Abstract
Purpose
This study aimed to quantify sleeping heart rate (HR) and HR variability (HRV) alongside circulating tumor necrosis factor alpha (TNFα) concentrations during 12-week Basic Military Training (BMT). We hypothesised that, despite a high allostatic load, BMT would increase cardiorespiratory fitness and HRV, while lowering both sleeping HR and TNFα in young healthy recruits.
Methods
Sixty-three recruits (18–43 years) undertook ≥ 2 overnight cardiac frequency recordings in weeks 1, 8 and 12 of BMT with 4 h of beat-to-beat HR collected between 00:00 and 06:00 h on each night. Beat-to-beat data were used to derive HR and HRV metrics which were analysed as weekly averages (totalling 8 h). A fasted morning blood sample was collected in the equivalent weeks for the measurement of circulating TNFα concentrations and predicted VO2max was assessed in weeks 2 and 8.
Results
Predicted VO2max was significantly increased at week 8 (+ 3.3 ± 2.6 mL kg−1 min−1; p < 0.001). Sleeping HR (wk1, 63 ± 7 b min−1) was progressively reduced throughout BMT (wk8, 58 ± 6; wk12, 55 ± 6 b min−1; p < 0.01). Sleeping HRV reflected by the root mean square of successive differences (RMSSD; wk1, 86 ± 50 ms) was progressively increased (wk8, 98 ± 50; wk12, 106 ± 52 ms; p < 0.01). Fasted circulating TNFα (wk1, 9.1 ± 2.8 pg/mL) remained unchanged at wk8 (8.9 ± 2.5 pg/mL; p = 0.79) but were significantly reduced at wk12 (8.0 ± 2.4 pg/mL; p < 0.01).
Conclusion
Increased predicted VO2max, HRV and reduced HR during overnight sleep are reflective of typical cardiorespiratory endurance training responses. These results indicate that recruits are achieving cardiovascular health benefits despite the high allostatic load associated with the 12-week BMT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Measurement of heart rate (HR) and heart rate variability (HRV) responses are commonly employed as non-invasive surrogate assessments of cardiac autonomic modulation (Michael et al. 2017; Task Force 1996), often used to inform exercise training programs (Singh et al. 2018). Compared with untrained individuals, participation in cardiorespiratory endurance training has been associated with lower resting HR and increased HRV, indicative of stronger cardiac parasympathetic (vagal) autonomic modulation (Goldsmith et al. 1992; Seals and Chase 1985). In contrast, studies investigating exposure to prolonged high-volume cardiorespiratory endurance training demands or stressors such as compromised sleep, insufficient recovery, and fatigue often demonstrate reduced HRV, although findings are inconsistent (Meeusen et al. 2013; Westphal et al. 2021; Pichot et al. 2002). It is becoming increasingly recognised that HRV responses are dependent on a range of physiological and environmental factors which are difficult to control in applied research settings (Fatisson et al. 2016), likely influencing previous study outcomes.
The Australian Army Basic Military Training (BMT) program exposes a relatively homogenous group of recruits to controlled nutrition, psychological, physical,and military skills training designed to improve physical function and develop foundational military skills (Drain et al. 2017). An important component of the Australian Army BMT is the physical training program which consists of approximately 40 sessions. The focus of the physical training program is higher-intensity, lower-volume strength, and cardiorespiratory endurance training, with ~ 93% of sessions completed over the first 9 weeks of BMT on-barracks (Burley et al. 2020), before the 2-week field training phase. In addition to structured physical training and recovery, all participants are exposed to a prescribed sleep opportunity (‘lights out’ at 22:00 h and ‘wake up’ at 06:00 h) when in barracks. However, despite the primary objective of BMT, the physical and mental challenges when combined with inadequate periods of recovery lead to high allostatic stress that can undermine the rate of physiological adaptation (Drain et al. 2017). Accordingly, BMT offers a uniquely controlled setting in which to investigate HR and HRV responses to prolonged physical training and stress.
Previously, the root mean square of successive differences (RMSSD) of HR, a common HRV estimate of cardiac vagal autonomic modulation (Task Force 1996), has been demonstrated to increase following BMT (Grant et al. 2016) and more advanced military training courses (Jouanin et al. 2004) when analysed using waking short-term (5 min) recordings. While short-term and longer-term (e.g., 24 h) HRV recordings are widely used in non-clinical and clinical investigations, consideration needs to be given to the settings in which data are collected when interpreting HR and HRV (Kleiger et al. 2005), particularly in military populations (Hinde et al. 2021). For example, independent of environmental and behavioural changes, circadian rhythm influences cardiac autonomic modulation of HR to produce typical diurnal variability, whereby nadir occurs overnight alongside increased HRV, reflective of increased vagal autonomic activity (Furlan et al. 1990; Task Force 1996). Furthermore, night sleep is an important period for both physiological and psychological recovery (Brosschot et al. 2007) and HRV recording reliability may be enhanced with reduced influence from environmental factors (Pichot et al. 2000). Taking these issues into consideration, this study aimed to monitor HR and HRV during prescribed sleep opportunities (22:00–06:00 h) over the course of BMT as a practical and standardised approach in an applied military setting where day-to-day activities can vary substantially.
