing data with respect to the primary endpoint (T-score). A per-protocol analysis was performed for all secondary endpoints. To be included into the per-protocol analysis, the training compliance needed to be 80% or higher, achieved by 16 women (76.2%) in the VT and 19 women (79.2%) in the RT. All tests were two-tailed, and a 5% probability level was considered significant. The Shapiro–Wilk test was used to check for normal distribution. Homogeneity of variance was determined using Levine’s F test. The intervention effects on primary and secondary endpoints were tested using the Kruskal–Wallis test to compare the delta values (baseline – follow-up, mean differences) of the groups. Within-group differences in pre-post-analysis were tested using the t test for paired samples (primary endpoint). The Friedman test was used analyzing within-group differences of all secondary endpoints. A post hoc Dunn–Bonferroni test was calculated for parameters with significant group difference. For comparison of baseline characteristics of the three groups, a one-way ANOVA was used for normally distributed variables.
Results
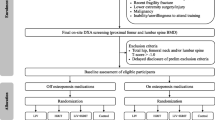
Participants, recruitment, and process evaluation
A total of 67 eligible patients signed informed consent. Two patients did not meet inclusion criteria; therefore, 65 patients were randomly allocated to one of the three study groups. Four patients withdrew consent after randomization (all CG), leaving 61 patients for intention-to-treat analysis (VT n = 18; RT n = 22; CG n = 21). Eight subjects retired early from the study: three due to non-intervention related injuries, four did not respond to invitations for follow-up measurements, and one due to severe chronic illness (breast cancer). Figure 2 shows the detailed CONSORT flow diagram of the study. In seven patients (VT n = 2; RT n = 3; CG n = 2), the final T-scores had to be implemented due to loss of follow-up with the data carried forward method. The mean number of exercise sessions in the VT was n = 93 (± 7) and in the RT n = 89 (± 7), with an achievable maximum of 104 sessions. The leisure time activity level was assessed for each patient at baseline using the IPAQ questionnaire (version 2005). There were no baseline differences in the metabolic equivalent-minutes per week between groups (p = 0.154). Intensity categories (low, moderate, high) were formed according to the IPAQ manual (version 2005) and presented for each group in the supplemental material 2. All baseline characteristics of the participants are presented in Table 1.
Follow-up results
Primary endpoint
Twelve months of WBVT or resistance training did not demonstrate any statically significant effect on BMD (T-score) compared with the CG. The results from the per-protocol and sensitivity analysis were similar to those obtained in the intention-to-treat analysis (Table 2; Fig. 3). Furthermore, no significant changes were seen in the left-sided hip or lumbar spine (T-score) in any group (Table 3). In addition, we analyzed the BMD of the femoral neck as an important subregion of the hip. However, there were no significant changes in any group after the 12-month intervention period in T-score values: VT from − 1.77 ± 0.67 to − 1.74 ± 0.66 (p = 0.653); RT from − 1.54 ± 0.66 to − 1.62 ± 0.64 (p = 0.069); CG from − 1.63 ± 0.53 to − 1.68 ± 0.66 (p = 0.382).
Bone mineral density of the left hip and lumbar spine before (T0) and at the end of intervention (T12) in the vibration training (VT) group, the resistance training (RT) group, and the control group (CG). Individual values are presented together with means ± SD according to the intention-to-treat analysis
Secondary endpoints: between group analysis
Isokinetic muscle strength
The analysis of isokinetic muscle strength between the groups showed a statistically significant difference in knee extensors, calculated as the mean difference between the baseline (T0) and 6 (T6) months at an angular velocity of 60°/s (χ2 = 8.971, p = 0.011) and 240°/s (χ2 = 16.567, p = 0.000) and between the baseline (T0) and 12 (T12) months at an angular velocity of 240°/s (χ2 = 6.694, p = 0.035) (supplemental material 3). After 6 months, there was a difference in the left knee extensors at an angular velocity of 60°/s between the RT and the CG (p = 0.017, r = 0.46) (supplemental material 4). An effect was also observed in the left knee extensors at an angle velocity of 240°/s (p > 0.000, r = 0.66) (supplemental material 4), which was greater in the VT than in the CG (p = 0.018, r = 0.46) (supplemental material 4). After 12 months, there was a difference in the left knee extensors at an angle velocity of 240°/s between the RT and the CG (p = 0.030, r = 0.42) (supplemental material 4).