In addition to enhance cardiorespiratory fitness and cardiac physiological adaptations, participation in physical activity or exercise training is associated with a reduction in systemic inflammation (Lavie et al. 2011). However, the changes in pro-inflammatory cytokine markers, such as tumor necrosis factor α (TNFα), during and in response to BMT have been inconsistent, with several studies observing an increase (Booth et al. 2006; Gomez-Merino et al. 2003; Ojanen et al. 2018) while a more recent study has shown a decrease in TNFα at the completion of BMT (Tait et al. 2021). Recent evidence postulates that an increase in vagal nerve activity, which shares innervation to the gut and the spleen, may indirectly inhibit the release of circulating TNFα (Bonaz et al. 2016) and other specific inflammatory markers (Alen et al. 2021). Considering this postulation, increased HRV observed during BMT (Grant et al. 2016) could be further associated with a reduction in TNFα. However, the relationship between HRV, as a reflection of cardiac vagal modulation, and TNFα has yet to be investigated in young healthy adults.
The principle aim of this investigation was to quantify sleeping HR and the well-established vagally mediated HRV metric of RMSSD in recruits, during prescribed overnight sleep opportunities, throughout BMT. The primary hypothesis was that overnight sleeping HR would be reduced and RMSSD would be increased alongside improvements in cardiorespiratory fitness as a result of 12-week BMT. A secondary aim was to examine the association between fasted morning circulating TNFα concentrations and vagally mediated RMSSD. Finally, a number of less-established HRV metrics were included for exploratory analyses.
Materials and methods
Experimental overview
This study collected data during a 12-week BMT program and was part of a larger project designed to quantify training loads and monitor the physiological and psychological responses of recruits during BMT, the experimental procedures and results of which have been published previously (Larsen et al. 2022). All recruits completed identical training syllabuses that included orientation, progressive physical training (40 sessions) and military skills (weeks 1–9), field training (weeks 10–11), and ceremonial preparations and March out (week 12) as previously described (Larsen et al. 2022). The typical training day (06:00–22:00 h) in the first nine weeks included supervised physical training and military education sessions in that order. Week 1 represents baseline data, week 8 represents the end of prescribed physical training and week 12 represents the end of BMT. Overnight cardiac frequency monitoring was initiated in week 1 following the provision of consent and recruits’ initial medical assessment. For week 12, data were recorded across 3 nights due to preparation for the march out parade. In addition, finger prick blood samples were collected in a fasted state upon wakening at the commencement of BMT (week 1), week 8 and week 12 of training to assess changes in circulating TNFα concentrations. Cardiorespiratory physical fitness was assessed via multi-stage shuttle test performance during weeks 2 and 8 of BMT.
Participants
One hundred male and female recruits (18–43 years) volunteered to participate in the study in which 63 recruits (males: n = 55, females n = 8; 23 ± 5 years; 76.8 ± 14.0 kg; 24.3 ± 3.4 kg m−2) met the inclusion criteria; i.e., ≥ 2 overnight sleep recordings with a minimum 4 h of continuous RR-interval data collected between 00:00 and 06:00 h in week 1, 8 and 12 of BMT, and completed BMT within the scheduled 12 weeks. The remaining 37 recruits were excluded from the current study due to withdrawal of consent, delayed training schedule (e.g., injury or inability to meet training standards), discharged from training, or failure to meet inclusion criteria. Recruits were from three platoons that commenced training in August and September, 2019, at the Army Recruit Training Centre, Kapooka (Australia). The study procedures and risks were explained verbally and provided in writing to each recruit before they provided written informed consent. The study was approved by the Department of Defence and Veterans’ Affairs Human Research Ethics Committee (protocol number: 083-18).
Heart rate and HRV measurement
Overnight cardiac frequency was recorded using electrocardiographic chest-strap HR monitors, with the RR-interval data recordings downloaded from the devices and imported to the Polar Team2 System (Polar Electro Oy, Kempele, Finland). The RR-intervals were then exported into Kubios software for subsequent analysis (Tarvainen et al. 2014). All files were passed through an automatic noise detection filter and artefact correction algorithm (Lipponen and Tarvainen 2019) which removed artefacts due to ectopic beats, missed beats etc. Artefacts were replaced using cubic spline interpolation leaving only physiologically normal-to-normal interval (NN-interval) time series before HRV analysis was completed. With the use of the NN-interval time series of each participant, absolute HR and HRV data were calculated as weekly averages using a 4-h window collected between 24:00 and 06:00 h from the same two nights (totaling 8 h from each weekly time point). In the majority of participants, data was collected from 24:00 to 04:00 to reduce the influence of the initial stages of sleep and awakening. When a file had > 5% of the total beats corrected (AVG, 1.1%; SD, ± 0.9%), visual evidence of sleep disturbances or an incomplete overnight recording that prohibited analysis of a 4-h window, it was not included in the analysis and replaced with a file from the night before/after.