Health- related quality of life (EQ-5D)
After 12 months, EQ-VAS in the RT was significantly improved compared to the CG (p = 0.013, r = 0.48) (supplemental material 3 and 4).
Postural control
For the balance test, no differences between the groups were found at any measurement point.
After 15 months of follow-up (T15), there were no statistically significant differences for the secondary endpoints between groups (supplemental material 1).
Secondary endpoints: within-group analysis
Isokinetic muscle strength
The isokinetic strength measurements showed statistically significant improvement in all groups, with the exception of the knee extensors at an angle velocity of 60°/s in the CG (χ2 = 7.473, p = 0.058) and the knee flexors at an angle velocity of 240°/s in the VT (χ2 = 6.600, p = 0.058) (Table 4).
Health-related quality of life (EQ-5D)
The VAS of the EQ-5D was statistically significantly improved only in the RT (χ2 = 8.165, p = 0.043) (Table 4).
Postural control
There was a statistically significant difference in the balance test only in the RT (χ2 = 16.895, p = 0.001) (Table 4). All results of the analysis within the group are presented in Table 4 and supplemental material 5 (post hoc tests).
Discussion
We set out to assess the effects of WBVT and resistance training on BMD T-scores, muscle strength, postural control, and quality of life in comparison to a CG in postmenopausal, osteopenic women. After the 12-month intervention, neither WBVT nor resistance training showed any statistical benefit for BMD T-score values of the lumber spine and total hip as compared to the CG. With two exceptions (CG: 60°/s extensors, VT: 240°/s flexors), there was a significant improvement in muscle strength in the lower extremity within the three study groups (Table 4). This may possibly be due to getting used to the device, although a period of 6 months passed between the first three tests (T0, T6, and T12) and another 3 months between the end of the study (T12) and follow-up (T15). For this reason, however, it is not usual to perform a completely independent, non-evaluated test run on the isokinetic force measurement system. Despite the significant improvements within the groups (Table 4), there are several significant differences between the two intervention groups (VT and RT) and the CG (supplemental material 4), which in turn point to an even bigger increase in strength through physical training. Nevertheless, it is possible that the strength gain of the two intervention groups was not higher due to the training intensity chosen. It is known from the literature that most successful training protocols are using loads corresponding to 80% of 1RM (Marques et al. 2012). Patients of our RT group trained on average with 70% 1RM which could explain the lower strength increases for this group. The achievement of the necessary intensity is also always influenced by personal factors (e.g., motivation, willingness to do exercise until volitional fatigue, fear of injuries, good/bad previous experience with strength training, etc.) and the supervising team can only have limited influence on this. An improvement in the health-related quality-of-life score and balance was observed only in the RT. These beneficial effects on secondary endpoints were lost 3 months after the intervention period (T15). These findings highlight the importance of maintaining an active lifestyle.
Comparison with existing literature
The non-superiority of WBVT and resistance training as compared to the CG in maintaining BMD is in line with findings of Liphardt et al. (2015) and Mohammad Rahimi et al. (2020). Using comparable vibration settings but different training positions, Liphardt et al. (2015) observed similar declines in BMD and bone architectural parameters in the vibration and the non-training control groups after 20-month follow-up. T-score values in our study remained constant in all groups, but unlike Liphardt et al. (2015), this was only assessed after 12 months. The intervention period may have been too short to detect any significant differences between groups. In addition, resistance training had no beneficial effects on BMD, which is in contrast to current literature (Howe et al. 2011). The work of Howe et al. (2011) demonstrates that especially high impact activities like running/jumping or resistance training exercises using high weights were successful in increasing BMD of the spine, the total hip, or the femoral neck. Consequently, the selected loads of the RT group in our study (70% 1RM) may have been somewhat too low. Additionally, we expected that the chosen vibration settings would produce the necessary impact loads to the skeletal system for triggering anabolic responses. However, the pure vibration time in the VT group was 6 min, which was lower compared to other successful vibration protocols with 12 min (Verschueren et al. 2004) or 10 min (von Stengel et al. 2011a, b). Even high load strength training programs (6–8 exercise machines, 3 sets of 8 repetitions per machine) have a longer load time of about 7.5–10 min, assuming 8 repetitions are performed in 25 s. The lower effective training time could therefore be a further explanation for the lack of improvements in this group. Continuous increases in knee extensor strength were observed in the VT, which is consistent with the current literature (Verschueren et al. 2004; Von Stengel et al. 2011a, b). Of note, our findings demonstrate that participants in the RT and the CG showed improvements for the knee flexors, too. In the RT, study participants showed an almost continuous improvement of knee extensor as well as flexor strength (supplemental material 5). This is in line with the existing literature (Siegrist et al. 2006; Verschueren et al. 2004). Heavy exercise is less attractive in older adults with possible negative impact on long-term adherence, and might expose them to an increased risk of injuries (Von Stengel et al. 2011a, b). Nevertheless, the training settings applied seem to be adequate in postmenopausal women for increasing lower extremity strength without decreasing compliance. This is also supported by the low number of dropouts (RT n = 3) during the study period. However, small improvements in knee flexor strength were also observed for the CG, ranging from 4 to 16 Nm. These improvements are probably more related to learning effects than to strength gains. Therefore, these variables have to be interpreted with caution.
Increases in postural control were exclusively found in the RT, possibly due to the 10–15 min balance training. The sensorimotor input via vibration training in our study seems insufficient to improve balance, which is in contrast to a previous report of 8 months of WBVT, showing a significant difference in balance skills, determined by the blind flamingo test (Gusi et al. 2006). In addition, a meta-analysis and systematic review by Ma et al. (2016) reported improvement of fall related factors (e.g., isometric strength, balance, and fall rate) through WBVT. Since we did not record the number of falls, we cannot make any assumptions about the effects that our interventions might have had.
Health-related quality of life assessed by EQ-5D-3L showed increased solely for the RT but only after 12 months of training. It is well known that prolonged physical activity positively affects self-efficacy, self-esteem, and quality of life (Bize et al. 2007).
Study strengths and limitations
Our study has several strengths and some limitations. All study participants were treated and tested in a 12-month RCT at one institution by specially trained personnel. The compliance was high, indicating that the exercise program was attractive. No adverse events related to the interventions were reported, indicating that WBVT and resistance training are safe treatment options in postmenopausal osteopenic women.
The isokinetic muscle strength significantly increased within all three study groups. This effect was not present when comparing mean differences between the intervention and control group. This may at least partly be due to a Hawthorne effect in the CG mitigating the success of the intervention.
There were baseline differences in age and muscle strength between groups. Patients of the RT group were significantly older and weaker which could have influenced a possible training effect. A study period of 12 months might be too short to induce measurable and meaningful effects of WBVT or resistance training on BMD as compared to our CG. Based on our results and existing evidence, an intervention period of at least 24 months is recommended. Unfortunately, we did not have full access to information on patients’ medication, and therefore, we cannot exclude that some patients might have taken vitamin D supplementation beyond the standard dosage of 800 IE per day.
Furthermore, we are aware that the EuroQol tool (EQ-5D-3L) has its limitations concerning the assessment of health-related quality of life.
Conclusion
In conclusion, WBVT or resistance training did not lead to significant improvement in BMD (T-score) in postmenopausal osteopenic women after 12 months of controlled intervention compared to physically inactive controls. Muscle strength was improved in the VT and the RT, but improvements were also seen in the CG. In summary, there is limited evidence to determine training intensity and duration of WBVT in postmenopausal women with osteopenia when the treatment goal is defined as an increase in BMD. Nevertheless, health-related quality of life and postural control can be improved by resistance training, which is of clinical relevance for postmenopausal osteopenic women strengthening the importance of regular loading of the musculoskeletal system.