HRV metrics were computed using time, frequency and non-linear domains. The study investigated RMSSD of NN-intervals as the most established HRV metric reflecting vagal modulation of HR (Task Force 1996). RMSSD was also investigated following correction for HR—by division of RMSSD by average NN-interval to the power 4 (Sacha et al. 2013). In addition, the low frequency (LF, 0.04–0.15 Hz), high frequency (HF, 0.15–0.4 Hz), LF/HF ratio, sample entropy (SampEn), approximate entropy (ApEn) along with both the short-term detrended fluctuation analysis alpha-1 (DFAα1) and long-term alpha-2 (DFAα2) scaling exponents were included for further exploratory analyses. Power spectra were calculated by means of fast Fourier transformation. The European Heart Rhythm Association (EHRA) HRV signal analysis position paper provides further clarification of the HRV metrics reported in this study (Sassi et al. 2015).
Tumor necrosis factor α (TNFα) measurement
Blood sample collection was performed using the finger prick method in a fasting state (between 06:00 and 07:00 h). In brief, the hand of each recruit was warmed using gloves and the finger was cleaned using an alcohol swab. A 21-G lancet (Sarstedt, Germany) puncture enabled the finger to bleed freely and enough volume was collected to fill a 300 µL tube treated with lithium heparin (Sarstedt, Germany). Samples were centrifuged at 4000 rpm for 5 min at 4 °C. Plasma obtained was stored at − 80 °C and later analysed independently by a registered laboratory. Samples were analysed in duplicate using a High Sensitive T Cell Cytokine Panel (HSTCMAG-28SK, Milliplex, Merck) to provide raw values for circulating TNFα. Results dropping below the detection threshold were allocated the value for the assay’s minimum detectable limit (TNFα: 0.16 pg/mL). Analyses had an intra-assay percent coefficient of variation (%CV) of < 6% and an inter-assay %CV of < 20%.
Cardiorespiratory physical fitness
Cardiorespiratory physical fitness was assessed via multi-stage shuttle test performance during weeks 2 and 8 of BMT. Performance scores in the multi-stage shuttle test were used to predict VO2max according to Ramsbottom et al. (1988).
Statistical analysis
Prior to statistical analysis, the distribution of continuous data was analysed for normality using the D’Agostino–Pearson omnibus (K2) test and homogeneity of variances was confirmed via Brown–Forsythe test. As RMSSD was not normally distributed, natural logarithmic transformed observations were analysed, and these were normally distributed. A paired t test was used to compare differences in VO2max at week 2 and week 8. A repeated measures one-way analysis of variance (ANOVA) was used to compare differences between BMT weeks for HR and HRV metrics recorded during overnight sleep. Tukey’s post hoc tests were applied to identify where any significant differences occurred. A mixed-effects model was used to compare differences between BMT weeks for circulating TNFα concentrations and Pearson’s correlation analysis was used to investigate associations with RMSSD in a subset of the recruits at weeks 1 (n = 50), 8 (n = 28) and 12 (n = 39). Data are presented as mean (95% CI) unless otherwise stated and statistical significance was accepted at p ≤ 0.05. Statistical analyses were completed in GraphPad Prism (v9, GraphPad Software, USA).
Results
Cardiorespiratory physical fitness
At week 2, predicted VO2max of participants was 42.5 ± 3.8 (mL kg−1 min−1). The multi-stage shuttle test conducted at weeks 2 and 8 demonstrated a significant increase in predicted VO2max (+ 3.3 ± 2.6 mL kg−1 min−1; p < 0.001).
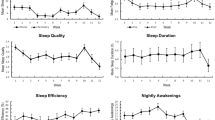
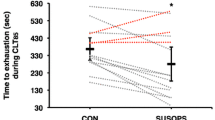
Heart rate, RMSSD and TNFα
The average overnight sleeping HR progressively reduced (p < 0.001) throughout BMT (Fig. 1a, b). More specifically, average overnight sleeping HR was 5 b min−1 slower at week 8, relative to week 1 and further reduced by 3 b min−1 at week 12, relative to week 8. Average overnight sleeping RMSSD progressively increased (p < 0.001) throughout BMT (Fig. 2a, b); however, when RMSSD was corrected for underlying HR it was observed to be progressively lower (Fig. 2c). Circulating TNFα concentrations remained unchanged at week 8 but were significantly reduced at week 12 (Fig. 3a). No correlations were observed between RMSSD and TNFα at week 1 (Pearson r = − 0.022; p = 0.88), week 8 (Pearson r = 0.021; p = 0.92) or week 12 (Fig. 3b; Pearson r = − 0.019; p = 0.25). Likewise, no evidence of a relationship was observed when RMSSD and TNFα were assessed as a relative change between weeks 1 and 8 (Pearson r = − 0.314; p = 0.11), 1 and 12 (Pearson r = − 0.265; p = 0.10) or between weeks 8 and 12 (Pearson r = 0.292; p = 0.12).
a Time-course changes in group mean (± 95% CI) overnight sleeping heart rate collected in participants (n = 63) during 12-week Basic Military Training. b Changes in overnight sleeping heart rate from week 1 (dashed line). Each individual response is plotted along with the group mean ± 95% CI (solid black line). Data analysed using a one-way repeated measures ANOVA with Tukey’s multiple comparisons test. ****p < 0.0001. b min−1, beats per minute
a Time-course changes in group mean (± 95% CI) overnight sleeping RMSSD collected in participants (n = 63) during 12-week Basic Military Training. b Changes in overnight sleeping RMSSD from week 1 (dashed line). Each individual response is plotted along with the group mean ± 95% CI (solid black line). c Time-course changes in group mean (± 95% CI) HR corrected overnight sleeping RMSSD. RMSSD is presented using msec for ease of physiological interpretation but was analysed after natural logarithmic transformation to achieve normal distribution. Data analysed using a one-way repeated measures ANOVA with Tukey’s multiple comparisons test. ****p < 0.0001; ***p < 0.001; *p < 0.05. RMSSD, root mean square of successive differences; HR, heart rate
a Time-course changes in group mean (± 95% CI) circulating morning TNFα concentrations collected in participants (week 1: n = 50; week 8: n = 28; week 12: n = 39) during 12-week Basic Military Training. Data analysed using a mixed-effects model with Tukey’s multiple comparisons test. ***p < 0.001; ns, not significant. b Correlation between change in RMSSD and TNFα between week 1 and 12 of Basic Military Training in a subset of the recruits. Each individual response is plotted on the graph and a simple linear regression line of best fit (solid black line) has been fitted to the data with Pearson r and two-tailed p value displayed. RMSSD, root mean square of successive differences; TNFα, tumor necrosis factor alpha
Other HRV metrics
Frequency domain LF and HF power during week 8 remained unchanged from week 1. However, LF and HF power had increased significantly (p < 0.001) during week 12, relative to both week 1 and week 8 (Table 1). The average overnight sleeping LF:HF power ratio was significantly (p < 0.001) reduced at weeks 8 and 12 compared to week 1, with no differences observed between weeks 8 and 12 (Table 1). Relative to week 1, the average overnight sleeping non-linear domain HRV metrics ApEn and SampEn were significantly (p < 0.001) increased at weeks 8 and 12, with no further differences observed between weeks 8 and 12 (Table 1). Finally, the average overnight sleeping DFAα1 and α2 were significantly (p < 0.001) reduced at both week 8s and 12 compared to week 1 but no further significant decreases were observed between weeks 8 and 12 (Table 1).
Discussion
In alignment with our primary hypothesis, this study demonstrates for the first time, that an intensive 12-week BMT program increased vagally mediated RMSSD and slowed HR during overnight sleep. Exploratory analyses of less-established HRV metrics collected from the frequency domain (e.g., HF power and the LF:HF ratio) provided further evidence of increased vagal activity. These changes, typically observed alongside enhanced cardiorespiratory fitness (Goldsmith et al. 1992), were still evident despite the high allostatic stress experienced during BMT (Drain et al. 2017). However, in this apparently healthy cohort, no correlation was evident between fasted morning circulating TNFα concentrations, which also reduced over time, and RMSSD, a HRV estimate of cardiac vagal autonomic modulation (Task Force 1996). The unique observations from this study indicate that the BMT program provides suitable physical and cognitive stressors that, at a group level, are strong enough to promote increases in vagally mediated RMSSD and slow overnight sleeping HR whilst also conveying a small yet vagally independent reduction of TNFα, reflecting lowered inflammatory status.
The primary outcome from the current study was the progressive increases in the well-established vagally mediated HRV metric of RMSSD throughout 12 weeks of BMT in these young and healthy participants. In alignment, HF power, a frequency domain metric reflective of vagal activity, was significantly increased in week 12 and predominantly responsible for driving the observed reduction in the LF:HF power ratio. This observation contrasts with findings from previous studies demonstrating that in otherwise healthy individuals, prolonged high-volume training demands and/or additional stressors, including compromised sleep, insufficient recovery, and fatigue, are associated with mixed HRV outcomes (Meeusen et al. 2013; Westphal et al. 2021; Pichot et al. 2002). The differing results may be explained by the volume and intensity of the physical training prescribed which significantly increased cardiorespiratory fitness by 7% at week 8. Further, although the novel BMT program that recruits completed in the current study includes training activities that are physically and cognitively challenging, it primarily prescribes low-moderate intensity physical activity with intermittent periods of high-intensity exercise (Burley et al. 2020), whereas traditional military physical training programs have emphasised high-volume cardiorespiratory and muscular endurance activities (Kyröläinen et al. 2018). Nevertheless, Grant et al. (2016) and Jouanin et al. (2004) demonstrated similar effects on short-term (5 min) awake recordings of HRV metrics reflecting cardiac vagal modulation; we support and strengthen these observations by monitoring during prescribed overnight sleep opportunities incorporating the nadir HR.