Abbreviations
- A:
-
Amplitude
- BMD:
-
Bone mineral density
- CG:
-
Control group
- Df:
-
Degree of freedom
- DMM/kg:
-
Relative peak torque to body mass
- F:
-
Frequency
- G:
-
Gravity (9.80665 m/s2)
- GGT:
-
“Gleichgewichtstest”/ balance test
- Hz:
-
Hertz
- MET:
-
Metabolic equivalent
- N:
-
Number
- r:
-
Pearson correlation coefficient
- RM:
-
Repetition maximum
- RT:
-
Resistance training group
- SD:
-
Standard deviation
- T0:
-
Baseline
- T6:
-
After 6 month interventions
- T12:
-
After 12 month interventions
- T15:
-
Follow-up after 15 months after start of interventions
- VAS:
-
Visual analogue scale
- VT:
-
Vibration training group
- WBVT:
-
Whole body vibration training
- χ2 :
-
Chi-square
References
Altman DG (2009) Missing outcomes in randomized trials: addressing the dilemma. Open Med 3(2):e51-53
Bize R, Johnson JA, Plotnikoff RC (2007) Physical activity level and health related quality of life in the general adult population: a systematic review. Prev Med 45:401–415. https://doi.org/10.1016/j.ypmed.2007.07.017
Bös K, Wydra G, Karisch G (1992) Gesundheitsförderung durch Bewegung, Spiel und Sport. Ziele und Methoden des Gesundheitssports in der Klinik. Perimed, Erlangen
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. JBMR 22:465–475. https://doi.org/10.1359/jbmr.061113
Chung SL, Leung KS, Cheung WH (2014) Low-magnitude high-frequency vibration enhances gene expression related to callus formation, mineralization and remodeling during osteoporotic fracture healing in rats. J Orthop Res 32:1572–1579. https://doi.org/10.1002/jor.22715
EuroQolGroup (1990) EuroQol- a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Feiring DC, Ellenbecker T, Derscheid GL (1990) Test-Retest Reliability of the Biodex Isokinetic Dynamometer. JOSPT 11:298–301
Fratini A, Bonci T, Bull AM (2016) Whole body vibration treatments in postmenopausal women can improve bone mineral density: results of a stimulus focussed meta-analysis. PLoS ONE 11:e0166774. https://doi.org/10.1371/journal.pone.0166774
Gusi N, Raimundo A, Leal A (2006) Low-frequency vibratory exercise reduces the risk of bone fracture more than walking: a randomized controlled trial. BMC Musculoskelet Disord 92:1–8. https://doi.org/10.1186/1471-2474-7-92
Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C et al (2011) Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD000333.pub2
Iwamoto J, Takeda T, Sato Y, Uzawa M (2005) Effect of whole-body vibration exercise on lumbar bone mineral density, bone turnover, and chronic back pain in post-menopausal osteoperotic women treated with alendonate. Aging Clin Exp Res 17:157–163
Lau RW, Liao LR, Yu F, Teo T, Chung RC, Pang MY (2011) The effects of whole body vibration therapy on bone mineral density and leg muscle strength in older adults: a systematic review and meta-analysis. Clin Rehabil 25:975–988. https://doi.org/10.1177/0269215511405078
Liphardt AM, Schipilow J, Hanley DA, Boyd SK (2015) Bone quality in osteopenic postmenopausal women is not improved after 12 months of whole-body vibration training. Osteoporos Int 26:911–920. https://doi.org/10.1007/s00198-014-2995-8
Ma C, Liu A, Sun M, Zhu H, Wu H (2016) Effect of whole-body vibration on reduction of bone loss and fall prevention in postmenopausal women: a meta-analysis and systematic review. J Orthop Surg Res 11:1–8. https://doi.org/10.1186/s13018-016-0357-2
Macaluso AE, De Vito G (2004) Muscle strength, power and adaptations to resistance training in older people. Eur J Appl Physiol 91:450–472. https://doi.org/10.1007/s00421-003-0991-3
Machado A, Garcia-Lopez D, Gonzalez-Gallego J, Garatachea N (2010) Whole-body vibration training increases muscle strength and mass in older women: a randomized-controlled trial. Scand J Med Sci Sports 20:200–207. https://doi.org/10.1111/j.1600-0838.2009.00919.x
Marques EA, Mota J, Carvalho J (2012) Exercise effects on bone mineral density in older adults: a meta-analysis of randomized controlled trials. Age 34:1493–1515. https://doi.org/10.1007/s11357-011-9311-8
Mohammad Rahimi GR, Smart NA, Liang MTC, Bijeh N, Albanaqi AL, Fathi M, Niyazi A, Mohammad Rahimi N (2020) The impact of different modes of exercise training on bone mineral density in older postmenopausal women: a systematic review and meta-analysis research. Calcif Tissue Int 106:577–590. https://doi.org/10.1007/s00223-020-00671-w
Oliveira LC, Oliveira RG, Pires-Oliveira DA (2016) Effects of whole body vibration on bone mineral density in postmenopausal women: a systematic review and meta-analysis. Osteoporos Int 27:2913–2933. https://doi.org/10.1007/s00198-016-3618-3