In line with the primary HRV outcome of the study, on average a progressive 8 b min−1 slowing of overnight sleeping HR was observed at week 12 of BMT. This 12% reduction is consistent with typical effects of endurance training on heart rhythm between an ‘untrained’ and a ‘trained’ group (Goldsmith et al. 1992). However, there were a small number of recruits amongst the cohort in which sleeping HR remained stable or slightly increased (Fig. 1b). Similar observations have been made previously, whereby nocturnal HRV increased in most but not all individuals subjected to four weeks of endurance training (Nummela et al. 2016). It is likely the non-response is explained, at least in part by a higher training status prior to commencing BMT (Pickering and Kiely 2019), individual fluctuation of HR and HRV related to sleep or other overnight disturbance (Hinde et al. 2021), or human variance in response to exercise training and highlights the importance of future studies considering precision exercise medicine to promote uniform responses (Ross et al. 2019). Nonetheless, slowing of resting HR is most commonly attributed to increased vagal tone, particularly in studies investigating exercise training induced resting bradycardia (Coote and White 2015). However, the decline observed in resting HR could be explained by additional contributory factors, other than exclusively a change in vagal tone. Indeed, direct intrinsic adaptations within myocardial tissue are known to promote a resting bradycardia (Boyett et al. 2017). Our results with respect to entropy and RMSSD (corrected for underlying HR) support the notion that intrinsic factors may have also contributed to the decline in resting HR (Boyett et al. 2013). Entropy is a measure of the degree of irregularity or the likelihood that successive RR intervals will repeat themselves, with greater values thought to indicate increased complexity of the physiological processes underlying the control of HR (Pincus and Goldberger 1994). We observed in our investigation a significantly increased entropy at week 8 of BMT. Similarly, with respect to RMSSD corrected for underlying HR, we demonstrated that vagally mediated RMSSD was proportionally decreased at each time point. Whilst debate exists as to whether HRV is a valid measure of cardiac autonomic modulation or is primarily a non-linear surrogate of HR itself (Boyett et al. 2019; Malik et al. 2019; Macartney et al. 2021), these results suggest progressive and proportional reductions in vagal modulation when RMSSD is normalised to HR. When taken together, the HR corrected results in combination with measures of entropy appear to support the notion of direct intrinsic adaptations of the cardiac tissue contributing towards exercise induced resting bradycardia (Boyett et al. 2013). Thus, an adaptive interplay of neural (vagal) modulation and structural changes to cardiac tissue may collectively be responsible for the observed decline in HR; however, the answer to this question is outside the scope of the current study. Irrespective of mechanism, the observed reduction in HR during extended periods of sleep in these recruits conveys an ivabradine like effect on coronary artery perfusion (increased) which occurs primarily during diastole (Heusch 2008).
Interestingly, in the current study, despite significantly reduced mean circulating TNFα concentrations at week 12 and progressive increases in RMSSD, no correlations between these measures were observed at any of the time points during BMT. There are several possible reasons for this. Firstly, chronic systemic inflammation is predominantly observed in individuals pushed routinely to the limits of their physical capabilities combined with insufficient recovery (Carfagno and Hendrix 2014). It is unlikely that the stressors within the BMT program are strenuous enough over the 12 weeks to stimulate such an inflammatory response. In fact, the BMT program has recently been demonstrated to cause minimal perturbation to inflammatory markers (Tait et al. 2021). Second, RMSSD is a surrogate measure of vagal activity upon sino-atrial nodal tissue (Gourine and Ackland 2019). Accordingly, increases in RMSSD may not directly translate to increased vagal nerve activity by the multi-synaptic interaction between the vagus and the splanchnic nerves (Bassi et al. 2020) modulating splenic macrophage TNFα release (Bonaz et al. 2016; Alen et al. 2021). Finally, high inflammatory states are commonly observed in older (Alen et al. 2021) or cardiometabolic chronic disease cohorts with elevated resting HR (Osborn and Olefsky 2012). In combination, these data lead us to reject the postulation that an increase in HRV, as a reflection of cardiac specific vagal nerve activity, may be associated with indirect inhibition of the release of circulating TNFα in young and healthy individuals.
The reduction observed in this study of overnight sleeping DFAα1 away from 1.0 was also noteworthy. This metric of fractal complexity is quantified using values from 0.5 to 1.5, with lower values indicating more random and higher values indicating more correlated interbeat variability behaviour, and a value of approximately 1.0 signifying a balance between random and predictable (self-similar) interbeat behaviour (Peng et al. 1995). In healthy individuals, relative to their awake measurements, DFAα1 has been demonstrated to be increased during REM sleep but reduced during light sleep with a further reduction during deep sleep (Penzel et al. 2003; Bunde et al. 2000). Accordingly, the lower sleeping DFAα1 values observed during week 8 and 12 within the current study may well indicate a shift in sleep patterns towards predominantly deep sleep. However, this point is rather speculative as it has been acknowledged that further work is needed to understand the link between sleep stage and heart rhythm (Penzel et al. 2003).
In conclusion, the current study reveals that 12-weeks of BMT in Army recruits increases vagally mediated RMSSD and slows HR during overnight sleep with an eventual reduction on circulating TNFα concentrations. These results indicate that, on average, recruits are achieving cardiovascular and inflammatory health benefits despite experiencing cumulative stressors associated with the Australian Army 12-week BMT course. However, it was evident that a small number of individuals did not respond in alignment with the group and further research is necessary to identify the potential contributing factors (e.g., nutrition, hydration, psychological) at an individual level. This highlights the need to engage further with understanding human physiological variation (Tipton et al. 2021) in response to multi-stressor environments such as BMT. Nevertheless, the homogenous young and healthy group used in the study, alongside prescribed overnight sleep opportunities and the tightly controlled nature of a military training environment make these findings particularly novel relative to other less controlled applied settings. Lower resting HR and increased HRV are strongly associated with superior exercise capacity (Gourine and Ackland 2019), maintenance of which is essential for well-being and optimal cardiac health outcomes across a lifespan, and for promoting career longevity in military recruits.
Availability of data and materials
Data will be made available upon request to the corresponding author.
Abbreviations
- ANOVA:
-
Analysis of variance
- ApEn:
-
Approximate entropy
- b min− 1 :
-
Beats per minute
- BMT:
-
Basic military training
- DFA:
-
Detrended fluctuation analysis
- HF:
-
High frequency
- HR:
-
Heart rate
- HRV:
-
Heart rate variability
- LF:
-
Low frequency
- ms:
-
Milliseconds
- RMSSD:
-
Root mean square of successive differences
- SampEn:
-
Sample entropy
- TNFα:
-
Tumor necrosis factor alpha
- VO2max:
-
Maximal oxygen consumption
References
Alen NV, Parenteau AM, Sloan RP, Hostinar CE (2021) Heart rate variability and circulating inflammatory markers in midlife. Brain Behav Immunity-Health 15:100273
Bassi GS, Kanashiro A, Coimbra NC, Terrando N, Maixner W, Ulloa L (2020) Anatomical and clinical implications of vagal modulation of the spleen. Neurosci Biobehav Rev 112:363–373. https://doi.org/10.1016/j.neubiorev.2020.02.011
Bonaz B, Sinniger V, Pellissier S (2016) Anti-inflammatory properties of the vagus nerve: potential therapeutic implications of vagus nerve stimulation. J Physiol 594(20):5781–5790. https://doi.org/10.1113/jp271539
Booth CK, Probert B, Forbes-Ewan C, Coad RA (2006) Australian Army recruits in training display symptoms of overtraining. Mil Med 171(11):1059–1064. https://doi.org/10.7205/milmed.171.11.1059
Boyett MR, D’Souza A, Zhang H, Morris GM, Dobrzynski H, Monfredi O (2013) Viewpoint: Is the resting bradycardia in athletes the result of remodeling of the sinoatrial node rather than high vagal tone? J Appl Physiol 114(9):1351–1355. https://doi.org/10.1152/japplphysiol.01126.2012
Boyett MR, Wang Y, Nakao S, Ariyaratnam J, Hart G, Monfredi O, D’Souza A (2017) Point: Exercise training-induced bradycardia is caused by changes in intrinsic sinus node function. J Appl Physiol 123(3):684–685. https://doi.org/10.1152/japplphysiol.00604.2017
Boyett M, Wang Y, D’Souza A (2019) CrossTalk opposing view: heart rate variability as a measure of cardiac autonomic responsiveness is fundamentally flawed. J Physiol 597(10):2599–2601. https://doi.org/10.1113/jp277501
Brosschot JF, Van Dijk E, Thayer JF (2007) Daily worry is related to low heart rate variability during waking and the subsequent nocturnal sleep period. Int J Psychophysiol 63(1):39–47. https://doi.org/10.1016/j.ijpsycho.2006.07.016
Bunde A, Havlin S, Kantelhardt JW, Penzel T, Peter J-H, Voigt K (2000) Correlated and uncorrelated regions in heart-rate fluctuations during sleep. Phys Rev Lett 85(17):3736–3739. https://doi.org/10.1103/PhysRevLett.85.3736
Burley SD, Drain JR, Sampson JA, Nindl BC, Groeller H (2020) Effect of a novel low volume, high intensity concurrent training regimen on recruit fitness and resilience. J Sci Med Sport 23(10):979–984
Carfagno DG, Hendrix JC (2014) Overtraining syndrome in the athlete: current clinical practice. Curr Sports Med Rep 13(1):45–51
Coote JH, White MJ (2015) CrossTalk proposal: bradycardia in the trained athlete is attributable to high vagal tone. J Physiol 593(Pt 8):1745–1747. https://doi.org/10.1113/jphysiol.2014.284364
Drain JR, Groeller H, Burley SD, Nindl BC (2017) Hormonal response patterns are differentially influenced by physical conditioning programs during basic military training. J Sci Med Sport 20:S98–S103. https://doi.org/10.1016/j.jsams.2017.08.020
Fatisson J, Oswald V, Lalonde F (2016) Influence diagram of physiological and environmental factors affecting heart rate variability: an extended literature overview. Heart Int 11(1):5000232
Task Force (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 93:1043–1065. https://doi.org/10.1161/01.CIR.93.5.1043
Furlan R, Guzzetti S, Crivellaro W, Dassi S, Tinelli M, Baselli G, Cerutti S, Lombardi F, Pagani M, Malliani A (1990) Continuous 24-hour assessment of the neural regulation of systemic arterial pressure and RR variabilities in ambulant subjects. Circulation 81(2):537–547
Goldsmith RL, Bigger JT Jr, Steinman RC, Fleiss JL (1992) Comparison of 24-hour parasympathetic activity in endurance-trained and untrained young men. J Am Coll Cardiol 20(3):552–558. https://doi.org/10.1016/0735-1097(92)90007-a
Gomez-Merino D, Chennaoui M, Burnat P, Drogou C, Guezennec CY (2003) Immune and hormonal changes following intense military training. Mil Med 168(12):1034–1038. https://doi.org/10.1093/milmed/168.12.1034
Gourine AV, Ackland GL (2019) Cardiac vagus and exercise. Physiology 34(1):71–80. https://doi.org/10.1152/physiol.00041.2018