Rittweger J (2010) Vibration as an exercise modality: how it may work, and what its potential might be. Eur J Appl Physiol 108:877–904. https://doi.org/10.1007/s00421-009-1303-3
Ritzmann R, Kramer A, Bernhardt S, Gollhofer A (2014) Whole body vibration training – improving balance control and muscle endurance. PLoSONE 9:e89905. https://doi.org/10.1371/journal.pone.0089905
Schulz KF, Altman D, Mohrer D (2010) Consort 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med 8:1–9
Siegrist M, Lammel C, Jeschke D (2006) Krafttraining an konventionellen bzw. oszillierenden geräten und wirbelsäulengymnastik in der prävention der osteoporose bei postmenopausalen frauen. Dtsch Z Sportmed 57:182–188
Slatkovska L, Shabbir MH, Beyene J, Hu H, Demaras A, Cheung AM (2011) Effect of 12 months of whole-body vibration therapy on bone density and structure in postmenopausal women: a randomized trial. Ann Intern Med 155:668–679
Titze S, Ring-Dimitriou S, Schober P, Halbachs CGS, Miko H et al (2010) Österreichische Empfehlungen für gesundheitswirksame Bewegung. Eigenverlag, Wien
Tothill P, Hannan WJ (2007) Precision and accuracy of measuring changes in bone mineral density by dual-energy X-ray absorptiometry. Osteoporos Int 18:1515–1523. https://doi.org/10.1007/s00198-007-0382-4
Van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D et al (2012) Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value Sets. Value Health 15:708–715. https://doi.org/10.1016/j.jval.2012.02.008
Verschueren SM, Roelants M, Delecluse C, Swinnen S, Vanderschueren D, Boonen S (2004) Effect of 6-month whole body vibration training on hip density, muscle strength, and postural control in postmenopausal women: a randomized controlled pilot study. JBMR 19:352–359. https://doi.org/10.1359/JBMR.0301245
Von Stengel S, Kemmler W, Bebenek M, Engelke K (2011a) Effects of whole-body vibration training on different devices on bone mineral density. Med Sci Sports Exerc 43:1071–1079
Von Stengel S, Kemmler W, Engelke K, Kalender WA (2011b) Effects of whole body vibration on bone mineral density and falls: results of the randomized controlled ELVIS study with postmenopausal women. Osteoporos Int 22:317–325. https://doi.org/10.1007/s00198-010-1215-4
Wenger KH, Freeman JD, Fulzele S, Immel DM, Powell BD, Molitor P et al (2010) Effect of whole-body vibration on bone properties in aging mice. Bone 47:746–755. https://doi.org/10.1016/j.bone.2010.07.014
Wydra G (1993) Bedeutung, diagnose und therapie von gleichgewichtsstörungen. Motorik 3:100–107
Xie L, Jacobson JM, Choi ES, Busa B, Donahue LR, Miller LM et al (2006) Low-level mechanical vibrations can influence bone resorption and bone formation in the growing skeleton. Bone 39:1059–1066
Zha D-S, Zhu Q-A, Pei W-W, Zheng J-C, Wu S-H, Xu Z-X, Li T (2012) Does whole-body vibration with alternative tolting increase bone minareal density and change bone metabolism in senior people? Aging Clin Exp Res 24:28–36
Acknowledgements
The authors would like to thank all participating patients for making this study possible. A special thanks also goes to Dr. Tanja Seifen for performing the informed consent with all interested patients, as well as to Christoph Kneidinger, BSc., MSc for revising and preparing the study data collected by the University Institute of Nuclear Medicine and Endocrinology.
Funding
Open access funding provided by Paracelsus Medical University. This work was supported by the PMU Research Fund—PMU-FFF (T-17/05/001-LAN).
Author information
Authors and Affiliations
Contributions
YK, RS, HK, CP, and AW conceived, designed, and administered the project. TJ analyzed data. YK, RS, FR, JN, and TJ wrote the manuscript. All authors read, edited, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the State of Salzburg (E- 1145).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Olivier Seynnes.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
421_2022_5010_MOESM1_ESM.pdf
Supplemental material 1: Training program of the vibration and resistance training groups. Supplementary file1 (PDF 91 KB)
421_2022_5010_MOESM2_ESM.pdf
Supplemental material 2: Percentage of intensity of leisure activities per group at baseline. Supplementary file2 (PDF 83 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kienberger, Y., Sassmann, R., Rieder, F. et al. Effects of whole body vibration in postmenopausal osteopenic women on bone mineral density, muscle strength, postural control and quality of life: the T-bone randomized trial. Eur J Appl Physiol 122, 2331–2342 (2022). https://doi.org/10.1007/s00421-022-05010-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-022-05010-5