Grant CC, Mongwe L, Janse van Rensburg DC, Fletcher L, Wood PS, Terblanche E, du Toit PJ (2016) The difference between exercise-induced autonomic and fitness changes measured after 12 and 20 weeks of medium-to-high intensity military training. J Strength Cond Res 30(9):2453–2459. https://doi.org/10.1519/JSC.0b013e3182a1fe46
Heusch G (2008) Heart rate in the pathophysiology of coronary blood flow and myocardial ischaemia: benefit from selective bradycardic agents. Br J Pharmacol 153(8):1589–1601. https://doi.org/10.1038/sj.bjp.0707673
Hinde K, White G, Armstrong N (2021) Wearable devices suitable for monitoring twenty four hour heart rate variability in military populations. Sensors. https://doi.org/10.3390/s21041061
Jouanin JC, Dussault C, Pérès M, Satabin P, Piérard C, Guézennec CY (2004) Analysis of heart rate variability after a ranger training course. Mil Med 169(8):583–587. https://doi.org/10.7205/milmed.169.8.583
Kleiger RE, Stein PK, Bigger JT Jr (2005) Heart rate variability: measurement and clinical utility. Ann Noninvasive Electrocardiol 10(1):88–101. https://doi.org/10.1111/j.1542-474X.2005.10101.x
Kyröläinen H, Pihlainen K, Vaara JP, Ojanen T, Santtila M (2018) Optimising training adaptations and performance in military environment. J Sci Med Sport 21(11):1131–1138
Larsen P, Drain J, Gibson N, Sampson J, Michael S, Peoples G, Groeller H (2022) Chronicity of sleep restriction during Army basic military training. J Sci Med Sport. https://doi.org/10.1016/j.jsams.2022.01.008
Lavie CJ, Church TS, Milani RV, Earnest CP (2011) Impact of physical activity, cardiorespiratory fitness, and exercise training on markers of inflammation. J Cardiopulm Rehabil Prev 31(3):137–145
Lipponen JA, Tarvainen MP (2019) A robust algorithm for heart rate variability time series artefact correction using novel beat classification. J Med Eng Technol 43(3):173–181. https://doi.org/10.1080/03091902.2019.1640306
Macartney MJ, McLennan PL, Peoples GE (2021) Heart rate variability during cardiovascular reflex testing: the importance of underlying heart rate. J Basic Clin Physiol Pharmacol 32(3):145–153. https://doi.org/10.1515/jbcpp-2020-0245
Malik M, Hnatkova K, Huikuri HV, Lombardi F, Schmidt G, Zabel M (2019) CrossTalk proposal: heart rate variability is a valid measure of cardiac autonomic responsiveness. J Physiol 597(10):2595–2598. https://doi.org/10.1113/jp277500
Meeusen R, Duclos M, Foster C, Fry A, Gleeson M, Nieman D, Raglin J, Rietjens G, Steinacker J, Urhausen A (2013) Prevention, diagnosis, and treatment of the overtraining syndrome: joint consensus statement of the European College of Sport Science and the American College of Sports Medicine. Med Sci Sports Exerc 45(1):186–205. https://doi.org/10.1249/MSS.0b013e318279a10a
Michael S, Graham KS, Davis GM (2017) Cardiac autonomic responses during exercise and post-exercise recovery using heart rate variability and systolic time intervals—a review. Front Physiol. https://doi.org/10.3389/fphys.2017.00301
Nummela A, Hynynen E, Kaikkonen P, Rusko H (2016) High-intensity endurance training increases nocturnal heart rate variability in sedentary participants. Biol Sport 33(1):7–13. https://doi.org/10.5604/20831862.1180171
Ojanen T, Jalanko P, Kyröläinen H (2018) Physical fitness, hormonal, and immunological responses during prolonged military field training. Physiol Rep 6(17):e13850. https://doi.org/10.14814/phy2.13850
Osborn O, Olefsky JM (2012) The cellular and signaling networks linking the immune system and metabolism in disease. Nat Med 18(3):363–374. https://doi.org/10.1038/nm.2627
Peng CK, Havlin S, Stanley HE, Goldberger AL (1995) Quantification of scaling exponents and crossover phenomena in nonstationary heartbeat time series. Chaos 5(1):82–87. https://doi.org/10.1063/1.166141
Penzel T, Kantelhardt JW, Grote L, Peter JH, Bunde A (2003) Comparison of detrended fluctuation analysis and spectral analysis for heart rate variability in sleep and sleep apnea. IEEE Trans Biomed Eng 50(10):1143–1151. https://doi.org/10.1109/TBME.2003.817636
Pichot V, Roche F, Gaspoz J-M, Enjolras F, Antoniadis A, Minini P, Costes F, Busso T, Lacour J-R, Barthelemy JC (2000) Relation between heart rate variability and training load in middle-distance runners. Med Sci Sports Exerc 32(10):1729–1736
Pichot V, Busso T, Roche F, Garet M, Costes F, Duverney D, Lacour JR, Barthélémy JC (2002) Autonomic adaptations to intensive and overload training periods: a laboratory study. Med Sci Sports Exerc 34(10):1660–1666. https://doi.org/10.1097/00005768-200210000-00019
Pickering C, Kiely J (2019) Do non-responders to exercise exist—and if so, what should we do about them? Sports Med 49(1):1–7. https://doi.org/10.1007/s40279-018-01041-1
Pincus SM, Goldberger AL (1994) Physiological time-series analysis: what does regularity quantify? Am J Physiol 266(4 Pt 2):H1643-1656. https://doi.org/10.1152/ajpheart.1994.266.4.H1643
Ramsbottom R, Brewer J, Williams C (1988) A progressive shuttle run test to estimate maximal oxygen uptake. Br J Sports Med 22(4):141–144
Ross R, Goodpaster BH, Koch LG, Sarzynski MA, Kohrt WM, Johannsen NM, Skinner JS, Castro A, Irving BA, Noland RC, Sparks LM, Spielmann G, Day AG, Pitsch W, Hopkins WG, Bouchard C (2019) Precision exercise medicine: understanding exercise response variability. Br J Sports Med 53(18):1141–1153. https://doi.org/10.1136/bjsports-2018-100328
Sacha J, Barabach S, Statkiewicz-Barabach G, Sacha K, Müller A, Piskorski J, Barthel P, Schmidt G (2013) How to strengthen or weaken the HRV dependence on heart rate–description of the method and its perspectives. Int J Cardiol 168(2):1660–1663. https://doi.org/10.1016/j.ijcard.2013.03.038
Sassi R, Cerutti S, Lombardi F, Malik M, Huikuri HV, Peng CK, Schmidt G, Yamamoto Y (2015) Advances in heart rate variability signal analysis: joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Europace 17(9):1341–1353. https://doi.org/10.1093/europace/euv015
Seals DR (1985) Chase PB (1989) Influence of physical training on heart rate variability and baroreflex circulatory control. J Appl Physiol 66(4):1886–1895. https://doi.org/10.1152/jappl.1989.66.4.1886
Singh N, Moneghetti KJ, Christle JW, Hadley D, Froelicher V, Plews D (2018) Heart rate variability: an old metric with new meaning in the era of using mhealth technologies for health and exercise training guidance. Part two: prognosis and training. Arrhythm Electrophysiol Rev 7(4):247–255. https://doi.org/10.15420/aer.2018.30.2
Tait JL, Bulmer S, Drain JR, Main LC (2021) Associations between inflammatory markers and well-being during 12 weeks of basic military training. Eur J Appl Physiol 121(3):849–860. https://doi.org/10.1007/s00421-020-04554-8
Tarvainen MP, Niskanen J-P, Lipponen JA, Ranta-Aho PO, Karjalainen PA (2014) Kubios HRV–heart rate variability analysis software. Comput Methods Programs Biomed 113(1):210–220
Tipton MJ, Corbett J, Eglin CM, Mekjavic IB, Montgomery H (2021) In pursuit of the unicorn. Exp Physiol 106(2):385–388. https://doi.org/10.1113/EP089147
Westphal W-P, Rault C, Robert R, Ragot S, Neau J-P, Fernagut P-O, Drouot X (2021) Sleep deprivation reduces vagal tone during an inspiratory endurance task in humans. Sleep. https://doi.org/10.1093/sleep/zsab105
Acknowledgements
We are extremely grateful to the Australian Army recruits who participated in the study and the staff at the Army Recruit Training Centre for their support to facilitate this investigation.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. Research reported in this publication was supported by the Defence Science and Technology Group by a Defence Science Partnering Deed #7081.
Author information
Authors and Affiliations
Contributions
HG, SM, GP contributed to the study conception and design. Material preparation, data collection and analysis were primarily performed by MM, SM and PL. The first draft of the manuscript was written by MM and all authors commented on previous versions of the manuscript. All authors have read and approved the final version of this manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All persons designated as authors qualify for authorship, and all those who qualify for authorship are listed.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent to participate
The study procedures and risks were explained verbally and provided in writing to each recruit before they provided written informed consent.
Ethics approval
The study was approved by the Department of Defence and Veterans’ Affairs Human Research Ethics Committee (protocol number: 083-18).
Additional information
Communicated by William J. Kraemer.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Macartney, M.J., Larsen, P., Gibson, N. et al. Overnight sleeping heart rate variability of Army recruits during a 12-week basic military training course. Eur J Appl Physiol 122, 2135–2144 (2022). https://doi.org/10.1007/s00421-022-04987-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-022-04987-3